Acute Kidney Injury toolkit
AKI: Recognition and response
The NCEPOD report Adding Insult to Injury identified failings in recognition, investigation and management of patients with AKI. There is evidence that illness complicated by AKI is associated with:
- High mortality - over 20% of patients with AKI in hospital die during admission
- Increased length of hospital stay and utilisation of NHS resources
- Incomplete recovery of kidney function with many patients developing new or worsening chronic kidney disease (CKD)
Recognising and responding to AKI warning stage test results for adults in primary care
The presence of AKI is determined using internationally recognised criteria that are based on individualised changes in serum creatinine concentration with respect to that person’s usual (or baseline) value, and/or reduction in urine volume (see Think Kidneys guidance for primary care).
Primary care teams should prioritise early AKI detection because:
- In approximately two thirds of cases AKI begins in the community
- AKI is associated with poor outcomes, even for patients who are not admitted to hospital.
Strategies to expedite AKI recognition and response should include:
- Prompting AKI awareness and risk reduction strategies among patients and healthcare staff, because AKI often begins without symptoms specific to AKI
- Maintaining a low threshold to perform blood tests to check kidney function if “at risk” patients become unwell
- Timely review of patients whose blood results trigger AKI warning stage alerts* in order to interpret the test result in clinical context.
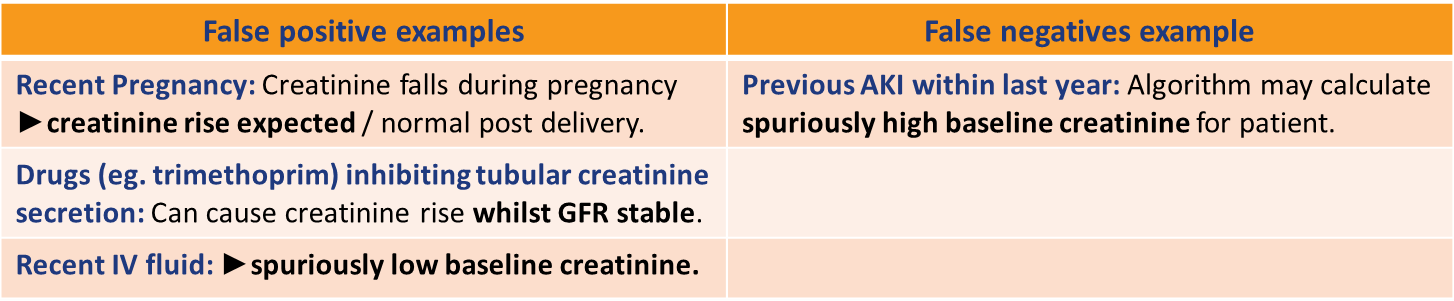
* NHS England has mandated that UK laboratories present AKI Warning Stage alerts alongside renal blood results, when potentially significant creatinine changes are identified. This system aims to highlight potential AKI cases promptly. The national AKI algorithm employs computer-based comparison of serial blood results and is unable to incorporate clinical context into assignment of AKI Warning Stage Test results. It is therefore imperative that clinical teams do not “rely” upon this system to accurately identify all AKI cases, as false positives and false negatives can occur if blood results are interpreted without clinical correlation. Although AKI Warning Stage alerts will help highlight most AKI cases, an overarching principal should be to “treat the patient not the test result”. Think Kidneys has published resources to support such timely validation and response to AKI warning alerts, tailored to primary care teams.
Table 1: Recommended response times to AKI Warning Stage Test Results for adults in primary care
Key questions when responding to an AKI Warning Stage Test Result:
Why was the blood test taken?
Clinical context at time of venesection influences the pre-test probability of the AKI Warning Stage Test Result:
- Routine chronic disease monitoring or drug monitoring? (Yes = AKI less likely)
- Assessment of acute illness? (Yes = AKI more likely)
It is good practice for primary care teams to implement processes to enable the person reviewing blood results to know “why” the test was taken, especially if 1) AKI was suspected; or 2) the blood results are likely to be sent to “Out of Hours” services. Enriching Summary Care Records can help better information exchange. Auditing response to AKI Warning Stage Test Results as well as conducting AKI case note reviews may support the development of a protocol for ensuring a safe and reliable system for managing tests.
Is this a true case of AKI?
AKI Warning Stage Test Results reflect changes in creatinine over time. Review of the clinical context and comparison with the patient’s baseline creatinine is necessary to decide if the patient with a warning stage test result does indeed have AKI. Consider:
- Is the patient acutely unwell? (If yes = AKI is more likely)
- Is the patient known to have chronic kidney disease (CKD) and is the change in creatinine due to progression of CKD rather than an acute change? (Particularly consider this if the baseline creatinine values are ≥ 12 months old; look at the serum creatinine values over a longer period of time to ascertain better the patients' baseline)
- Are there any other issues that might underlie a false positive result (table below)?
If still in doubt (and the patient is well) consider repeating the creatinine within 48-72hrs which will help determine whether the changes are dynamic/progressive or are stable (i.e. more consistent with CKD).
Any there any risk factors prompting early review / admission?
- Poor oral intake /urine output
- Hyperkalaemia, especially if moderate (K+ 6.0-6.4 mmol/L) or severe (K+ ≥ 6.5 mmol/L)
- Physiological evidence of deterioration (see NEWS2)
- Known CKD stages 4 or 5, or kidney transplant recipient
- Vulnerability to infection (therapeutic immunosuppression or immunodeficiency)
- Frailty with co-morbidities (CKD, diabetes, heart failure, liver disease, neurological or cognitive impairment)
- Past episodes of AKI
- Suspected intrinsic kidney disease (e.g. few pre/post renal features +/- abnormal urinalysis)
- Suspected urinary tract obstruction
Resources to guide response to AKI in primary care
The Think Kidneys Best Practice Guidance provides more detail on factors that require consideration when responding to AKI Warning Stage Test Results.
Table 2: Recognising and Responding to Acute Kidney Injury for Adults in Primary Care