Syncope toolkit
Information for commissioners
The health, social and economic burden of syncope for patients
Compared with people without syncope, those with syncope may experience the following:
- Reduced quality of life
- Increased fractures and soft tissue injury
- Unable to drive
- Unable to fly
- Unable to participate in leisure activities - competitive and recreational sport
- Twice as likely to lose their job
- 1.4 fold greater risk of accidents at work
- Increased levels of anxiety and depression
- Increased mortality, especially cardiac syncope.
The NHS syncope burden
Cost of syncope to the NHS
Much of the information regarding costs of hospital attendance, admission and investigation of syncope patients has been undertaken in secondary care settings and there is little information regarding syncope costs of management in primary care.
Key facts:
- 1-1.5% of A&E attendances are for syncope; 50% of patients are admitted to hospital
- 36% of patients experience significant trauma
- After attending A&E with syncope, 0.7% of patients die in the next 7-30 days, and 10% within a year
- Hospitalisation accounts for over 75% of the costs; most admissions are not necessary
- In a UK-based study, 25% of the patients had more than 20 tests, and 10% had more than 31 tests done
- Patients visit on average 3 different specialists and have 13 inconclusive tests before diagnosis.
Syncope care pathways
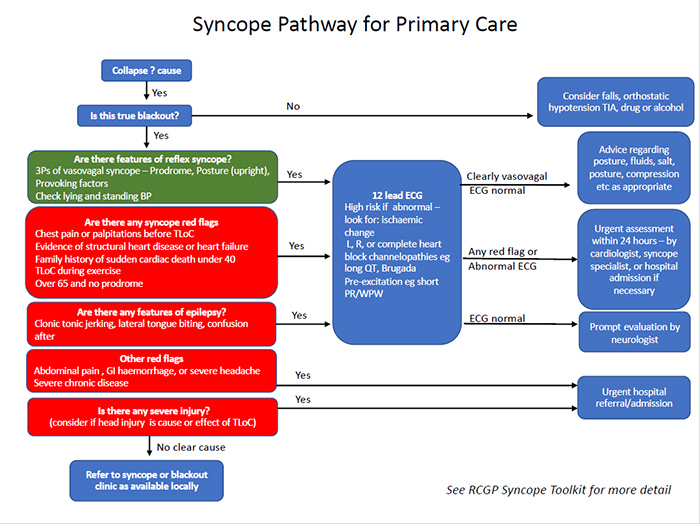
Download syncope pathway for primary care (76 KB PDF)
Syncope and Blackout clinics
Services available and referral procedures will differ throughout the UK.
Rapid Access Blackouts Units will usually see patients with both syncopal and non-syncopal causes of transient loss of consciousness (TLoC). Rapid Access Blackouts Clinics are often staffed by a multidisciplinary team of specialist nurses from backgrounds including cardiology, neurology and medicine for the elderly.
Syncope Units are usually based in secondary care. They can be led by any clinician with an interest in syncope such as cardiologists, A&E consultants and medicine for the elderly. A number of successful services are primarily nurse-led. Some clinics are virtual.
Some syncope clinics will also see patients with recurrent presyncope and PoTS.
- Referral to the unit may be from primary care, A&E, inpatient and outpatient secondary care and occasionally be self-referral
- It is recommended that rapid access referrals can be made for high risk patients
- Rapid access referrals from A+E can also be beneficial for low and intermediate risk patients to reduce hospital admission rates.
Syncope units can reduce healthcare costs primarily by:
- Reducing the number of admissions
- Reducing the duration of hospital stay
- Reducing the number of unnecessary tests.
Useful resources for commissioners
- Syncope Unit: rationale and requirement - the European Heart Rhythm Association position statement endorsed by the Heart Rhythm Society (2015)
- Blackout Care Pathways
- Healthcare Pioneers Report - showcasing best practice in syncope.