Resources for Secure Environments
| Site: | Royal College of General Practitioners - Online Learning Environment |
| Course: | Secure Environments Hub |
| Book: | Resources for Secure Environments |
| Printed by: | Guest user |
| Date: | Saturday, 7 March 2026, 1:13 AM |
Description
Providing healthcare in secure environments such as prisons, secure hospitals, young offender institutions and immigration removal centres presents unique challenges for GPs and primary care professional.
Table of contents
- Introduction
- National resources for secure environments
- Introductory resources
- Prescribing
- Infections and Communicable Diseases in Secure Environments (Public Health England)
- Pain
- Mental health
- Dementia
- Learning and intellectual disabilities
- Substance misuse
- End of Life and Palliative Care
- Third Sector Organisations
- Leadership
- Resources from the Royal Colleges
- Faculty of Forensic and Legal Medicine
- Deaths and complaints
- International
- Veterans
- Immigration
- Resources for Patients
- Learning and Intellectual Disabilities in Secure Environments
Introduction
Providing healthcare in secure environments such as prisons, secure hospitals, young offender institutions and immigration removal centres presents unique challenges for GPs and primary care professional. The RCGP Healthcare in Secure Environments project team has drawn together a comprehensive set of weblinks to provide sources of information to support healthcare professionals working in secure environments.
Providing healthcare in secure environments such as prisons, secure hospitals, young offender institutions, secure training centres and immigration removal centres presents unique challenges for GPs, nurses, pharmacy teams, other primary care and allied health professionals. It also provides unique opportunities for multi-disciplinary team working.
People in secure environments often have multiple complex physical health, mental health and substance misuse needs that exceed those of people living in the community. These issues can be compounded by social determinants that drive health inequalities, such as homelessness, unemployment, financial insecurity and debt, social isolation and poor access to or reluctance to engage with health services appropriate to their needs. Secure environments can exacerbate some of these challenges or provide an opportunity to address them.
Improving and better addressing the mental health, physical health and substance misuse needs of people in secure environments has the potential to improve their quality of life while inside and have a lasting impact on their health beyond release. This will have a further positive impact on the wider community.
The Healthcare in Secure Environments project team has created resources to assist clinicians starting out in secure environment healthcare which will be published over the coming months. They have also drawn together a comprehensive set of weblinks to provide sources of information for healthcare professionals working in secure environments.
The RCGP Secure Environment Group would like to set up a dynamic learning environment as part of the Healthcare in Secure Environments project in to:
- Share best practice and quality improvement initiatives
- Facilitate connection and exchange of clinical advice
- Discuss current issues and policies
- Facilitate sharing of policies, procedures and guidelines
National resources for secure environments
- The RCGP Secure Environments Group was established in 2004. It is committed to the delivery of health care of the highest possible standards to patients in the health and justice system.
- The RCGP Position statement on equivalence of care in secure environments asserts that prison health is public health and that people living in secure environments have a right to receive care that is of an equitable standard (but not necessarily the same) to people living in the community.
- The Worldwide Prison Health Research and Engagement Network (WEPHREN) is a global, open access collaborative forum for people interested in prison health. It brings together key stakeholders from across professions, disciplines and nations and supports professional development, equitable collaborative multi-centre research and health service growth initiatives. Through doing so, it aims to improve the health of people in prison.
- The NHS England Health and Justice commissions healthcare for children, young people and adults across secure and detained settings, including in prisons, secure facilities for children and young people, police and court Liaison and Diversion services and immigration removal centres, via 10 Health and Justice teams across 4 regions (North, Midlands, London and South).
- The NHSE Health and Justice Clinical Reference Group provides clinical oversight for Health and Justice commissioned services, championing best practice and evidence based approaches to healthcare provision. It represents the Health and Justice clinical body across the sector and makes links with all professions involved in service delivery, together with service users, their families and impacted communities.
- Public Health England has produced resources for 'public health in prison and secure settings' to track, treat and prevent single infections and outbreaks in prisons, secure settings and health services (see ‘Infections/Communicable diseases’ section)
- The Five Nations Health and Justice Collaborative Group provides a forum for health and justice partners in England, Scotland, Wales, Northern Ireland and the Republic of Ireland to debate and collaborate. The group aims to address health, well-being and social care issues relating to people in contact with the criminal justice system (CJS), particularly those in prisons. It informs the work of PHE as the UK Collaborating Centre for Health in Prisons and facilitates sharing of best practice. It also addresses health inequalities in order to reduce people offending and re-offending.NICE Guidelines for Assessment, diagnosis and management of Physical and Mental Health in prisons.
NICE Guidelines for Assessment, diagnosis and management of Physical and Mental Health in prisons
- NICE guideline (NG57) Physical health of people in prison (2016): This guideline covers assessing, diagnosing and managing physical health problems of people in prison. Recommendations include health assessments when people come into prison, promoting health and wellbeing in prison, managing medicines and managing health emergencies and rapid deterioration.
- NICE Quality standard (QS156) Physical health of people in prisons (2017): This quality standard covers assessing, diagnosing and managing physical health problems of adults aged 18 years and older in prisons or YOIs. There are five quality statements covering: medicines reconciliation, secondary screening, BBV and STI testing, lead care co-ordination for people with complex health and social care needs, and provision of TTOs or FP10 on transfer or discharge from prison.
- The 'NICE guideline (NG66) Mental health of adults in contact with the criminal justice system (2017)' covers the assessment, diagnosis and management of mental health problems in adults (aged 18 and over) in contact with the criminal justice system. It includes recommendations on psychological and pharmacological interventions, co-ordinated care planning and service organisation.
- The 'NICE Quality standard (QS163) Mental health of adults in contact with the criminal justice system (2018)' covers the recognition, assessment and management of mental health problems in adults (aged 18 and over) in contact with the criminal justice system. There are four quality statements which refer to: police response towards people with mental health problems, their referral for mental health assessment and appropriate information sharing of care and risk management plans between services.
Prison Healthcare Services in Wales
- The UK government is currently responsible for criminal justice in Wales but responsibility for healthcare (including prison healthcare) is devolved to the Welsh government. NHS Wales has accountability for prison health service planning and at a local level, Prison Health Partnership Boards, jointly chaired by Local Health Boards and the Governors of the prisons, have responsibility for the governance of prison health services.
There are five prisons in South Wales and one in North Wales, with a total population (all adult male) of 4,291 (figure for end April 2018). Each prison has a different profile, function and security category. HMP/YOI Parc is the only private prison in Wales and houses most 18-24 year olds serving custodial sentences, together with adults. Female and high-risk ‘Category A’ prison residents from Wales have to be housed in England. The nearest female establishments are HMP Eastwood Park, Gloucestershire and HMP Styal, Cheshire.
More information is contained in this 'Imprisonment in Wales: A Factfile'
- Public Health Wales has information produced by Public Health Wales about infectious diseases and prison specific outbreak planning. Other content includes the recently published adverse childhood experiences study and population level health interventions and policies.
- Healthcare provision in prisons in Wales: The Health, Social Care and Sport Committee of the National Assembly for Wales held an inquiry into health and social care provision in Welsh prisons and evidence was received from a number of organisations. It was delivered in 2021.
The Welsh Affairs House of Commons Committee has reviewed prison provision in Wales and produced the Prison provision in Wales report with recommendations for the government, including areas impacting on healthcare provision. These include: creating a central unit to facilitate NHS Wales/HMPPS healthcare delivery liaison and collaboration; appropriate substance misuse treatment; adequate funding and policies to support resettlement and ensure housing provision on release from prison.
This Partnership Agreement For Prison Health in Wales outlines agreed priorities between Her Majesty’s Prison and Probation Service (HMPPS) in Wales, the Welsh Government, Local Health Boards and Public Health Wales to drive improvements in the health and wellbeing of those held in Welsh prisons. The document recognises the unique statutory obligations of each partner organisation and builds on the shared objective of ensuring those in prison can live in environments that promote health and well-being and where health services can be accessed to an equivalent standard of those within the community. This supports the overarching aim that prison should be a place where an individual can reform their lives. To achieve this all parties have agreed to work toward the three objectives of the Welsh Government ‘Prosperity for All: The National Strategy for Wales’, ensuring that prisons and health services in prisons:
- Deliver quality health and care services fit for the future
- Promote good health and well-being for everyone
- Build healthier communities and better environments
Prison Healthcare Services in Scotland
- In Scotland, responsibility for criminal justice and prisons is devolved to the Scottish Government and responsibility for healthcare provision in prisons lies with NHS Scotland. In 2018, the government set up the Health and Social Care in Prisons Programme Board with the aim of driving health and social care improvement in prisons.
There are 15 prisons in Scotland, two of which are privately run. There is one dedicated women’s prison, HMP & YOI Cornton Vale, while women are also held in units at HMP Greenock, HMP Edinburgh and HMP & YOI Grampian. The total prison population in Scotland on 28/02/2020 was 8059. The female prison population in Scotland is one of the highest in Northern Europe and it has more than doubled since 2000.
- The Health in Custody Network is a national network in Scotland that aims to support the health inequalities agenda and reduce re-offending by working with partners in the Health and Justice sector, and with Public Social Partnerships and voluntary agencies in the Third Sector.
- Turas Learn is NHS Education for Scotland’s platform for learning and support resources. There is a page for health and social care professionals working in prisons that is due to be launched. It will provide a single point of access to take people out through links to different directorates.
- Information about healthcare in Scottish prisons has been published by the Scottish Public Health Observatory.
- NHS inform is Scotland's national health information service which provides links to patient health information.
Prison Healthcare Services in Northern Ireland
- In Northern Ireland, responsibility for criminal justice and prisons is devolved to the Northern Ireland Executive. Its Department of Health, Social Services and Public Safety has overall authority for health and social care services. The NHS in Northern Ireland is referred to as Health and Social Care Northern Ireland (HSCNI). The Public Health Agency HSCNI (PHA) is responsible for improving health and well-being and health protection and the PHA and HSC Board are responsible for the development of a fully integrated commissioning plan for health and social care across Northern Ireland.
Prison healthcare is delivered by South Eastern and Health and Social Care Trust (one of six HSC Trusts) across the three prison sites: Maghaberry Prison (high security, adult male, long term sentenced and remand); Magilligan Prison (medium to low security male, sentenced to six years or less); Hydebank Wood College and Ash House Women's Prison (education, learning and employment focus, young adults 18-21 years, unit for remand and sentenced female).
Introductory resources
In this section, there are resources to support clinicians navigating the challenges of safe equitable healthcare provision in secure settings. Further topics will be published over the coming months.
Prescribing
Prescribing in secure environments can be challenging due to the complexity of patient needs, the structural and operational limits of secure environments and the risks to the individual and the wider prison population associated with abuse and diversion of prescribed medicines and other illicit substances. This 'Top Tips for Safer Prescribing in Prisons', document has been written as a short accompaniment to the RCGP SEG Safer Prescribing in Prisons, 2nd Edition, January 2019. There are also links to further prescribing resources to equip clinicians for the challenge of prescribing in the secure context.
Healthcare staff starting out in prisons
Providing healthcare in secure environments is rewarding and demanding work. Primary care, substance misuse and mental health teams, along with other health professionals, have the opportunity to work together to provide integrated care for people, many of whom have complex needs. This 'Top tips for healthcare staff starting out in prisons' document gives an introduction to working in this different context. This GP+ Careers Podcast episode about Working in Secure Environments features a First5 GP working in secure environments and secondary care addiction services, providing valuable insights into working in a high security prison.
GPs working in immigration removal centres
People detained in immigration removal centres (IRC) in the UK are not prisoners. They have been administratively detained by the Home Office rather than their detention being ordered by a judge. While many persons may be foreign nationals who have just finished a prison sentence in the UK, the majority will be people who have either entered the UK irregularly or who no longer have the right to remain in the UK. This 'Top tips for GPs Working in Immigration Removal Centres' document provides some tips for GPs working in IRCs.
Prescribing
- The RCGP. Safer Prescribing in Prisons. Guidance for Clinicians. 2nd edition (770 KB, PDF) provides practical prescribing guidance for clinicians working in prison medicine.
- NHS England. Pain Management Formulary for Prisons: The formulary for acute, persistent and neuropathic pain. Second Edition: October 2017 and Implementation guide: December 2015 :There are two parts to this resource. The formulary provides a list of recommended medicines along with advice and clinical guidance links and the implementation guide covers scope and use of the formulary, prescribing and reviewing pain medicines in prison, self-management and optimising patient safety.
- Opioids Aware: This resource is for patients and healthcare professionals. It was produced by the Faculty of Pain Medicine of the Royal College of Anaesthetists in collaboration with PHE. It has five key messages which cover when opioids are useful (acute pain and end of life), when their benefit is limited (persistent pain), the increased risks of high dose opioids (equivalent to >120mg/d oral morphine), when to stop opioids and the importance of collaboration and planning when tapering and stopping.
- NHSE. Health and Justice mental health services: Safer use of mental health medicines (2017): This document provides a background to prescribing and mental health medicines in secure environments with clarification on the prescribing responsibility for initiating, continuing, reviewing or repeat prescribing of mental health medicines by specialist mental health prescribers.
- RCGP Top Ten Tips: Dependence Forming Medications. 2019: This brief guidance provides advice about patients safety and support and good clinical practice in relation to DFMs.
- NHS England Guidance for the handling of Tramadol in health and justice residential sites (2014) (PDF): From 10th June 2014, changes were made to the Misuse of Drugs Act (1971) to reclassify tramadol to a Schedule 3 Controlled Drug, exempted from safe custody requirements. This NHSE guidance provides information on the handling of Tramadol in health and justice settings as a result of the changes.
- PHE Dependence and withdrawal associated with some prescribed medicines: An evidence review (2019) (PDF): This important review by Public Health England was commissioned by the minister for public health and primary care. It sets out the scale, distribution and causes of prescription drug dependence in adults (aged 18 and over), and what might be done to address it. The review covers five classes of medicines: benzodiazepines; z-drugs; gabapentinoids; opioids for chronic non-cancer pain; antidepressants.
Infections and Communicable Diseases in Secure Environments (Public Health England)
Immunisation and Infection
Public Health England has published resources on immunisation and infectious diseases. People come into secure settings from the community and return from them to the community therefore advice for community settings is pertinent to people in prison. However, there are particular challenges posed by secure environments and therefore specific resources have been written to track, treat and prevent single infections and outbreaks in prisons, secure settings and health services.
Immunisation
- Immunisation against infectious disease – The Green Book
- COVID-19: the green book, Chapter 14a. Coronavirus (COVID-19) vaccination information for public health professionals
- COVID-19 vaccination programme
- Vaccine Update - newsletter for health professionals providing latest updates on vaccine development, policies and procedures
Infection
- Public health in prisons and secure settings - Resources to track, treat and prevent single infections and outbreaks in prisons, secure settings and health services.
- Infection control in prisons and secure settings
- Prevention and Management of Infections in Secure Settings
- Prevention of infection & communicable disease control in prisons & places of detention. A manual for healthcare workers and other staff (2011) This document for healthcare staff and others working in prisons and places of detention provides advice on: specific infections and dealing with outbreaks; immunisation and vaccination; infection prevention and control within custodial settings. It is designed to be used alongside PSO/PSIs and DH and HPA guidance and to complement local Infection Prevention and Control (IPC) procedures.
- Multi-agency contingency plan for the management of outbreaks of communicable diseases or other health protection incidents in prisons and other places of detention in England (2013, 2017) - joint HMPPS/NHS/PHE guidance; describes actions required to identify and manage an incident or outbreak and the roles and responsibilities of partner organisations involved.
- COVID-19
- Tuberculosis
- Managing tuberculosis (TB) in prisons (2013) – guidance for healthcare teams covering: TB screening in prisons, handling symptomatic patients, isolation (including recommendations re-court), treating TB and reporting cases.
- TB: Information for prison staff (2013) – leaflet about TB and handling infected prison residents
- Tuberculosis in prisons or immigration removal centres: NICE pathway (updated 2020)
- NICE pathway linked to the NICE guideline Tuberculosis NG33 (2019)
- Group A Streptococcal Disease and other bacterial infections
- Group A streptococcal disease (2019) – information for people in prison
- Preventing and Managing bacterial wound infections in prison (2019)– guidance for healthcare and residential staff and responding agencies on managing and preventing the spread of group A streptococcal (GAS) infection and other skin and soft tissue infections
- Influenza
- Other Viral Infections
- Guidance on Infection Control for Chickenpox and Shingles in Prisons, Immigration Removal Centres and other Prescribed Places of Detention (2017) – guidance on managing outbreaks of chickenpox or shingles for healthcare and other staff working in secure settings.
- Measles in prison: vaccination and infection control - information for staff (2013)
- Measles in prison: vaccination and infection control - information for prison residents (2013)
- Reporting single incidents and outbreaks
- List of reportable diseases to be notified to PHE Health Protection Teams by prison and other detention centre healthcare teams (updated 2020) - This guidance contains information about the importance of infectious disease surveillance in secure settings and a list of reportable diseases.
- Managing potential exposure to blood-borne viruses
- Guidance on management of potential exposure to BBVs in emergency workers - This resource contains information and guidance for frontline staff and service providers on BBV prevention and control, providing a generalised care pathway of management and action for cases of potential exposure which includes: first aid, risk assessment, management and follow up care.
- Improving testing and treatment rates for bloodborne viruses - Public Health England, the Hepatitis C Trust, British Liver Trust and National AIDS Trust recommend an ‘opt- out’ testing programme in prisons to improve the rates at which people in prison are tested for blood-borne viruses (BBVs).
- PHE resources on ‘opt out’ testing for BBVs
- Other Public Health England Resources for secure settings and Contact details for PHE Specialist Leads:
Pain
Public Health England. Managing persistent pain in secure settings. 2013
This resource aims to support healthcare professionals treating persistent pain in secure environments. It provides an overview of evidence based best practice and suggestions for context-specific implementation.
NHS England resources
- Pain Management Formulary for Prisons: The formulary for acute, persistent and neuropathic pain. Second Edition: October 2017
- Implementation guide: December 2015
There are two parts to this resource. The formulary provides a list of recommended medicines along with advice and clinical guidance links and the implementation guide covers scope and use of the formulary, prescribing and reviewing pain medicines in prison, self-management and optimising patient safety.
Opioids Aware
This resource is for patients and healthcare professionals. It was produced by the Faculty of Pain Medicine of the Royal College of Anaesthetists in collaboration with PHE. It has five key messages which cover when opioids are useful (acute pain and end of life), when their benefit is limited (persistent pain), the increased risks of high dose opioids (equivalent to >120mg/d oral morphine), when to stop opioids and the importance of collaboration and planning when tapering and stopping.
Pain in Secure Environments Course
This is a one-day course run by the Faculty of Pain Medicine and endorsed by Public Health England. It has been developed to meet the workforce training requirements for healthcare professionals working within Secure Environments.
NICE guideline [NG193]
This guideline covers assessing all chronic pain (chronic primary pain, chronic secondary pain, or both) and managing chronic primary pain in people aged 16 years and over.
Chronic Pain in Children and Young People (RCGP) This course aims to equip the GP with knowledge about the causes and
management of chronic pain in children. It will explore the impact and
appropriate assessment of pain in children up to the age of 18 and the
role the GP plays in the multi-disciplinary team.
Mental health
NHS England Health and Justice mental health services: Safer use of mental health medicines (2017)
This document provides a background to mental health medicines, medicines’ optimisation and prescribing in secure environments. It provides some clarity on the prescribing responsibility for initiating, continuing, reviewing or repeat prescribing of mental health medicines by specialist mental health prescribers.
NICE guideline (NG66) Mental health of adults in contact with the criminal justice system (2017)
This guideline covers the assessment, diagnosis and management of mental health problems in adults (aged 18 and over) in contact with the criminal justice system. It includes recommendations on psychological and pharmacological interventions, co-ordinated care planning and service organisation.
NICE Quality standard (QS163) Mental health of adults in contact with the criminal justice system (2018)
This NICE quality standard covers the recognition, assessment and management of mental health problems in adults (aged 18 and over) in contact with the criminal justice system. There are four quality statements which refer to: police response towards people with mental health problems, their referral for mental health assessment and appropriate information sharing of care and risk management plans between services.
NICE Quality standard (QS189) Suicide prevention (2019)
This quality standard covers ways to reduce suicide and help people bereaved or affected by suicide. There are five quality statements, three of which relate to the role of multi-agency suicide prevention partnerships, one about information sharing and confidentiality for adults at risk of suicide and one about tailored support for people bereaved or affected by suicide.
NICE Quality standard (QS34) Self harm (2013)
This quality standard covers the initial management of self-harm and the provision of longer-term support for children and young people (aged 8 to 18) and adults (aged 18 and over) who self-harm. There are eight quality statements covering: caring with compassion and respect for patients, assessment, monitoring, safe environments, risk management plans, psychological interventions and transitions between services.
NICE Quality standard (QS154) Violent and aggressive behaviours in people with mental health problems (2017)
This quality standard covers short-term prevention and management of violent and physically threatening behaviour among adults, children and young people with a mental health problem. It applies to settings where mental health, health and social care services are provided. There are five quality statements which include identifying triggers and de-escalation techniques to support patients, requirements around physical health monitoring when patients are restrained or given rapid tranquilisation, and provision of post-incident debrief for patients.
Mental Health and immigration detention
It is important that healthcare staff working in immigration detention are aware of the potential negative impact immigration detention can have on the mental health of immigration detainees (von Werthern et al (2018) & Bosworth, M (2016)). The limitations of immigration detention as a therapeutic environment are set out in the The Royal College of Psychiatrists “Position Statement on detention of people with mental disorders in Immigration Removal Centres”,.
Dementia
Alzheimer’s Society. The Prison Project: Raising Awareness of Dementia in Prisons
The Prisons Project was set up to raise awareness of dementia among prison staff and residents in order to increase the diagnosis rate in an ageing population.
Prisons and Probation Ombudsman Learning Lessons bulletin (Issue 11, July 2016)
This PPO Learning Lessons Bulletin explores the experience of prison residents with dementia and the challenges that prisons face when providing appropriate care and support for this vulnerable group of people.
Mental Health Foundation
The Mental Health Foundation's report 'Losing Track of Time. Dementia and the ageing prison population: treatment challenges and examples of good practice (2013)' set out to scope existing research on treating and managing male offenders with cognitive impairment and to identify and share examples of good practice.
HM Prison & Probation Service
In 2020, the Justice Select Committee of the House of Commons published the findings of their inquiry Ageing prison population. It identified the specific needs of the older population in prison, including accommodation, regime, health and social care needs, and release and resettlement planning.
Dementia-Friendly Communities and Local Dementia Action Alliances (LDAA)
At a local level, the Alzheimer’s Society supports communities to become dementia friendly. Until recently, the formation of Local Dementia Action Alliances was encouraged to provide structure for Dementia Friendly Communities (DFCs). Groups, made up of people from different sectors, were encouraged to set up a steering group and create a formal action plan to be published and updated on their local DAA website. While LDAAs continue, and can work towards DFC criteria to become officially recognised, some groups have found the formality surrounding LDAAs to be challenging.
New groups are being encouraged to use a more flexible approach, to establish an informal DFC steering group and to appoint a leader to facilitate a link between community members and the Alzheimer’s Society. There is a BSI PAS1365: A code of practice for dementia-friendly communities which recommends key areas for action to guide DFCs. The Alzheimer’s Society has DFC Officers who can support both newer, less formal DFCs and LDAAs (see web link and email contact details).
Get in touch by emailing: DementiaFriendlyCommunities@alzheimers.org.uk
HMP Littlehey action plan
HMP Littlehey is a member of a local DAA. They have an action plan for transforming care of residents with dementia by: raising awareness among staff and prison residents, joint working, and improving the physical environment. It is published on the link below.
Learning and intellectual disabilities
The Prison Reform Trust has highlighted the size and importance of the problem of learning disabilities also known as intellectual disabilities in prison: 7% of people in contact with the criminal justice system have a learning disability, compared with approximately 2% of the general population. Of those in prison with a learning disability, 85% report struggling to read prison information, 78% report problems filling in forms and 66% report making themselves understood. When including people with learning difficulties as well as learning disabilities, 34% of the prison population fall into this broader category. Of those with learning difficulties, the Prison Reform Trust found that 69% report struggled to read prison information and fill in forms and that 50% struggle to make themselves understood.
Many prisoners with intellectual disability may not have been formally diagnosed or identified. The prison healthcare team has an important part to play in diagnosis and referral for assessment to the mental health team.
Intellectual disability is closely associated with premature death. The LeDeR study is a learning disabilities mortality review in which every death in a person with a learning disability is evaluated. All such deaths should be reported to this study LeDeR.
Resources
The RCGP Secure Environments Group has produced 'Learning and Intellectual Disabilities in Secure Environments' resources and guidance for GPs and primary care professionals working in secure environments to help them improve their knowledge on how to support people with learning disabilities.
Substance misuse
- Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group (2017) Drug misuse and dependence: UK guidelines on clinical management. London: Department of Health: This is key guidance for clinicians treating people with drug problems in the UK and is frequently referred to as the ‘Orange book’. It was updated in 2017 and includes new guidelines about treating people in contact with the criminal justice system (community based and prison settings), new psychoactive substances and club drugs, misuse of prescription drugs and over-the-counter medicines and prevention of drug-related deaths, naloxone provision.
National Institute for Health and Care Excellence (NICE) Guidance
- NICE Quality standard (QS165) Drug misuse prevention (2018): The scope of this quality standard covers the prevention or delay of harmful use of drugs by assessing risk and signposting to appropriate services those children, young people and adults who are vulnerable to harmful use. There are four statements which refer to looked after children, care leavers, children in contact with youth offending services and adults. Although two statements apply directly to vulnerable individuals in community rather than settings, it is important to be aware of interventions and services that have the potential to change the trajectory of young lives and to be aware that looked after children and care leavers are over-represented in secure settings.
- NICE Quality standard (QS23) Drug use disorders in adults (2012): This quality standard covers assessment and treatment of drug use disorders in adults (aged 18 and over). It includes treating the misuse of opioids, cannabis, stimulants and other drugs.
- NICE Technology appraisal guidance (TA114) Methadone and buprenorphine for the management of opioid dependence (2007): This guidance for commissioners and providers considers the evidence for clinical and cost effectiveness of methadone and buprenorphine (oral formulations). It recommends a flexible case by case approach to deciding which drug to use and, where there is no difference in suitability, prescribing methadone as first choice. Other recommendations concern supervision of administration and embedding OST within a programme of supportive care.
- NICE (TA114) Methadone and buprenorphine for the management of opioid dependence - summary for patients and carers: This summarised guidance about the NICE TA on oral OST is written for patients and carers. If using the information for patients and residential staff, it is important to take in to account patient literacy levels and translation requirements, together with adjustments required for secure settings (e.g. supervised consumption only).
- NICE Technology appraisal guidance (TA115) Naltrexone for the management of opioid dependence (2007): This guidance covers the use of naltrexone under adequate supervision for detoxified, highly motivated people who were formerly opioid-dependent.
- NICE Clinical guideline (CG51) Drug misuse in over 16s: psychosocial interventions: This guideline covers treatment of problem drug use or dependence in adults and young people over 16 using psychosocial interventions, with the aim of reducing illicit drug use and improving people’s physical and mental health, relationships and employment
- NICE Clinical guideline (CG52) Drug misuse in over 16s: opioid detoxification: This guideline covers opioid detoxification in adults and young people over 16 in community, residential, inpatient and prison settings. It does not cover treatment of women who are pregnant.
- NICE Clinical guideline (CG120) Coexisting severe mental illness (psychosis) and substance misuse: assessment and management in healthcare settings (2011, 2016): This guideline covers assessment and management of people aged 14 years and over with coexisting severe mental illness (psychosis) and substance misuse. All adults and young people with psychosis and suspected drug use or with substance misuse and suspected psychosis should be referred to CAMHS or secondary care mental health.
NHS England
- NHS England (2018) Advice on actions for suspected ingestion of nicotine e-cigarette vaping liquid:This brief information, prepared to support staff delivering care in health and justice settings, provides basic advice about e-cigarette and vaping products, signs and symptoms of nicotine toxicity and action to be taken when this suspected.
Public Health England
- Public Health England: Five Nations Health and Justice Collaboration Statement on the presence of new psychoactive substances in custodial settings (2017): This statement contains information on the prevalence of NPS use in the community, feedback from people in prison, and recommendations for prisons that includes: clinical management plans; monitoring of drug use to inform health, security and operational policy; staff training and future research.
- Public Health England. New Psychoactive Substances (NPS) in prisons: a toolkit for prison staff (2017): This toolkit provides information and advice to support custodial, healthcare and substance misuse staff working in prisons to manage NPS use from a clinical, psychosocial and regime perspective. A number of principles can also be applied in community settings.
The Home Office
- New Psychoactive Substances (NPS) resource pack (2015/16): This resource pack contains information about NPS and advice on intervention. It is designed to equip educators and practitioners working with young people to discuss NPS and prevent and challenge drug-taking behaviour.
Project NEPTUNE
- Project NEPTUNE (Novel Psychoactive Treatment UK Network) was set up in response to the emerging clinical challenge of harms related to club drugs and NPS. It has produced a comprehensive clinical guidance paper and other related resources (see linked documents). There are e-learning modules which are open access but require registration.
- NEPTUNE Guidance on the Management of Acute and Chronic Harms of Club Drugs and Novel Psychoactive Substances (2015): This guidance is aimed at clinicians and other practitioners working across a range of settings. It is comprehensive and designed to help improve clinical practice in the management of NPS and club drug-related harms.
- NEPTUNE. Harms of Synthetic Cannabinoid Receptor Agonists (SCRAs) and Their Management (2016): This guidance provides advice about harms and management of harms associated with acute toxicity and chronic use of *SCRAs (*a range of synthetic cannabinoids often referred to as ‘Spice’, popular in prisons and among homeless populations.)
- NEPTUNE. Club Drug Use Among Lesbian, Gay, Bisexual and Trans (LGBT) People (2016): This document is intended to guide improvements in service and treatment planning. It describes patterns and factors relating to club drug use among LGBT sub-populations and discusses drug-related and other harms, including high-risk sexual behaviours.
- NEPTUNE. The misuse of synthetic opioids: harms and clinical management of fentanyl, fentanyl analogues and other novel synthetic opioids. Information for clinicians (2018): This document provides information on clinical management of the health-related harms associated with acute and chronic misuse of synthetic opioids. It is based on based available evidence.
- NEPTUNE. ATOMIC is a
free, evidence-based, mobile-learning application aimed at clinicians and other
practitioners who want to improve their knowledge of the acute and chronic
clinical harms of non-medical prescription drug use.
The European Monitoring Centre for Drugs and Drug Addiction
- Guidance for the use and reduction of misuse of benzodiazepines and other hypnotics and anxiolytics in general practice (PDF): This evidence-based guidance was written to support primary care clinicians prescribing and managing withdrawal and dependence on benzodiazepines and ‘Z’ drugs. It also considers misuse and the different effects sought from benzodiazepines. It has not been endorsed by other bodies and does not replace advice in the ‘Orange book’ however it provides helpful primary-care focused guidance.
Regional Medicines Optimisation Committee (RMOC)
- Position Statement. Oral Vitamin B supplementation in alcoholism (Nov 2019) (PDF): The RMOC has issued a position statement on oral Vitamin B supplementation in chronic alcoholism (parenteral supplementation is not covered). Vitamin B complex preparations are no longer recommended for prevention of Wernicke’s Encephalopathy in alcoholism however they may be prescribed on a short-term basis (10 days) for patients at risk of refeeding syndrome (see NICE CG32 Box 1 below). Vitamin B complex (as Vitamin B compound strong) may also be prescribed in rare cases e.g. medically diagnosed deficiency or chronic malabsorption.
Oral thiamine should continue to be prescribed (see NICE CG100) 200-300mg daily in divided doses for the prevention of Wernicke’s Encephalopathy to harmful or dependent drinkers who are malnourished (or at risk or malnourishment), have decompensated liver disease, acute withdrawal, before and during planned medically assisted alcohol withdrawal. Following successful alcohol withdrawal, thiamine should be continued for 6 weeks, providing patients have regained an adequate nutritional status.
- RMOC Buprenorphine Long Acting Injection Guidance (April 2021): The RMOC has produced guidance on the use of long-acting Buprenorphine injection opioid substitution treatment in community settings and secure environments (e.g. prisons, immigration removal centres, children and young people secure estates) in England. The guidance is aimed at substance misuse service providers, commissioners, community pharmacies and acute NHS Trusts in England. It includes topics such as practical considerations in different care settings, starting treatment and transferring care. It provides recommendations, clinical scenarios and a Buvidal® cost calculator to provide guidance to organisations/commissioners on the potential financial impact of Buvidal® implementation for a local population.
NICE Guidelines for Assessment, diagnosis and management of Physical and Mental Health in prisons
- NICE Clinical guideline (CG100) Alcohol-use disorders: diagnosis and management of physical complications (2010, 2017): This guideline provides recommendations on managing acute alcohol withdrawal and treating alcohol-related conditions in adults and young people (aged 10 years and older) with physical health problems that are completely or partly caused by an alcohol-use disorder.
- NICE (CG115) Alcohol-use disorders: diagnosis, assessment and management of harmful drinking (high-risk drinking) and alcohol dependence (2011): This guideline covers identification, assessment and management of alcohol-use disorders (harmful drinking and alcohol dependence) in adults and young people aged 10–17 years. Through improved assessments and goal setting for reduced consumption, it aims to reduce physical and mental health problems caused by alcohol.
NICE CG32: Box 1 - Criteria for determining people at high risk of developing refeeding problems
|
Patient has one or more of the following:
|
|
Or patient has two or more of the following:
|
Prescriber
- Parsons G. (2018) Guide to the management of gabapentinoid misuse: This article covers licensed and unlicensed indications of pregabalin and gabapentin, their pharmacology, misuse and management of patients who are discontinuing them.
Courses
- Drugs: Management of Drug Misuse (Level 1): This is an online course which provides introductory learning on evidence-based treatment of substance misuse in primary care, including the role of opiate substitution therapies (OST). It is a useful starting point for staff working in secure environments.
Addiction Professionals: Registration body and network (formerly known as SMMGP and FDAP)
The SMMGP (Substance Misuse Management in General Practice) – FDAP (Federation of Drug and Alcohol Practitioners partnership has changed its name to Addiction Professionals. It is a network for people from a wide range of professional backgrounds including GPs, psychiatrists, counsellors, key workers, pharmacists, psychologists, social workers, nurses and mentors, who work in the field of addictions treatment, including alcohol, other drugs and behavioural addictions. The organisation offers training and support for members and provides quality assurance through registration and professional accreditation. It runs ongoing professional development courses and provides free resources, which include a range of webinars and published guidance, pertinent to managing substance misuse in prison.
Webinars (published by SMMGP)
- Buprenorphine prescribing in criminal justice settings - the real picture
- How to deliver effective opioid substitution treatment in prisons
End of Life and Palliative Care
- Ambitions for Palliative and End of Life Care: This document was developed by the National Palliative and End of Life Care Partnership.
- Dying well in Custody Charter:The Dying well in custody charter is a prison-specific adaptation of the Ambitions for Palliative and End of Life Care Framework. ‘I statements’ and standards are attached to each of the six positive ambitions. The Ambitions and Standards ensure that care is coordinated across the secure setting and that staff are supported to achieve a level of competence and confidence to deliver end of life care professionally and with dignity. There is a self-assessment tool available with an ACT and ADOPT checklist to support implementation of the Charter.
- The Gold Standard Framework Training Programme in Prisons: The Gold Standards Framework has three steps: Identify, Assess, Plan well. Identification of prison residents in their last year of life allows for comprehensive assessment of their evolving needs and well-coordinated care and support. There is a GSF training programme for prisons. Engagement in the training programme requires two nominated leads from a prison to attend interactive workshops, share good practice examples, evaluate current practice and lead local implementation, sharing learning and expectations with staff in their own setting.
- RCGP Palliative and End of Life Care Toolkit: This toolkit has been developed in partnership with Marie Curie to support healthcare professionals to identify early those patients who are likely to die within 12 months and then to provide well-coordinated proactive care in their last 12 months of life. There are links to clinical guidance, national reports and best practice, resources for patients and carers, and training and appraisal tools.
- The Daffodil Standards: The RCGP and Marie Curie UK have jointly drawn up eight Daffodil Standards. They consist of quality statements, evidence-based tools, reflective learning exercises and quality improvement actions designed to assist primary care providers to reliably support all patients with advanced serious illness and end of life care needs.
Although not specifically tailored to the criminal justice system or to lower literacy levels, the information is likely to be helpful for staff in secure and community environments and may act as a starting point for discussion with residents and their families. The links below provide further resources from the research.
- End of life care for people with problematic substance use
- Clayson A, Sargent Z. End of life care for people with alcohol and other drug problems research project: ‘Insider Insights’ (2018) (PDF)
Do Not Attempt CPR (DNACPR) AND Advanced Directives
- Guidance from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. Decisions relating to CPR (2016)
- Advance Decisions (living wills)
- Compassion in Dying (DNAR forms and CPR decisions) (PDF)
DNACPR
As the age of the prison population increases and lengthy sentences continue to be administered by the courts, an increasing number of patients are likely to die in prison. It is important to identify early those patients in their final 12 months of life and, as part of their proactive care, to have timely and honest discussions about the appropriateness of CPR. Even if a clinician decides that CPR will not be appropriate for a patient, it is important to discuss the decision with them, unless it is deemed that ‘physical or psychological harm’ will be caused. DNACPR forms vary across different services but should be transferred with the patient if they move from one setting to another.
Advance Decisions (living wills, advance directives, ADRT) are legally binding documents which must be written down, signed by the patient (who must have capacity at the time of writing) and signed by a witness. They do not require a solicitor or a specific form to be completed. An Advance Decision allows someone to refuse any medical treatment in advance. It will only be used if they do not have capacity to make or communicate a decision for themselves. Decisions around CPR may be included in advance decisions if desired.
Advance Statements may also be written. These are not legally binding but can express a patient’s preferences, wishes, beliefs and values regarding their future care. Anything written in an Advance Statement must be taken into account when making a best interests decision for that person. There are links below relating to CPR decision making, DNAR forms and Advance Decision forms.
Release on Temporary License and Early Release on Compassionate Grounds
‘Early release may be considered where a prisoner is suffering from a terminal illness and death is likely to occur soon. There are no set time limits, but three months may be considered to be an appropriate period. It is therefore essential to try to obtain a clear medical opinion on the likely life expectancy. The Secretary of State will also need to be satisfied that the risk of re-offending is past and that there are adequate arrangements for the prisoner's care and treatment outside prison.
Early release may also be considered where the prisoner is bedridden or severely incapacitated. This might include those confined to wheelchairs, paralysed or severe stroke victims. Applications may also be considered if further imprisonment would endanger the prisoner's life or reduce his or her life expectancy. Conditions which are self-induced, for example following a hunger strike, would not normally qualify a prisoner for release.’
How to make an application on medical grounds – determinate sentence
- Chapter 12 Appendix A details compassionate release criteria (medical and tragic family circumstances).
- Chapter 12 Appendix B Form 210 Section 4 is the part of the application that should be completed by the registered medical practitioner. It is important to give as much information about the medical condition as possible, to include other reports e.g from hospital consultants and to provide an indication of likely life expectancy in the report.
Early Release on Compassionate Grounds Policy Framework
How to make an application on medical grounds – indeterminate sentence
- Compassionate release medical grounds criteria:
- ‘the prisoner is suffering from a terminal illness and death is likely to occur very shortly (although there are no set time limits, 3 months may be considered to be an appropriate period for an application to be made to Public Protection Casework Section [PPCS]), or the ISP is bedridden or similarly incapacitated, for example, those paralysed or suffering from a severe stroke AND
- the risk of re-offending (particularly of a sexual or violent nature) is minimal AND
- further imprisonment would reduce the prisoner’s life expectancy AND
- there are adequate arrangements for the prisoner’s care and treatment outside prison AND
- early release will bring some significant benefit to the prisoner or his/her family.
- Resource and cost implications of maintaining staff on bed-watch duties at an outside hospital/hospice are not grounds to justify release on compassionate grounds if the criteria set out above are not met. Other examples of cases not meeting the criteria are where conditions are self-induced, for example: following a hunger strike or where a prisoner refuses treatment.
- Chapter 12 Annex A Compassionate Medical Condition Report form Section 4 is the part of the application that should be completed by the registered medical practitioner. It is important to give as much information about the medical condition as possible, to include other reports e.g. from hospital consultants and to provide an indication of likely life expectancy in the report.
Third Sector Organisations
- Clinks supports, promotes and represents the voluntary sector, working with people in the criminal justice system and their families. Its vision is of a vibrant, independent and resilient voluntary sector that enables people to transform their lives. It produces resources and runs events, training and conferences.
- The Howard league for Penal Reform is a national charity, independent of government, which works with parliament, the media, criminal justice professionals, students and members of the public to influence debate and progress meaningful change to create safer communities. It provides a legal service for children and young people in custody, conducts research, and runs a variety of campaign programmes. Recent programmes have included transforming prisons, reducing child arrests and promoting real work in custody.
- The Independent Advisory Panel on Deaths in Custody (IAP) is an ‘arms-length’ body co-sponsored by the Ministry of Justice, Home Office and Department of Health and Social Care whose core aim is to bring about a continuing and sustained reduction in the number and rate of deaths in all forms of state custody in England and Wales. IAP provides independent advice and expertise to the Ministerial Board on Deaths in Custody. It also makes recommendations to operational services and provides guidance on policy and best practice across sectors.
- INQUEST is a charity which provides free and independent advice to bereaved people following a death in state care or detention in England and Wales. Their specialist casework includes deaths in police and prison custody, immigration detention, mental health settings and deaths involving multi-agency failings or where wider issues of state and corporate accountability are in question. They provide casework support through the inquest and investigation process for cases within their remit, and have online resources and a handbook available for anyone facing an inquest into the death of a relative.
- Medical Justice is a third sector organisation which helps people in detention, undertakes research, publishes reports to help to bring about policy change and campaigns to improve health care for people held in detention. It writes medico-legal reports which can be used to support asylum claims and letters outlining significant medical concerns.
- Nacro is a national social justice charity offering support with jobs, education and training, resettlement and rehabilitation, health and wellbeing, and housing. Nacro’s Justice team works with young and adult offenders in prisons and in the community, supporting them to change their lives and to reduce the risk of reoffending. Nacro has recently published a Resettlement guide for healthcare professionals. The guide was written to introduce healthcare professionals working in the prison environment to the challenges faced by service users on leaving custody and to the resettlement interventions designed to meet these challenges. The guide provides prompts for action that the healthcare team can take to support service users.
- The Prison Reform Trust (PRT) is an independent UK charity founded in 1981 which coordinates research, communications and advice functions. It works with partner organisations where necessary and gathers, analyses and publishes the facts about UK prisons, aiming to promote good practice, influence policy makers and inform prisoners, staff and the wider public. Its main objectives are to reduce unnecessary imprisonment, promote community solutions to crime, improve treatment and conditions for prisoners and their families and to promote equality and human rights in the justice system.
- The Prisoners’ Education Trust is a prison education charity which works in every prison in England and Wales. It funds around 250 different courses in levels and subjects which are otherwise unavailable. It supports people to choose courses, build connections with others and progress with their learning and it Champions the positive impact of education on rehabilitation.
- The Royal British Legion is the country’s largest Armed Forces charity, providing support to serving and ex-serving personnel and their families. It offers expert advice and guidance, support with recovery, rehabilitation and transitioning to civilian life. RBL outlines key priority areas and highlights actions for the government to improve the health, finances and wellbeing of the Armed Forces, veterans and their families.
- SSAFA (Soldiers', Sailors' & Airmen's Families Association) is the UK’s oldest national Armed Forces charity. SSAFA VCJS Support Service provides direct support to members of the Armed Forces, veterans and their families in contact with the criminal justice system. It works collaboratively with a number of other organisations including Clinks, NACRO, Prisoners’ Education Trust, POPS, Pact, Inside Time, Barnardo’s and Unlock in order to provide holistic support.
- Unlock is an independent national charity that provides information, advice and support for people with convictions who are facing barriers because of their criminal record. Unlock also provides training and resources about criminal record disclosure to practitioners who support people with convictions and supports employers in the fair treatment of people with criminal records.
- The Centre for Mental Health is a charity which works with partner organisations to carry out research, economic analysis and policy influence in mental health. It publishes reports on a variety of criminal justice topics including prevention of suicide, Mental health and criminal justice service transitions for young adults, employment support, therapy dogs.
Leadership
Pete Wynter is Director of the Leadership College London (endorsed by the Institute of Leadership and Management), Founding Director at Onelife Leadership, a charitable company working with young leaders around the UK and beyond, and he trains top flight athletes in leadership and team dynamics as part of the coaching team at Gloucester Rugby. Fernando Carrillo is a leadership consultant at Leadership College London and founder of WellWater, a charity that seeks to develop leaders committed to improving the lives of others.
Pete and Fernando recently delivered leadership training workshops at the RCGP SEG 7th Health and Justice Summit (see links to videos). They also run London’s Leadership Podcast which has bite-sized videos for feeding leadership knowledge, recommended reading, and a series of podcasts. The podcasts can be listened to ‘on the go’ on the iTunes podcast app but, for on-site lunchtime team learning, use the weblink.
Resources from the Royal Colleges
Resources from the Royal College of Nursing
- The RCN has produced six 'Time and space' mindfulness based videos, each around seven minutes long, covering different stages of the day. They have been produced to help clinical staff manage the stresses of the working day.
Resources from the Royal College of Psychiatrists
The Quality Network for Prison Mental Health Services
The Quality Network for Prison Mental Health Services (QNPMHS) was set up in 2015 to promote quality improvement in prison mental health services. It is one of the Royal College of Psychiatrists’ Centre for Quality Improvement programmes.
The QNPMHS engages mental health services who are part of its membership in an annual cycle of self and peer-review. The network aims to: promote quality improvement; share best practice; encourage openness; create a model of engagement and help services benchmark against other ‘like’ services, plan future improvements and demonstrate the quality of their care provision.The QNPMHS runs events and also shares learning both through publishing resources from their past events and by running an online discussion forum on the QNPMHS group page of the knowledge hub. Members can join the knowledge hub by email prisonnetwork@rcpsych.ac.uk. Enquiries about QNPMHS can be made to Kate Townsend, Programme Manager. Email: Kate.Townsend@rcpsych.ac.uk
The QNPMHS has produced the 'Standards for Prison Mental Health Services', which provide a framework for assessment of the quality of care provided by mental health services, through a process of self and peer review.
Faculty of Forensic and Legal Medicine
The Faculty of Forensic and Legal Medicine (FFLM) is one of the faculties of the Royal College of Physicians. It was founded to promote the advancement of education and knowledge in the field of forensic and legal medicine and to develop and maintain good practice of forensic and legal medicine by ensuring the highest professional standards of competence and ethical integrity, for public benefit. There are a number of useful publications on topics relevant to the secure environment.
Managing patients who conceal illicit drugs (Packers and Stuffers)
Recommendations for healthcare professionals asked to perform intimate body searches. Guidance for doctors from the British Medical Association and the Faculty of Forensic & Legal Medicine.
Deaths and complaints
The Prisons and Probation Ombudsman (PPO) carries out independent investigations into deaths and complaints in custody. The purpose of PPO investigations is to understand what happened, to ensure justice is done and to identify learning for the organisations involved. Fatal incident reports and action plans are published once inquests have taken place.
Learning lessons bulletins are published following collective analysis of PPO investigations. They cover a range of topics with the aim of potentially helping to prevent future avoidable deaths and resolve issues that may lead to complaints.
International
- European Committee for the Prevention of Torture and Inhuman or Degrading Treatment or Punishment (CPT): The European Committee for the Prevention of Torture and Inhuman or Degrading Treatment or Punishment (CPT) was set up under the Council of Europe’s “European Convention for the Prevention of Torture and Inhuman or Degrading Treatment or Punishment” in 1989. The function of the CPT is to protect people deprived of their liberty against torture and other forms of ill-treatment. The CPT visits places of detention including prisons, YOIs, secure training centres, IRCs, police stations and psychiatric hospitals to assess the treatment of people held there. After each visit, a detailed report is provided by the CPT to the State in which the place of detention is located, with findings and recommendations. A response to any issues raised is required.
- United Nations Humans Rights Office of the High Commissioner: The Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment (“SPT”) - The Office of the High Commissioner for Human Rights (UN Human Rights) has a mandate to promote and protect all human rights for all people. The Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment (“SPT”) is a treaty body authorised to proactively prevent torture and ill treatment through visiting places of detention and advising and providing assistance on the establishment of National Preventive Mechanisms.
- World Health Organisation (Europe) Prisons: Publications on prison health are available through both the WHO international and the WHO Europe web pages.
- WHO Health in Prisons Programme (HIPP): HIPP was set up in 1995. It promotes health in prison settings by providing technical advice to member states on communicable diseases, illicit drug use, mental health and prison health system development. It aims to: encourage integrated working between prison health, public health and NGOs; promote adherence to recognised international codes of human rights and medical ethics; reduce exposure to communicable diseases in prisons; promote equivalence of healthcare with the wider community; reduce reoffending by contributing to drug and mental health rehabilitation.
- Partnership for Health in the Criminal Justice System: The Partnership for Health in the Criminal Justice System website provides prison health-related resources supplied by WHO/Europe and partner organizations. The platform also facilitates opportunities for sharing good practice and networking.
- The Worldwide Prison Health Research and Engagement Network (WEPHREN) is a global, open access collaborative forum for people interested in prison health. It brings together key stakeholders from across professions, disciplines and nations and supports professional development, equitable collaborative multi-centre research and health service growth initiatives. Through doing so, it aims to improve the health of people in prison.
Veterans
- The RCGP has partnered with NHS England and NHS Improvement to produce a Veteran's Healthcare Toolkit containing guidance for GPs on how to meet the healthcare needs of military veteran patients and their families. The guidance includes details of dedicated veterans’ health-related services, other services and advice on requesting service medical records.
- Royal British Legion
- SSAFA (Soldiers', Sailors' & Airmen's Families Association). This website provides details of support available to veterans in the criminal justice system and to their families.
Immigration
- The BMA Report: Locked up, locked out: health and human rights in immigration detention (2017) report explores the role of doctors in protecting and promoting health-related human rights of detained individuals.
- Public Health England. NHS entitlements: migrant health guide (2014, updated 2020): All prisoners and immigration detainees are exempt from charges for healthcare. This guidance explains NHS entitlements in England for overseas visitors. There is separate guidance about NHS services for overseas visitors to Scotland produced by NHS Inform
- The Detention Centre Rules 2001 is a key statutory document which applies to IRCs (but not short term holding facilities). The rules set out the purpose of detention and what people in detention should have access to, including healthcare, welfare and privileges. Rules 33-37, 40 and 42 are particularly important to doctors and other healthcare staff.
- Detention Services Orders: All healthcare personnel working in immigration removal centres should familiarise themselves with the Detention Services Orders which provide further guidance on procedures in detention. Of particular importance (although not limited to):
Though not directly relevant to healthcare personnel it is important for healthcare to understand how the Home Office deal with vulnerability and how Rule 35/32 reports fit into a larger system:
- Medical appointments outside the detention estate
- Medical emergency response codes
- Medical information sharing
- Pregnant women in detention
- Release of detainees from immigration detention
- Removal from association and temporary confinement
- Self harm reduction strategy – Assessment care in detention and teamwork
Further information on Rule 35
- Home Office: Detention services order 09/2016 Detention centre rule 35 and Short- term Holding Facility rule 32 Version 7.0 (2019)
Rule 35 of Detention Centre Rules and Rule 32 of Short-term Holding Facility Rules aim ‘to ensure that particularly vulnerable detainees are brought to the attention of those with direct responsibility for authorising, maintaining and reviewing detention’. These rules stipulate that healthcare staff must report to Home Office caseworkers responsible for managing and reviewing a person’s detention:
- the likelihood of a detainee’s health being injuriously affected by continued detention
- a suspicion that a detained person has suicidal intentions
- concern that a detained person may have been a victim of torture
This Home Office guidance provides advice about the preparation and consideration of rule 35 and rule 32 reports. Doctors must complete rule 35 reports in IRCs. In Short-term Holding Facilities both doctors and registered nurses may complete rule 32 reports.
Mental Health and immigration detention
It is important that healthcare staff working in immigration detention are aware of the potential negative impact immigration detention can have on the mental health of immigration detainees (von Werthern et al (2018) & Bosworth, M (2016)). The limitations of immigration detention as a therapeutic environment are set out in the The Royal College of Psychiatrists “Position Statement on detention of people with mental disorders in Immigration Removal Centres”,
Resources for Patients
Exercise and relaxation resources
If people are unable to access the gym or take part in communal activities, this can impact on their physical and mental health. These in-cell exercise, relaxation and yoga resources have kindly been provided by Cell Workout and Prison Phoenix Trust. There are also links to gentle exercises for people with reduced mobility, at risk of escalating frailty and falls.
Cell-based workouts
- The Cell Workout exercises were produced by LJ Flanders (taken from his book, Cell Workout) and originally published in Inside Time, the national online newspaper for prisoners and detainees.
- Cell Workout No 1 (PDF) contains general advice on the benefits of a healthy lifestyle.
- For complete body exercises:
- Cell Workout No 2 (PDF)
- Cell Workout No 3 (PDF)
- Cell Workout No 4 (PDF)
- Cell Workout No 5 (PDF)
- Cell Workout No 6 (PDF)
- Cell Workout No 7 (PDF)
- To target more specific muscle groups:
- Cell Workout No 8 (PDF)
- Cell Workout No 9 (PDF)
- Cell Workout No 10 (PDF)
- We would suggest printing off Cell Workout No 1 (general advice) and then choosing another Cell Workout sheet to print off. This will provide a small selection workouts, giving the resident some choice and variation in their in-cell workout routine.
- Inside Time contact details:
Inside Time, PO Box 251, Hedge End, Hampshire, SO30 4XJ
e: info@insidetime.org
t: 01489 795945
Exercises for people with limited mobility
People with limited mobility will be at risk of increasing frailty and falls if they are confined to their cell or room. Exercises using resistance bands may be useful but will usually require additional guidance from a physiotherapist or a member of the gym staff. Security clearance and consideration of individual patient risk (e.g. avoid if on ACCT) will also be required. The links below are to guide gentle in-cell exercise.
- NHS Sitting Exercises
- Flexibility (PDF)
- Balance (PDF)
- Strength (PDF)
- All Active. Chair based strength exercises (resistance bands) (PDF)
- Age UK. Preventing Falls: Strength and balance exercises for healthy ageing (PDF)
- South Cambridgeshire Falls Prevention Service: Chair based exercise (PDF)
- Parkinson’s exercise framework: Key messages for professionals to give the people they support (PDF)
- Age UK. Elderly Fall Prevention: Avoiding a fall
Relaxation resources
The Prison Phoenix Trust provides books and CDs for prison residents which contain advice on relaxation and yoga exercises. They have generously provided printable resources for the Spotlight Toolkit:
- How to Meditate (PDF)
- Everyday Yoga (PDF)
- Cell Bed Yoga (PDF)
- Chair Yoga for Everybody (PDF)
- Square Breathing (PDF)
- Yoga for Worrying (PDF)
- Yoga for Strength (PDF)
- Yoga for Sleep (PDF)
Prison Phoenix Trust For further information, contact:
The Prison Phoenix Trust
PO Box 328, Oxford OX2 7HF
t: 01865 512521
COVID-19 patient resources
Resources written for people in secure environments during the Coronavirus pandemic can be found at: COVID-19 Resource Hub: Specific patient groups and settings (rcgp.org.uk)
Learning and Intellectual Disabilities in Secure Environments
Introduction
The Prison Reform Trust has highlighted the size and importance of the problem of learning disabilities also known as intellectual disabilities in prison: 7% of people in contact with the criminal justice system have a learning disability, compared with approximately 2% of the general population. Of those in prison with a learning disability, 85% report struggling to read prison information, 78% report problems filling in forms and 66% report making themselves understood. When including people with learning difficulties as well as learning disabilities, 34% of the prison population fall into this broader category. Of those with learning difficulties, the Prison Reform Trust found that 69% report struggled to read prison information and fill in forms and that 50% struggle to make themselves understood.
Many prisoners with intellectual disability may not have been formally diagnosed or identified. The prison healthcare team has an important part to play in diagnosis and referral for assessment to the mental health team.
Intellectual disability is closely associated with premature death. The LeDeR study is a learning disabilities mortality review in which every death in a person with a learning disability is evaluated. All such deaths should be reported to this study LeDeR.
Introductory resources
NHS England: Beyond the High Fence. From the unheard voices of people with a learning disability, autism or both.
NHS England published a document in early 2019 called ‘Beyond the High Fence’. It was co-produced with people with a learning disability or autism with lived experience of being in prison or in a secure hospital setting. Problems identified with being in prison included: a lack of nurses with expertise in learning disabilities (LD) and autism, a lack of prison staff understanding of LD and autism, excessively strict rules and frequent restraints, a lack of emotional support, bullying by other prisoners and the experience of prison resulting in a detrimental impact on mental health. Although experience of secure hospitals was overall better than being in prison, problems associated with hospitals included: poor handover from prison, over-medication with psychotropic drugs, being locked up for years longer than would have been the case in prison, institutionalisation and loss of confidence about independence, delays between parole board hearings and mental health tribunals.
Neisha Betts, Project Manager, Health & Justice, NHS England & NHS Improvement and Ann Norman RCN Criminal Justice nursing adviser at the Royal College of Nursing & learning disability nursing UK were approached by the RCGP Spotlight Project team for their expert advice on learning disabilities in the secure environment. A comprehensive toolkit produced by HMPPS: Making services work for people with learning disabilities and challenges (LDC), a toolkit for prisons and probation staff is available. There are opportunities for ‘lunchtime learning’ and multi-disciplinary team discussion with the aim of raising awareness and standards of care for people with LD in secure environments.
Department of Health and Social Care. Betts, N. Positive Practice, Positive Outcomes, A handbook for Professionals in Criminal Justice System working with Offenders with Learning Disabilities, 2011 Edition.
This publication has concise chapters explaining learning disabilities (LD) definitions, LD and the Criminal Justice System, health and social care needs of people with LD, legislation and the key principles of effective communication. The role and importance of Community LD Teams, Criminal Justice Liaison and Diversion Teams, LD partnership boards, third sector peer advocacy groups and professional advocacy schemes are introduced. There are separate chapters addressing specific issues in police custody, courts, prison and probation services and mention of PSO/PSI relevant to people with LD. There are helpful case studies, Positive Practice examples and a section with Practical Actions in each chapter. There is also a useful list of additional resources at the end of the publication.
NHS England. Betts, N. Equal Access, Equal Care. Guidance for Prison Healthcare Staff treating Patients with Learning Disabilities (2015)
This publication identifies a range of important issues relating to caring for people in prison with LD. It covers the definition of LD, considerations around capacity, common health conditions, social care provision and benefits of specialist LD nurses. Sections 10-13 cover recommendations for healthcare staff relating to assessments and health action planning, reasonable adjustments, communication, care pathways, transitions and partnership working. There are links to useful resources and appendices covering communication tips and a checklist for ‘Gold Standard’ provision.
Public Health England Guidance relating to Learning Disabilities
Public Health England has published a collection of guides on reasonable adjustments for people with a learning disability.
Assessment
National Institute for Health and Care Excellence (2017) Learning disabilities: identifying and managing mental health problems. Quality standard QS142
- There are five quality statements in this quality standard: people with learning disabilities (LD) should have: annual health check, including review of mental health problems
- mental health assessment (if needed) by someone with expertise in mental health problems in LD,
- key worker if learning disability and severe mental illness (SMI)*
- tailored psychological interventions (if required),
- annual documentation of reason for continuing antipsychotic medication (if not stopped).
*SMI: severe depression/anxiety impacting on functioning; psychosis; schizophrenia; bipolar disorder; eating disorder; personality disorder; schizoaffective disorder
NICE guideline: NG54 (2016) Mental health problems in people with learning disabilities: prevention, assessment and management.
The guideline contains advice about communication, capacity, annual health checks and behaviour changes that may assist identification of a mental health problem in a person with LD. It covers assessment with appropriate expertise, and the need to be aware of physical health, sensory or cognitive problems either masking or underlying a mental health issue. It identifies the importance of using adapted or specific tools, risk assessments that include identification of vulnerability and the need for safeguarding protocols, and risk management plans that set out individual, social and environmental interventions to reduce risk. It outlines what should be included in a mental health care plan, adaptations to and specific psychological interventions, pharmacological interventions (to be started only by specialists in mental health/LD) and occupational interventions.
Communication and care
National Institute for Health and Care Excellence (2015, updated 2019) Learning disability: behaviour that challenges. Quality standard QS101
There are 12 quality statements in this quality standard. Behaviour that challenges is defined as: Behaviour of such an intensity, frequency or duration as to threaten quality of life and/or physical safety of the person, or others around them (including behaviour likely to severely limit, or result in being denied access to/use of ordinary community facilities).
Requirements of healthcare providers include: identifying lead practitioner to coordinate care; involving families and carers in developing care/support plan; annual health check with GP to identify physical illness early; initial assessment of behaviour to identify triggers, function and environmental causes of behaviour; opportunities for meaningful personalised daily activities (daily activity schedule, behaviour support plan); access to specialist behavioural support (e.g social care providers, community LD teams links on release); support (planned for release) with choice of housing; documented review of person each time restrictive intervention; ensuring psychosocial interventions 1st line (before use of antipsychotics); ensuring medication review (multi-disciplinary) 12/52 after starting antipsychotics and every 6/12.
Royal College of Nursing (2017) Dignity in health care for people with learning disabilities (3rd Edition)
Developed by the RCN LD Nursing Forum with the input of an expert panel of people with learning disabilities, this guidance is designed to improve dignity in healthcare provision for people with LD. The definition of dignity is broken down into key themes identified by the expert panel: understanding my health; respect me; get to know me; having choices and making decisions; feeling safe; communicating with me. The publication gives examples of good practice and also lists medical problems affecting people with LD more commonly than the general population. There is a list of resources and references and an appendix with a Bill of Rights.
Royal College of Nursing (2017) The needs of people with learning disabilities: what pre-registration students should know, London: RCN
This publication was written to identify competencies required by pre-registration nursing students regarding the health needs of people with a LD.
Nursing in Practice (2017). Norman A. Providing support to people with learning disabilities in primary care
This brief article explains issues affecting people with LD, reasonable adjustments that can be made for their appointments (length, timing, communication, Easy Read written information), common health issues and the importance of patient autonomy.
Public Health England Guidance relating to Learning Disabilities
Public Health England has published a collection of guides on reasonable adjustments for people with a learning disability.
Growing older with learning disabilities
NICE guideline: NG96: Care and support of people growing older with learning disabilities 2018
The NG96 guideline covers the identification of changing needs, planning for the future, and delivering services including health, social care and housing for people growing older with LD. There is guidance about recording actions identified in the annual health check, reasonable adjustments to assist with appointments, and planning for hospital transfers, including the use of a hospital passport. Skills, knowledge and training provision for staff are covered.
NICE: QS187: Learning disability: care and support of people growing older (2019)
There are five quality statements in QS187: Each person growing older with LD should have: a named lead practitioner to co-ordinate care, a person-centred needs assessment, future care planning and reviews, an annual health check (to inform health action plan), a meeting with hospital staff prior to planned admissions (use of hospital passport).
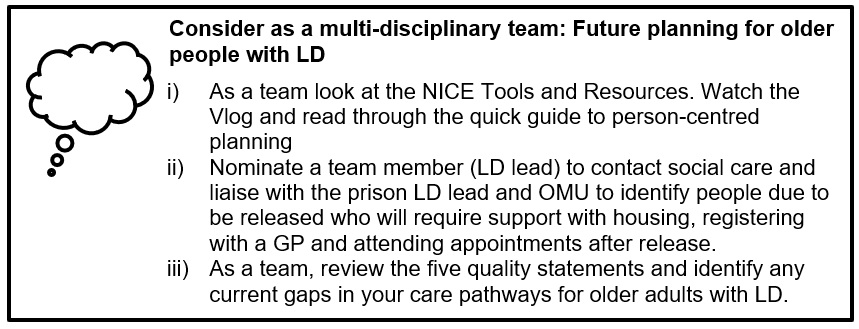
Further resources:
- NICE guideline [NG96]: Care and support of people growing older with learning disabilities
- NICE - Person-centred future planning: A quick guide for practitioners supporting people growing older with learning disabilities
NICE: Support for adults with learning disabilities as they grow older - What to expect
This is a short video for older patients with LD. Below is the link to an Easy Read version of the guideline.
NICE: People growing older with learning disabilities.
Learning disabilities and substance misuse
Public Health England (PHE) Guidance relating to Learning Disabilities
Public Health England has published a collection of guides on reasonable adjustments for people with a learning disability.
PHE: Substance misuse in people with learning disabilities: reasonable adjustments guidance (2016)
This guidance advocates a personalised approach to providing substance misuse services to people with LD, tailoring interventions to meet individual needs, including communication needs. It suggests that people with LD may benefit more from a 1:1 approach rather than group work. In the guidance, there are links to accessible resources for people with LD using substance misuse services.
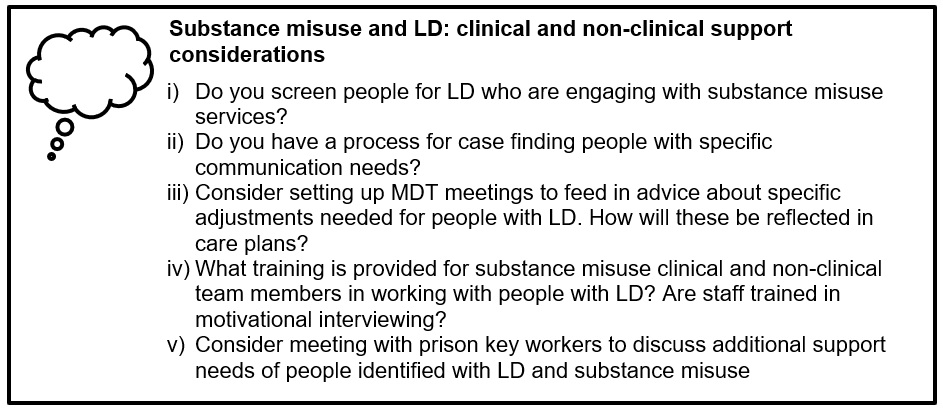
Medication and learning disabilities
PHE: Pharmacy and people with learning disabilities: making reasonable adjustments to services (2017) PHE publications gateway number 2017086HTML
This guidance is useful for pharmacy teams working on site in secure environments and for community pharmacy providers contracted to provide services in secure environments. It includes summarised points for consideration including adjustments to make that will enhance management and monitoring of medicines for people with LD, links to resources provided by RPS and CPPE and case studies with examples of reasonable adjustments.
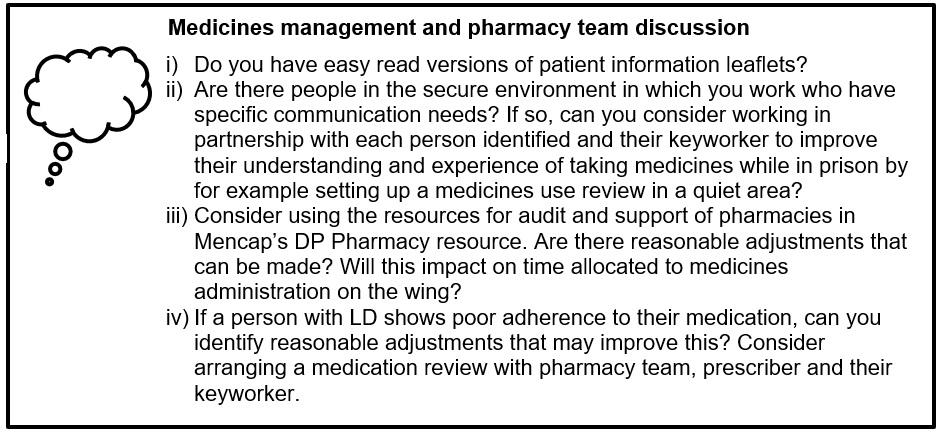
NHS England (2017) Stopping over-medication of people with a learning disability, autism or both (STOMP)
This publication was written to highlight the importance of identifying and reviewing people with learning disability or autism who are prescribed antipsychotic medication in order to reduce and stop inappropriate prescribing for challenging behaviour. It provides an algorithm for review and reduction of antipsychotics, suggestions for practices, examples of practice-wide approaches and individual case studies.
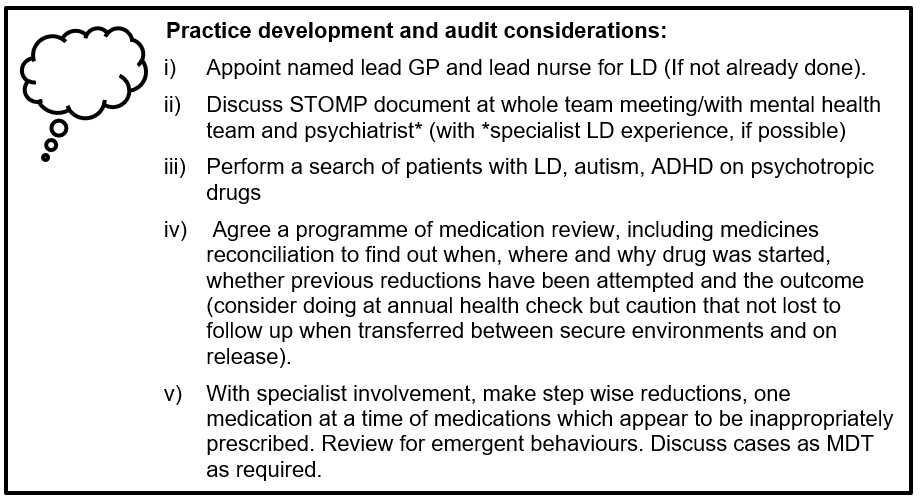
Further resources
Further resources
- Other resources for healthcare professionals produced by Mencap
- Other Resources available from Royal College of Psychiatrists for healthcare professionals
Communication guidance and links
The links below are provided to assist the healthcare team in supporting people with LD who have difficulties with communication, accessing health information and appointments.
- Scope: Communication Access Introduction Cards
- Easy Health
- Change
- How to make information accessible. A guide to producing easy-read documents
- Inspire Services (design and produce Easy Read documents)
- Learning Disability Helpline - Monday to Friday: call 0808 808 1111
- Other Resources available from Royal College of Psychiatrists
- Examples of Easy Read documents in use in the Criminal Justice System
Books Beyond Words
Pictorial resources originally developed for people with learning disabilities to facilitate conversations and explore emotions, the Criminal Justice book set covers 8 topics related to court, prison and crime. There have been further resources developed for people in secure settings during the Coronavirus pandemic, which have been co-authored with RCGP and Michael Emmett, a former service user. These resources are suitable, not only for people with learning disabilities but also for people with low literacy levels and language barriers, and for facilitating conversations and discussing emotions induced by difficult topics. There is a coaching and quick guide suitable for use by clinical and non-clinical prison staff and by peers.
Appendix
Caring for people with learning disabilities: Crib cards
Kindly provided by Ann Norman, Royal College of Nursing
In this section, there are definitions and short explanations that will be useful to share with, for example, nursing students and other health professionals new to working with people with learning disabilities. The 'bite-size' essential information points can be transferred onto crib cards.
What is a learning disability?
A learning disability affects the way a person understands information and how they communicate. Individuals may have difficulty in:
- understanding new or complex information
- learning new skills
- coping independently.
They often have significantly higher health needs, which are commonly unmet and not recognised, and result in premature deaths.
Duty of care
All health services must ensure that reasonable adjustments are made to ensure that people with a learning disability have equal access to health care. Recommended adjustments include:
- information in a format accessible to the person
- longer appointment times
- managing environmental factors
- providing funded additional support
- undertake an assessment of risks and support needs by speaking to the person and others that know them well
Diagnostic over shadowing
This occurs when a clinician attributes symptoms or behaviours to a person’s learning disability rather than another medical cause.
Consent
No-one can consent on behalf of an adult with a learning disability unless they have been appointed as a deputy by the Court of Protection. Parents or support staff should not be asked to consent on the person’s behalf. Instead the Best Interest process must be followed if an individual is assessed as unable to make a decision in line with Mental Capacity Act 2005.
Communication
It is important that you listen to the person, their family members and/or care staff. And ensure information is provided in the person’s preferred format. This may include, easy-read content, large print text, sign language and/or pictures. Review the person’s records to ensure the correct method is used.
Hospital passports
The person using the health service may be able to provide you with their hospital passport which will contain vital information on how best to support them.
Discharge planning
There are many different living arrangements, so no assumptions should be made about the type of support a person receives. Establish where the person lives, who they live with, what support they receive, and what skills their support has. Agree the discharge plan with all who will be involved in supporting them. They may have a health action plan where their discharge health needs can be added. Registered learning disability nurses may be available as hospital liaison nurse or community nurses to offer support and assistance.
Abbreviations:
LD – Learning Disability
NG – NICE Guideline
QS – Quality Standard
PHE – Public Health England
NHS – National Health Service
MCA – Mental Capacity Act
OMU – Offender Management Unit