RCGP Safeguarding toolkit
| Site: | Royal College of General Practitioners - Online Learning Environment |
| Course: | Clinical toolkits |
| Book: | RCGP Safeguarding toolkit |
| Printed by: | Guest user |
| Date: | Tuesday, 3 March 2026, 2:20 AM |
Description
The aim of this toolkit is to enhance the safeguarding knowledge and skills that GPs already have to enable them to continue to effectively safeguard children and young people, as well as adults at risk of harm.
Table of contents
- Introduction
- Key questions in safeguarding
- Part 1: Professional safeguarding responsibilities
- Safeguarding responsibilities as a GP
- Safeguarding roles and responsibilities in general practice
- Safeguarding and personal wellbeing
- Managing concerns and allegations of abuse by colleagues, staff or anyone in a position of trust
- Safeguarding across the four UK nations
- Safeguarding in the independent or online/digital GP sector
- Part 2A: Identification of abuse and neglect
- The rights of children
- Adverse childhood experiences
- Safeguarding young people aged 16 and 17 years old
- Age of consent
- How does child abuse/neglect present in general practice?
- Obstacles to recognising and responding to child abuse and neglect
- Where do children experience abuse and neglect?
- Contextual safeguarding
- Children at greater risk of abuse and neglect
- Children who may be invisible to services
- Looked-after children
- Caring for refugee and unaccompanied asylum seeking children (UASC)
- Perinatal safeguarding
- Unseen men
- Disguised compliance
- Types of child abuse and neglect
- Physical abuse
- Perplexing presentations and fabricated or induced illness (FII)
- Neglect
- Was not brought (children)
- Emotional abuse
- Sexual abuse
- Talking about child sexual abuse
- Working with families affected by child sexual abuse
- Online child sexual abuse and exploitation
- Child sexual exploitation
- Child criminal exploitation and gangs
- Harmful sexual behaviour
- Independent Inquiry into Child Sexual Abuse (IICSA)
- Child trafficking and modern slavery
- Female genital mutilation (FGM)
- Child abuse linked to faith or belief
- Bullying and cyberbullying
- Part 2B: Topics covering both child and adult issues
- Part 2C: Identifying adult abuse and neglect
- Types of adult abuse
- Physical abuse
- Sexual abuse
- Psychological or emotional abuse
- Financial or material abuse
- Modern slavery
- Discriminatory abuse
- Neglect and acts of omission
- Self-neglect
- Organisational abuse
- Adults at greater risk of abuse and neglect
- How does adult abuse/neglect present in general practice?
- Safeguarding those who are homeless
- Was not brought (adult)
- Part 3A: Responding to abuse and neglect
- Part 3B: Responding to concerns about child abuse
- Part 3C: Responding to concerns about adult abuse
- Part 3D: Contributing to the lifelong holistic care of victims and survivors of abuse
- Part 3E: Responding to allegations of abuse regarding staff or persons in a position of trust (PiPoT)
- Part 4: Documenting safeguarding concerns and information
- Part 5: Information Sharing and multiagency working
- Guidance on information sharing
- What does ‘information sharing’ in a safeguarding context mean?
- The challenges of information sharing in general practice
- Why do we need to share information?
- When should we share information?
- What information should we share?
- Who should we share information with, and how?
- Information sharing and the law
- Consent
- Legal considerations for sharing personal information
- APPENDIX 1: Information sharing advice and guidance
- References
- Acknowledgements
Introduction
Welcome to the RCGP Safeguarding toolkit. This toolkit builds on the previous RCGP Child Safeguarding toolkit and RCGP Adult Safeguarding toolkit and combines both into one toolkit, aligned with the new RCGP Safeguarding Standards. The new standards are a whole-life course document covering both child and adult safeguarding, recognising that there are overlapping knowledge and capabilities in general practice.
Safeguarding in general practice has evolved significantly in recent years. General practice is a key partner in the multi-agency arena of safeguarding. Safeguarding can only be effective when professionals and agencies work together in partnership. Across the four UK nations, there are many similarities in safeguarding practice. There are, however, different legislations and local processes. This toolkit covers core knowledge that is applicable to all four nations and outlines some of the key differences in each nation. However, all practitioners need to be aware of the legislation, guidance and processes as it applies in their UK nation, which are highlighted later in this section.
Safeguarding in general practice can be defined as:
Contributing to the protection of children and adults from abuse and neglect using the specific skills, resources and capacity available in general practice by:
- implementing professional safeguarding responsibilities which includes continual professional development in safeguarding
- preventing abuse and neglect
- identifying abuse and neglect
- responding appropriately to abuse and neglect, including supporting victims and survivors of abuse
- having governance systems and processes in place to support safeguarding
- working collaboratively with other health colleagues, safeguarding partners and agencies.
The aim of this toolkit is to enhance the safeguarding knowledge and skills that GPs already have to enable them to continue to effectively safeguard children and young people, as well as adults at risk of harm.
Intended audience
This toolkit is for any GP or GP specialty trainee working in general practice in the UK and will also be useful for any practitioner working in general practice. Everyone is at a different stage in their GP career. For those who are new to general practice, or general practice in the UK, we recommend first completing the RCGP eLearning course on Core safeguarding in general practice (Level 3). These modules provide an overview of safeguarding in general practice in the UK and will also be useful to any practitioner as a safeguarding update or refresher. Completing the modules, along with the essential reading list below, will provide a solid background in safeguarding.
Essential reading list
This reading list is essential in understanding the principles of adult and child safeguarding, and should form part of your core knowledge around safeguarding:
- GMC. Protecting children and young people: The responsibilities of all doctors. 2018.
- GMC. Ethical hub - Adult safeguarding. Updated 2024.
- GMC. Good medical practice. 2024.
- Information Commissioner’s Office. A 10 step guide to sharing information to safeguard children. 2023.
- RCGP. GP online services toolkit. The GP online services toolkit contains a section on safeguarding challenges of online patient access. This is an essential read for anyone working in general practice where there is patient online access.
Key questions in safeguarding
These key questions link summary information from the toolkit to provide easily accessible information.
Presentations of child and adult abuse and neglect in general practice are seldom clear-cut and well-defined. Both children and adults can experience different types of abuse at the same time. There are many similarities to the presentations of different types of abuse, such as change in behaviour, mental health difficulties including self-harm, drug and alcohol use, disturbed sleep, and physical symptoms and signs.
Identifying abuse and neglect is not always easy. Knowing the signs of the different types of child and adult abuse helps to be able to identify possible concerns about abuse and neglect, as well as giving a voice to children and adults who are experiencing abuse.
Part 2 of the toolkit outlines the different types of abuse that children and adults can experience and how these might present in general practice. There are many signs that are common indicators of many different types of abuse such as behaviour changes and mental health concerns. Identification of any signs of abuse should prompt further exploration using professional curiosity.
Always keep abuse and neglect in mind as a potential cause for any reason a patient may present in general practice.
Responding to concerns about child abuse.
There are five steps to take. These are summarised here with further information and guidance in Part 3 of the toolkit.
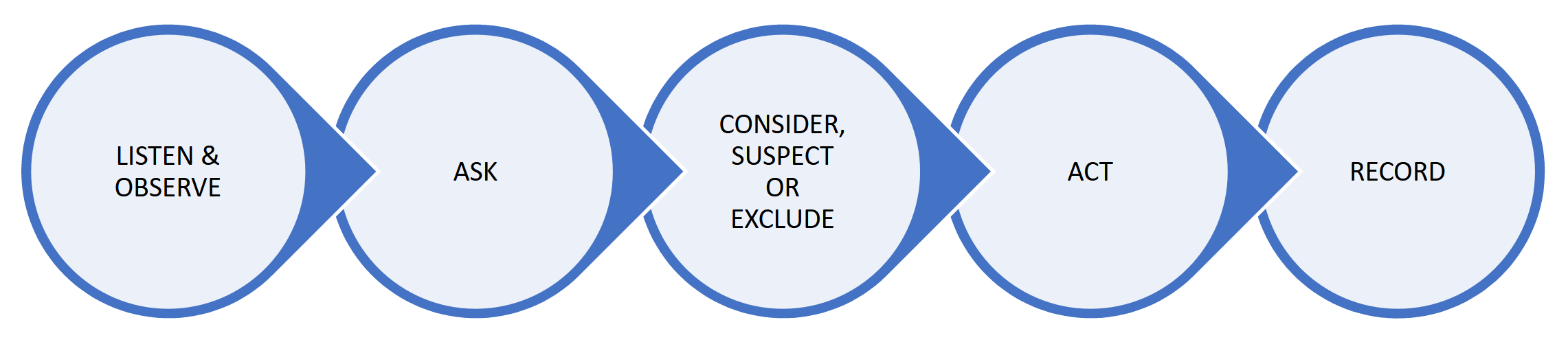
- Step 1. Listen and observe. Piece together any information you already have about that child and family.
- Step 2. Ask. Seek an explanation for any injury, presentation or concern from both the parent or carer and the child/young person (if possible, dependent on age, communication needs, disabilities).
-
Step 3. Consider, suspect or exclude abuse or neglect:
- Consider – child abuse is one possible explanation for the concerns and is included in your differential diagnosis.
- Suspect – you have a serious level of concern about the possibility of child abuse (you do not need to have proof).
- Exclude – a suitable explanation is found for your concern.
-
Step 4. Act.
- If you suspect child abuse, you should follow your local multi-agency safeguarding processes and make a safeguarding referral to children’s social care/Health and Social Care Trust (Northern Ireland).
- If you are considering child abuse, you should decide on what further action needs to be taken, such as gathering further information, discussing your concerns and arranging review of the child.
- If you have excluded child abuse at this time, you should continue to exercise professional curiosity and be prepared to once again consider or suspect child abuse should the situation change, or new information come to light.
- Step 5. Record. Ensure clear documentation in the child’s record (and that of any other family member as appropriate). Mark entries ‘not for online access’.
Responding to concerns about adult abuse.
There are five steps to take. These are summarised here with further information and guidance in Part 3 of the toolkit.
- If you are unsure, seek further advice from a colleague, your organisational safeguarding lead or local safeguarding professionals.
- Ensure the patient is safe and deal with any immediate medical needs.
Is the adult an 'adult at risk/adult at risk of harm'?
YES: consider an adult safeguarding referral and follow steps 4 & 5 below.
NO: consider:- other sources of support for the adult
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation if new relevant information comes to light
- Continue to monitor the situation as risk and the ability to safeguard themselves may change over time.
Does the adult at risk of harm have capacity to make a decision about a safeguarding referral?
NO: proceed with an adult safeguarding referral.
YES and they consent to a referral: proceed with an adult safeguarding referral.
YES but they do not consent to a referral: consider:- whether they need more information on the safeguarding adult process, which might address any concerns they have
- what other sources of support are available
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation at appropriate intervals as risk can change as can an adult’s ability to protect themselves.
- reassess the situation if new relevant information comes to light
UNCERTAIN: discuss with a colleague, your organisational safeguarding lead or local safeguarding professionals.
NOTE FOR PRACTITIONERS WORKING IN WALES – all practitioners working in Wales should be aware of the statutory ‘duty to report’.
- The practice/organisation safeguarding lead.
- A more experienced colleague.
- The Caldicott Guardian or Data Protection Officer if you need advice about information sharing.
- Local safeguarding professionals such as Named GPs/Nurses for Safeguarding, Designated Health Professionals, safeguarding leads within health boards.
- Social worker – you can contact your local authority/Health and Social Care Trust by phone and ask to speak to the duty social worker if you have an urgent safeguarding concern. You can find these numbers on the safeguarding section on the website of your local authority, or in Northern Ireland, your local Health and Social Care Trust.
- The phone numbers for your local safeguarding professionals, local authority, Health and Social Care Trust (Northern Ireland), should be clearly displayed and easily accessible within your organisation.
- For practitioners in England, the NHS Safeguarding App is an easy way to find your local authority details. It can be accessed by visiting your device’s appropriate app store and searching for ‘NHS Safeguarding’.
Information sharing is essential to safeguarding children and adults.
Sharing information in a safeguarding context means sharing relevant personal information about children and adults that multi-disciplinary and multi-agency professionals and agencies hold. The information is shared in order to safeguard children and adults from abuse and neglect.
Below are the key principles of information sharing and a summary of the ‘Why, When, Who, What and How’ of information sharing. Further guidance, including on issues around consent, can be found in Part 5 of the toolkit.
You can also find more guidance on making child and adult safeguarding referrals in Part 3 of the toolkit (if needed).
Summary of the ‘Why, When, Who, What and How’ of information sharing for the purposes of safeguarding:
When there is a concern that a child is at risk of, or is experiencing, abuse or neglect.
When there is a concern that an adult is at risk of, or is experiencing, abuse or neglect and one of the following:- It is required by law.
- The adult provides consent for the information to be shared.
- The adult does not have the capacity to provide consent for the information to be shared.
- It is in the public interest, i.e. there are others at risk of serious harm, or it is necessary to share information to prevent a serious crime or there is an imminent risk of serious harm to the individual.
Information can also be shared when safeguarding advice is being sought – this can often be done without sharing the names or other identifying features of the patient involved.
- General practice multi-disciplinary team.
- Wider health multi-disciplinary team.
- Multi-agency safeguarding partners.
- Other relevant agencies as appropriate.
- High quality documentation of safeguarding information is fundamental to safeguarding children and adults in order to:
- ensure victims and survivors of abuse have the healthcare and support they need
- allow a picture to be built over time of emerging concerns
- manage and share information about risk appropriately
- allow for effective information sharing when required
- allow for discussions with patients about online access where there are safeguarding concerns.
- Experiencing abuse and/or neglect as a child or adult has significant implications on health and wellbeing so therefore needs to be documented.
- All safeguarding information should be stored within the medical record, not separate to it.
- Any documents containing third party information should be flagged as such with the appropriate code.
- It is not necessary to black out information within safeguarding documents before putting into the patient record.
- The use of coding to record key safeguarding information is important to be able to easily find the relevant information when needed in the future or for audit purposes.
- Safeguarding information should be managed safely to reduce the risk of perpetrators using any disclosures of abuse from victims (or any information in the medical record) to further abuse them.
- If any member of staff is unsure how to manage safeguarding information, they should always seek advice from the practice safeguarding lead/Caldicott Guardian/Information Governance lead/Data Protection Officer.
- All safeguarding information should be redacted from patient online access and clearly marked ‘not for online access’.
Further information and guidance on documenting and coding safeguarding information.
Having knowledge of local safeguarding policies and procedures is essential to effective safeguarding. This table outlines the knowledge you need so that you can take prompt safeguarding action when necessary. Please access the downloadable version of the table (DOCX).
How do I contact them?
How do I contact them?
Safeguarding learning is a continual process and enables us to have the knowledge and capabilities to safeguard our patients.
The RCGP Safeguarding Standards set out the professional safeguarding standards and safeguarding training requirements for GPs and anyone working in any general practice setting in the UK. This includes, but is not limited to, NHS GP practices, independent and online providers of general practice services, Primary Care Networks (PCNs), GP out of hours and extended access services. The standards combine and include both safeguarding children and adults and are a whole life course document. These standards form part of the wider intercollegiate documents on safeguarding knowledge and competencies for all healthcare staff.
It is important to note that both adult and child safeguarding knowledge and capabilities are equally necessary and expected for all staff in general practice, even if the staff member only works with adults.
The RCGP Safeguarding Standards set out five key areas of safeguarding knowledge and capabilities, shown here.
- Understanding statutory, legal, professional and employment safeguarding responsibilities and duties, including the obligation to act when there is a safeguarding concern.
- Preventing abuse and neglect as far as possible through timely action and intervention.
- Accounting for the influence of personal beliefs, experience and attitudes.
- Maintaining individual wellbeing.
- Supporting colleague wellbeing.
- Recognising indicators and signs of all types of abuse and neglect in children and adults.
- Identifying children and adults who may be more vulnerable to abuse and neglect.
- Applying principles of consent, confidentiality and capacity in relation to safeguarding.
- Mitigating barriers to healthcare faced by victims and survivors of abuse.
- Understanding the lifelong impact of abuse.
- Learning from those with lived experience of abuse.
- Practising in a trauma-informed way.
- Applying relevant legislation.
- Being vigilant and addressing organisational/institutional abuse/neglect.
- Acting when there is a safeguarding concern.
- Talking to children, adults, families, parents and carers about abuse.
- Following local referral processes for child and adult safeguarding.
- Contributing to the lifelong holistic care needed by victims and survivors of abuse.
- Seeking advice and guidance and escalating concerns when necessary.
- Promptly acting on, and responding appropriately to, any concerns or allegations about persons in a position of trust.
- Documenting safeguarding concerns accurately and safely in the patient record.
- Managing safeguarding documents in line with best practice in information governance and data protection.
- Proactively addressing safeguarding challenges of patient online access including coercion to access records.
- Participating in multi-agency and multi-disciplinary working.
- Sharing information appropriately and proactively in a safeguarding context.
- Contributing to safeguarding reviews.
- Learning from safeguarding serious case reviews (local and national).
This table gives a summary of the safeguarding training requirements as set out in the RCGP Safeguarding Standards for GPs and anyone working in a general practice setting in the UK. Also see ‘RCGP safeguarding standards for general practice’.
- Receptionists, administrative and secretarial staff (with the exception of manager/lead roles of these groups who will need level 2).
- Volunteer staff.
- Safeguarding included in practice/organisation induction AND completion of relevant safeguarding level 1 eLearning updates.
- Level 1 safeguarding update.
- Practice managers (including deputy managers) and equivalent leadership roles. [ALSO SEE ADDITIONAL REQUIREMENTS FOR THIS GROUP]
- Care navigators.
- Reception managers.
- Safeguarding administrators.
- Managers/leads of administrative/secretarial teams.
- Health care assistants, pharmacy technicians.
- Safeguarding included in practice/organisation induction AND completion of relevant safeguarding level 2 eLearning updates.
- Complete relevant safeguarding level 2 eLearning modules.
- Have a safeguarding induction with an appropriate senior leader e.g. practice manager/practice safeguarding lead depending on nature of role. This induction should include:
- discussion about the safeguarding structure, policies and procedures within the practice/organisation
- identification of any areas of professional development related to safeguarding.
- Level 2 safeguarding update
- GPs, practice nurses, physician associates, nursing associates, pharmacists, paramedics, Advanced Care Practitioners, Advanced Nurse Practitioners, social prescribers, mental health workers, physiotherapists, podiatrists, dieticians and any similar ARRS (Additional Roles Reimbursement Scheme) roles.
- Primary care network (PCN) safeguarding roles in England such as PCN safeguarding co-ordinators.
- GP speciality trainees [who should refer to the specific safeguarding training requirements for the workplace based assessment (WBPA) part of the MRCGP exams]
- Safeguarding included in practice/organisation induction.
- Completion of relevant safeguarding level 3 eLearning updates (or provide evidence of prior completion) e.g. RCGP modules.
- Meet with the practice/organisational safeguarding lead, their deputy, or other relevant senior leader within one month of starting their new role to:
- discuss the safeguarding structure, policies and procedures within the practice/organisation
- identify any areas of professional development need related to safeguarding.
- Level 3 safeguarding update.
- Completion of the Safeguarding Structured Reflective Template to demonstrate reflection and learning across the breadth of all the five areas of safeguarding knowledge and capabilities. This must include both child and adult safeguarding issues, even if a practitioner only works with adults.
Annually:
- Safeguarding update.
- Demonstrate regular attendance at the local practice safeguarding lead forums (if available in the locality).
- Demonstrate an example of reflection/learning aligned with the practice/organisational role specific knowledge and capabilities.
- The practice/organisation safeguarding lead.
- A more experienced colleague.
- Caldicott Guardian or Data Protection Officer, if you need advice about information sharing.
- Local safeguarding professionals such as Named GPs/Nurses for Safeguarding, Designated Health Professionals, or safeguarding leads within health boards.
- Social worker – you can contact your local authority (Health and Social Care Trust in Northern Ireland) by phone and ask to speak to the duty social worker if you have an urgent safeguarding concern.
For those who are new to general practice, or general practice in the UK, we recommend first completing the RCGP eLearning course - Core Safeguarding in General Practice (Level 3). These modules provide an overview of safeguarding in general practice in the UK and will also be useful to any practitioner as a safeguarding update or refresher. Completing the modules, along with the essential reading list, will provide a solid background in safeguarding.
When you have completed the eLearning modules and the essential reading list, you will have a great foundation in safeguarding that you can build throughout your career in UK general practice. See ‘What safeguarding training do I need?’ above for further information on training requirements.
- A resource for busy GPs and general practice staff to refer to when they need safeguarding support or are unsure of what steps to take when they have a safeguarding concern about an adult or child.
- An educational resource to support the building and development of safeguarding knowledge and capabilities. Some practitioners might dip in and out of the toolkit when they need to, others may read through it systematically over time to support their safeguarding learning.
- A resource for practice safeguarding leads to use to support safeguarding learning and reflection in their organisation.
There are five parts to the toolkit – these match the five different key areas of safeguarding knowledge and capabilities set out in the RCGP Safeguarding Standards. Contents of the toolkit are summarised below:
- Essential reading list.
- Safeguarding roles and responsibilities in general practice.
- Safeguarding and personal wellbeing.
- Summary of relevant safeguarding legislation and guidance in each UK nation.
- Identifying child abuse and neglect:
- the rights of children
- adverse childhood experiences (ACEs)
- safeguarding young people aged 16 and 17 years old
- age of consent, Fraser guidelines and Gillick competence
- how does child abuse/neglect present in general practice?
- obstacles to recognising and responding to child abuse and neglect
- where do children experience abuse and neglect
- contextual safeguarding
- children at greater risk of abuse and neglect
- children who may be invisible to services
- looked after children
- caring for refugee and asylum seeking children
- perinatal safeguarding
- unseen men
- disguised compliance
- types of abuse and neglect (including Was Not Brought).
- Radicalisation (covers child and adults).
- Domestic abuse (covers child and adults) including ‘honour’ based abuse and forced marriage.
- Transitional safeguarding.
- Identifying adult abuse and neglect:
- human rights based approach
- principles of safeguarding
- types of abuse and neglect
- organisational abuse including safeguarding in care homes
- adults at greater risk of abuse and neglect
- how does adult abuse/neglect present in general practice
- safeguarding those who are homeless
- Was not brought.
- How should we respond when we have concerns that a child or adult is experiencing abuse or neglect?
- Responding appropriately and effectively in general practice to concerns about abuse.
- Talking to children, adults, families and carers about abuse.
- Trauma-informed practice.
- Responding to concerns about child abuse:
- the child’s voice
- five-step process to responding to concerns about child abuse and neglect:
- listen and observe
- ask
- consider, suspect or exclude
- act
- document
- early Help
- making a child safeguarding referral
- top tips for making a child safeguarding referral and writing safeguarding reports– The 5 Cs
- working with parents and carers when there are safeguarding concerns about their children/the children they care for
- child protection system in the UK.
- Responding to concerns about adult abuse:
- five-step process to responding to concerns about adult abuse and neglect:
- concern about abuse
- the views of the adult
- is the adult an ‘adult at risk of harm’?
- assessing mental capacity (includes mental capacity principles, decisional and executive capacity, ‘unwilling’ or ‘unable’ to safeguard, assessing capacity in complex situations and in self-neglect, giving medication covertly
- is a safeguarding referral needed?
- what should happen if an adult at risk of harm has capacity but does not want any safeguarding procedures and is unwilling to take steps to safeguard themselves
- making safeguarding personal
- making an adult safeguarding referral
- top tips for making an adult safeguarding referral and writing safeguarding reports – the 5 Cs
- adult safeguarding processes.
- five-step process to responding to concerns about adult abuse and neglect:
- Contributing to the lifelong holistic care of victims and survivors of abuse.
- Responding to allegations of abuse regarding staff or persons in a position of trust (PiPoT).
- Documenting and coding safeguarding information in the electronic medical record.
- Key principles of documenting safeguarding concerns and information in the patient electronic medical record.
- Who is responsible for managing safeguarding information in the practice/organisation?
- What is ‘safeguarding information’?
- Sources of safeguarding information.
- Recording family groups/relationships.
- Domestic abuse – specific guiding of domestic abuse and MARAC information.
- Recording adult drug and alcohol problems, mental health problems and learning disabilities.
- ‘Was not brought’.
- Management of child protection conference invitations, reports (including those provided by general practice and those received) and minutes.
- Management of adult safeguarding conference invitations, reports(including those provided by general practice and those received) and minutes.
- Contextual safeguarding situations.
- Information about perpetrators of abuse.
- Codes to use.
- Managing safeguarding information in the context of patient online access.
- Key principles of information sharing.
- The challenges of information sharing.
- The why, when, who, what and how of information sharing.
- Information sharing and the law.
- Consent.
These two templates have been developed to support safeguarding learning and reflection. They can be used to support annual appraisal as well as revalidation.
Part 1: Professional safeguarding responsibilities
This section covers the safeguarding responsibilities for all those working in general practice in the UK as well as outlining specific safeguarding roles in general practice.
Safeguarding responsibilities as a GP
Safeguarding duties and responsibilities for all doctors working in the UK, including GPs, are set out by the General Medical Council (GMC).
The GMC highlights the importance of safeguarding in their guidance for doctors; all GPs should be familiar with, and follow, these professional standards. The GMC standards with particular relevance to safeguarding are:
- Good medical practice. 2024.
- Confidentiality: good practice in handling patient information. Updated 2018.
- Protecting children and young people: the responsibilities of all doctors. Updated 2018.
- 0 – 18 years: guidance for all doctors. Updated 2018.
- Adult safeguarding ethical hub (this ethical hub shows how the GMC professional standards can be applied in adult safeguarding).
Good medical practice 2024 includes the following guidance on safeguarding:
“Safeguarding children and adults who are at risk of harm
- You must consider the needs and welfare of people (adults, children and young people) who may be vulnerable, and offer them help if you think their rights are being abused or denied. You must follow our more detailed guidance on Protecting children and young people and 0-18 years: guidance for all doctors.
- You must act promptly on any concerns you have about a patient – or someone close to them – who may be at risk of abuse or neglect, or is being abused or neglected.”
Safeguarding roles and responsibilities in general practice
Everyone in the practice team has a responsibility for safeguarding and each member plays a crucial role. The RCGP Safeguarding Standards outline the safeguarding knowledge and capabilities for GPs and anyone working in any general practice setting in the UK.
All regulated clinical staff have safeguarding roles and responsibilities set out in guidance from relevant professional regulators (for example, General Medical Council, Nursing and Midwifery Council, General Pharmaceutical Council, Health & Care Professions Council). All staff should have their safeguarding duties and responsibilities outlined in their terms of employment.
Practice Safeguarding Lead
All practices should have a Practice Safeguarding Lead. The specifics of this role are outlined in the RCGP Safeguarding Standards document. There may also be a Deputy Safeguarding Lead (practices in England should be aware that ‘Working Together to Safeguard Children 2023: statutory guidance’ states that: "GP practices should have a lead and deputy lead for safeguarding, who should work closely with the named GP ”*). The role of the safeguarding lead is to support safeguarding within the practice, not to manage all safeguarding activity.
*Named GPs only exist in England and are GPs employed by an ICB (Integrated Care Board) to advise and support GP practice safeguarding leads (Working Together to Safeguard Children 2023: statutory guidance).
Practice managers
Practice managers play a crucial role in safeguarding in general practice by demonstrating safeguarding leadership, embedding safeguarding culture, and in particular, ensuring safe recruitment processes. The safeguarding specifics of this role are outlined in the RCGP Safeguarding Standards document.
Safeguarding Administrators
Practices should consider having a Safeguarding Administrator (practices use different terms) – this is a member of the Practice administrative team who, depending on size of practice and structure, either manages or oversees, the recording and coding of safeguarding information coming in and out of the practice. The role of safeguarding administrator does not need to be the individual’s sole role, but someone in the administrative team with the appropriate safeguarding knowledge, capabilities and responsibility. The safeguarding administrator should receive ongoing training and support for their role as set out in the RCGP Safeguarding Standards.
Safeguarding support roles
As practices evolve, and with the establishment of Primary Care Networks (PCNs) in England, there has been development of safeguarding support roles, such as safeguarding co-ordinators, within practices/PCNs. This role can be extremely varied depending on the background and experience of the individual which can range from an administrative role within a current practice structure to a safeguarding nurse employed by a number of PCNs.
The principle of the role is to support safeguarding work in primary care.
Practices/PCNs should be aware that safeguarding support roles in primary care:
- Are new, therefore caution, time and patience are needed with their development and integration.
- Are only one part of safeguarding practice and culture in primary care – safeguarding remains the responsibility of ALL staff members.
- Are an addition to current safeguarding practice and culture in primary care, not a replacement.
- Have no national standard as the role varies between practices and PCNs.
- Are recruited from a wide variety of individuals therefore experience and ability varies hugely.
- Will need significant supervision and guidance from the practice safeguarding lead and other relevant senior practice team members in line with their role, learning needs and expectations of the practice.
- Should not make any clinical or safeguarding decisions.
- Should have a clear job role with clear governance and escalation processes embedded.
- Should have the appropriate indemnity for their role.
The role can include:
- Managing the safeguarding diary of child protection and adult safeguarding conferences to support timely report completion and also to maximise GP attendance at these conferences where possible.
- Assisting GPs with preparation of safeguarding reports for safeguarding meetings and conferences e.g completing demographics and factual information such as missing vaccinations, ‘was not brought’ information, outstanding health referrals.
- There should be robust supervision and governance structures in place within the practice regarding the preparation of reports to ensure appropriate, relevant and proportionate information is shared
- Administrative staff should not interpret clinical information within a record for the purpose of a safeguarding report
- The responsibility of the completion of safeguarding reports remains with GPs
- Supporting with safeguarding coding from safeguarding documents coming into the practice.
- Liaison with patients/families regarding any outstanding health issues raised through safeguarding conferences, e.g. liaising with parents to book appointments for a child’s health needs (such as vaccinations or health reviews) when a child is on a child protection plan.
- Maintain up to date registers/coding of children on child protection plans and looked after children.
- Help to support clinicians following up children and adults who are not brought to appointments. For example, by contacting them and arranging another appointment.
- Co-ordinate practice safeguarding meetings.
- Collate and maintain staff safeguarding training registers.
- Work closely with the practice safeguarding lead and practice manager.
At this current time, given the infancy of safeguarding support roles, it is generally not appropriate for individuals in these roles to attend child or adult safeguarding conferences/strategy meetings for the following reasons:
- Children and adults at risk of harm who are subject to child protection /adult safeguarding conferences are some of our most vulnerable patients. These conferences can be extremely difficult for families/adults and it is essential they are treated with respect.
- There are no ‘‘observational’ roles at a safeguarding conference. Every professional there must actively participate in the discussions and decision making.
- Professionals present need to be able to analyse, understand and interpret the information presented by all agencies as well as by the child/family/adult/carers.
- Professionals present need to be able to understand a wide range of risks involved in the situation and partake in any risk assessments.
- The professional representing primary care needs to be able to explain and interpret health information to non-health professionals, including the patient/family/carers.
- Professionals need to be able to respectfully challenge other agencies/professionals if appropriate and need to have sufficient authority to do so. They also need to be able to respond to respectful challenge towards themselves, their colleagues or their organisation.
Safeguarding and personal wellbeing
Safeguarding is part of the holistic care given to patients in general practice and it can be very rewarding to be involved in preventing and stopping abuse happening. However, there is no doubt that being involved in safeguarding can be professionally and personally challenging. Safeguarding requires us as professionals to ‘think the unthinkable’ which can make us feel very uncomfortable, especially as GPs, when trust, empathy and compassion are key to our therapeutic relationships with patients. Being involved in safeguarding cases or hearing personal experiences of abuse from patients can be very upsetting. There is also emotional complexity involved as in general practice we provide care for both victims and perpetrators of abuse. This complexity can be magnified by the contextual experiences of perpetrators of abuse who have their own experiences of being a victim of abuse. A key element of a GP’s role has always been to be an advocate for patients. This role can be conflicted when a patient is causing harm to others and this can be challenging to deal with.
In addition, for any healthcare professional who is a victim or survivor of abuse themselves, professionally having to deal with concerns about abuse to children or adults can be very difficult and can trigger unwanted memories and emotions.
Talking to colleagues can be very helpful – whether this is to simply debrief after a difficult consultation or experience, or to seek advice and guidance. Support, advice and guidance can also be sought from the practice safeguarding lead and/or local safeguarding professionals such as named GPs/nurses, Designated Health Professionals or safeguarding leads within health boards.
The most important thing to remember is that no practitioner has to deal with difficult safeguarding issues alone – there is always help available.
There are lots of resources available for your own wellbeing. The links below are for national organisations, you may also have sources of local support such as through your practice/organisation, your GP, local agencies who support victims and survivors of abuse or via your LMC (Local Medical Committees).
- GMC. Wellbeing resources for doctors. 2022.
- BMA. Your wellbeing. 2024.
- NHS. Practitioner Health. 2024. Practitioner Health is a free, confidential NHS primary care mental health and addiction service with expertise in treating health and care professionals.
- NAPAC. Supporting Recovery From Childhood Abuse. 2023. The National Association of People Abused in Childhood: supports adult survivors of any form of child abuse.
- The Survivors Trust. Homepage of The Survivors Trust. Supporting victims and survivors of sexual violence.
- Refuge. Homepage of National Domestic Abuse Helpline. Supporting victims and survivors of domestic abuse.
Managing concerns and allegations of abuse by colleagues, staff or anyone in a position of trust
This is covered in Part 3 of the toolkit: Responding to abuse and neglect.
Safeguarding across the four UK nations
Safeguarding responsibilities apply to everyone working in healthcare in all of the four UK nations. Each nation has their own safeguarding legislation and guidance which all staff in general practice should be aware of in the nation in which they work. Key legislation and guidance for each UK nation are shown below.
England
Legislation
- Children Act 1989.
- Female Genital Mutilation Act 2003.
- Children Act 2004.
- Mental Capacity Act 2005.
- The Care Act 2014.
- Children and Social Work Act 2017.
- Domestic Abuse Act 2021.
Further details about child protection legislation and guidance in England regarding children can be found on the NSPCC website.
Guidance
- Department for Education. Working together to safeguard children. Updated 2024.
- HM Government. What to do if you’re worried a child is being abused. Advice for practitioners. 2015.
- Home Office. Mandatory Reporting of Female Genital Mutilation – procedural information. 2016.
- HM Government. Multi-agency statutory guidance on female genital mutilation. 2020.
- Department of Health and Social Care. Care and support statutory guidance. Updated 2024.
- Department for Constitutional Affairs. Mental Capacity Act 2005. Code of Practice. 2007.
- Department for Education. Information Sharing. Advice for practitioners providing safeguarding services for children, young people, parents and carers. 2024.
Northern Ireland
Legislation
- The Children (Northern Ireland) Order 1995.
- Female Genital Mutilation Act 2003.
- The Safeguarding Vulnerable Groups (Northern Ireland) Order 2007.
- Safeguarding Board Act (Northern Ireland) 2011.
- Children’s Services Co-operation Act (Northern Ireland) 2015.
- Mental Capacity Act (Northern Ireland) 2016 and Mental Capasity Act (Northern Ireland) 2016 by Department of Health.
Further details about child protection legislation and guidance in Northern Ireland regarding children can be found on the NSPCC website.
Guidance
- Safeguarding Board for Northern Ireland. Procedures Manual. Updated 2023.
- Department of Health, Social Services and Public Safety and and the Department of Justice. Adult Safeguarding: Prevention and Protection in Partnership. 2015.
- Multi-agency practice guidelines: Female Genital Mutilation.
Scotland
Legislation
- Adults with Incapacity (Scotland) Act 2000.
- Prohibition of Female Genital Mutilation (Scotland) Act
- The Adult Support and Protection (Scotland) Act 2007).
- Children and Young People (Scotland) Act 2014.
- United Nations Convention on the Rights of the Child (Incorporation) (Scotland) Act 2024.
Further details about child protection legislation and guidance in Scotland regarding children can be found on the NSPCC website.
Guidance
- Scottish Government. Adult Support and Protection (Scotland) Act 2007: guidance for General Practice. 2022.
- Scottish Government. Adult Support and Protection (Scotland) Act 2007: Code of Practice. 2022.
- Scottish Government. Adults with incapacity: guide to assessing capacity. 2008.
- Scottish Government. NHS Public Protection Accountability and Assurance Framework. 2022.
- Scottish Gorvernment. Getting it right for every child (GIRFEC) - Statutory Guidance - Assessment of Wellbeing 2022 – Part 18 (section 96) of the Children and Young People (Scotland) Act 2014. 2022.
- Scottish Government. National Guidance for Child Protection in Scotland 2021. Updated 2023.
- Scottish Government. Responding to female genital mutilation: multi-agency guidance. 2017.
- National Trauma Transformation Programme. Homepage of NTTP. Responding to Psychological Trauma in Scotland.
- National Adult Support and Protection Coordinator. Adult Support and Protection: Scotland. Seven minute briefing. 2024.
Centre for Excellence for Children’s Care and Protection. Child Protection: Scotland. Seven minute briefing. 2025.
Wales
Legislation
- Children Act 1989.
- Female Genital Mutilation Act 2003.
- Children Act 2004.
- Mental Capacity Act 2005.
- Social Services and Well-being (Wales) Act 2014.
- Violence against Women, Domestic Abuse and Sexual Violence (Wales) Act 2015.
Further details about child protection legislation and guidance in Wales regarding children can be found on the NSPCC website.
Guidance
- Social Care Wales. Wales Safeguarding Procedures. 2024.
- Welsh Government. Social Services and Well-being (Wales) Act 2014. Working Together to Safeguard People: Code of Safeguarding Practice. 2022.
- Welsh Government. Safeguarding Guidance. Updated 2024.
- Home Office. Mandatory Reporting of Female Genital Mutilation – procedural information. 2016.
- HM Government. Multi-agency statutory guidance on female genital mutilation. 2020.
- Department for Constitutional Affairs. Mental Capacity Act 2005. Code of Practice. 2007.
Safeguarding in the independent or online/digital GP sector
Patients can choose to be seen via the NHS or via the independent sector, or in combination with the independent health appointments forming a 'complimentary service'. Some patients will elect for all of their care to be in the independent sector. There are also online/digital providers of GP services.
Legal and professional responsibilities around safeguarding are the same regardless of whether the healthcare setting is an NHS or non-NHS/independent/online/digital setting. For doctors, the GMC professional standards apply regardless of the healthcare setting.
GPs working in the independent or online sectors can face additional challenges in safeguarding patients due to:
- Limited access to patients' NHS GP and hospital health records.
- Patients may decline to share information regarding private consultations with their NHS GP which can lead to concerns and problems.
- Unverified information being provided such as demographic information which may not be genuine because it is not always cross checked. This means that patients can 'disappear' or be hard to trace.
- Less reliable computer systems to code non-attendance or 'was not brought' and other issues that might raise safeguarding suspicions. Multiple non-attendances are less likely to be flagged as a potential safeguarding issue.
- Multi-agency safeguarding information is not routinely shared with the independent sector.
- There may not be clear processes for reporting safeguarding concerns. This can be a particular issue for online providers who may see patients from across the UK.
- Families not being registered with the same independent sector practice or an NHS GP practice and therefore not visible.
- Parents or carers choosing not to share relevant information and no robust system to cross check with the more extensive NHS note keeping systems, such as hospital records or nursing and midwifery records that are often easily accessible within an NHS GP setting.
- Lack of robust standardised systems to ensure referral outcomes are communicated back to the referring independent GP from consultants and specialists.
- No robust system being in place for sharing information with their patient's usual NHS GP. This may be a problem if patients are seen when on holiday or out of their usual catchment area for other reasons.
- Potentially underused standardised pathways and protocols for safeguarding referrals in the independent setting compared to regularly used protocols and pathways in the NHS.
- Recognising abuse in affluent families can be difficult, for example child neglect can be much less visible. There can also be challenges working with parents from affluent and professional backgrounds.
- Independent clinics may only see adults and therefore children and any dependent adults may be less visible.
- Parents' perceptions that they are paying for a ring fenced specific medical service which does not invoke any safeguarding intervention by the independent GP.
- Potential differences in private patients' medical cultural background and their understanding of UK standards and the doctor's statutory duties under UK safeguarding regulations.
- Private patient expectations of 'control' over the private consultation and GP.
What can GPs working in the independent and online/digital sector do to ensure safeguarding is embedded into their practice?
Always consider safeguarding
- Always consider child and adult safeguarding in every interaction with a patient.
- Even if an
independent setting only has adult patients, practitioners in these
settings must always be mindful of children. The GMC in their
guidance Protecting children and young people: The responsibilities of all doctors, states:
“You must consider the safety and welfare of children and young people, whether or not you routinely see them as patients. When you care for an adult patient, that patient must be your first concern, but you must also consider whether your patient poses a risk to children or young people. You must be aware of the risk factors that have been linked to abuse and neglect and look out for signs that the child or young person may be at risk.” - Ensure knowledge and awareness of specific types of abuse where perpetrators may seek to use the independent health sector to obtain medical treatment for victims of abuse but evade wider multi-agency involvement. For example, modern slavery, trafficking, sexual and criminal exploitation, domestic abuse, ‘Honour-based’ abuse, Fabricated and Induced Illness.
- Be aware that some patients may seek to use independent healthcare to evade statutory services, especially when there are safeguarding concerns.
- Understand how abuse might present in affluent families.
- Understand, and be able to respond to, the challenges of safeguarding in affluent communities.
- Consider how safeguarding concerns will be further explored or followed up in a setting where patients pay for consultations. Where a cost may normally be attributed to patient contacts, this should never be a barrier for carrying out appropriate safeguarding activity. For example, in situations where you are ‘considering’ abuse or neglect as a possible cause for a patient’s presenting symptoms or situation, how will you explore and follow this up if the patient does not wish to pay for further consultations?
- Work closely with colleagues and discuss any safeguarding concerns early.
Safeguarding training
- Attend regular safeguarding training and ensure training is up to date and relevant to role – GPs and all general practice staff, regardless of whether they work in the NHS, independent or online sector, require the same level of safeguarding training as set out in the RCGP Safeguarding Standards. These standards include child and adult safeguarding equally and are applicable even if the independent GP service sees only adult patients.
- Consider how the organisation keeps itself up to date with safeguarding national guidance and case reviews.
Safeguarding policies and procedures
- Ensure safeguarding responsibilities and policies are clear and visible on the organisation’s website and available to staff in consulting rooms.
- Ensure there are policies in place regarding information sharing and that these are clear and visible on the organisation’s website.
- Ensure all staff members are aware of and have read the organisation’s safeguarding policies.
- Ensure local safeguarding referral processes and contact numbers are kept up to date and easily accessible to all staff members. In England, the NHS Safeguarding App (4) is a comprehensive resource and includes links to all safeguarding partnerships within England.
- Providers of online and remote GP services should be aware of the specific challenges this brings with regards to safeguarding such as providing care across a large geographical area including delivering care across national and international borders – providers should ensure they have processes in place to identify safeguarding concerns and respond appropriately.
- The following documents will be helpful for online providers to ensure
they are providing a safe service:
- CQC. The state of care in independent online primary health services. Findings from CQC’s programme of comprehensive inspections in England. Updated 2022.
- FSRH/BASHH. Standards for Online and Remote Providers of Sexual and Reproductive Health Services. 2019.
- If the organisation provides virtual consultations, be clear on how safeguarding concerns can be identified and followed up.
- If the organisation provides questionnaire-based interactions with clinicians, consider how safeguarding concerns can be identified and followed up.
- Encourage patients to also register with an NHS GP.
Verifying patient identity
-
Have clear policies in place regarding checking identities. This is of particular importance when there are prescription requests that could indicate a safeguarding concern such as for addictive drugs or for recurrent sexually transmitted infections.
Safe prescribing
- Have clear safe prescribing policies in place, especially regarding drugs with the potential for misuse as well as addiction.
- Have clear policies in place regarding checking identities, especially when there are prescription requests that could indicate a safeguarding concern such as for addictive drugs or for recurrent sexually transmitted infections.
Organisational safeguarding lead
- Have a organisational safeguarding lead.
- Ascertain who safeguarding advice can be sought from when needed and have this information easily accessible to all staff members. This includes seeking advice from within the organisation and from external safeguarding professionals.
- Ascertain whether the organisational safeguarding lead can be part of any local peer support networks such safeguarding lead forums.
Safeguarding documentation and information sharing
- Information sharing is fundamental to safeguarding children and adults. Those working in the independent sector should have an understanding of the multi-agency process of information sharing when there are safeguarding concerns and how they will ensure they are included in this process. For example, when there is a concern that a child or adult is being abused or neglected, multi-agency partners need all the relevant information from health services to be able to make safe and accurate decisions about that child or adult’s welfare. Local authorities will generally request relevant information from NHS health partners such as GPs, health visitors, midwives, mental health trusts and hospital trusts. Independent providers should consider how they can ensure that the information they hold can be part of the multi-agency safeguarding process and response.
- Ensure safeguarding concerns are documented clearly in the patient record including appropriate safeguarding coding and flags on records so that when there are safeguarding concerns, these are immediately identifiable to any clinician caring for the patient.
- Professionals and providers should seek consent to share information wherever appropriate to do so but also be aware of their responsibility to share information without consent when necessary to do so, particularly when there are safeguarding concerns.
- If a patient does not want to share information with their NHS GP or other healthcare providers, this should be fully explored to understand the reasons for this.
- Safeguarding relies on appropriate and effective communication between different healthcare providers. Providers should therefore ensure there is good communication and information sharing between independent GPs and other independent sector staff and between NHS sector staff including NHS GPs, hospital staff and social care. This is a professional responsibility and placing the onus on patients to do this is inappropriate.
Think family approach
- Make children visible and use a 'think family' approach in consultation. Have conversations with the parents that discuss their children at an early stage in the doctor patient relationship.
- Understand the constraints of seeing families and children with limited access to full information and think about asking for more contextual information if necessary to support your 'think family' approach.
Further resources
- CQC. GP mythbuster 25: Safeguarding adults at risk. Updated 2024.
- CQC. GP mythbuster 33: Safeguarding children. Updated 2024.
References
- GMC. Protecting children and young people: The responsibilities of all doctors.
- Kingston and Richmond Safeguarding Children Partnership. Safeguarding in Affluent Communities.
- Professor Claudia Bernard. Goldsmiths, University of London. An Exploration of How Social Workers Engage Neglectful Parents from Affluent Backgrounds in the Child Protection System.
- CQC. The state of care in independent online primary health services. Findings from CQC’s programme of comprehensive inspections in England.
- FSRH/BASHH. Standards for Online and Remote Providers of Sexual and Reproductive Health Services.2019.
- NHS England Safeguarding App. For practitioners in England, the NHS Safeguarding App is an easy way to find your local authority details. It can be accessed by visiting your device’s appropriate app store and searching for ‘NHS Safeguarding’.
Part 2A: Identification of abuse and neglect
This section covers the identification of abuse and neglect in children and adults. The information contained within this section is taken from a very wide range of sources, with the aim to bring together the key information practitioners need in general practice to be able to identify abuse and neglect.
Identifying child abuse and neglect:
- The rights of children.
- Adverse childhood experiences.
- Safeguarding young people aged 16 and 17 years old.
- Age of consent, Fraser Guidelines and Gillick competence.
- How does child abuse/neglect present in general practice?
- Obstacles to recognising and responding to child abuse and neglect.
- Where do children experience abuse and neglect?
- Contextual safeguarding.
- Children at greater risk of abuse and neglect.
- Children who may be invisible to services.
- Looked after children.
- Caring for refugee and asylum seeking children.
- Perinatal safeguarding.
- Unseen men.
- Disguised compliance.
- Types of child abuse and neglect:
- physical abuse
- bruising in non-mobile infants
- abusive head trauma and persistently crying babies
- perplexing presentations and fabricated or induced illness (FII)
- neglect
- Was not brought
- emotional abuse
- sexual abuse
- talking about child sexual abuse
- working with families affected by child sexual abuse
- online child sexual abuse and exploitation
- child sexual exploitation
- child criminal exploitation and gangs
- harmful sexual behaviour
- Independent Inquiry into Child Sexual Abuse (IICSA)
- child trafficking and modern slavery
- female genital mutilation (FGM)
- child abuse linked to faith or belief
- bullying and cyberbullying.
- physical abuse
Topics covering both child and adult issues:
- Radicalisation.
- Domestic abuse including ‘honour’ based abuse and forced marriage.
- Transitional safeguarding.
Identifying adult abuse and neglect:
- Types of adult abuse and neglect:
- physical abuse
- sexual abuse
- psychological or emotional abuse
- financial or material abuse
- modern slavery
- discriminatory abuse
- neglect and acts of omission
- self-neglect.
- Organisational abuse including safeguarding in care homes.
- Adults at greater risk of abuse and neglect.
- How adult abuse/neglect presents in general practice?
- Safeguarding those who are homeless.
- Was not brought.
The rights of children
The rights of children are enshrined in UK law. The UK ratified the UN Convention on the Rights of the Child (UNCRC) in 1992. The Convention has 54 articles that cover all aspects of a child’s life and set out the civil, political, economic, social and cultural rights that all children everywhere are entitled to. It also explains how adults and governments must work together to make sure all children can enjoy all their rights.
Every child has rights “without discrimination of any kind, irrespective of the child’s or his or her parent’s or legal guardian’s race, colour, sex, language, religion, political or other opinion, national, ethnic or social origin, property, disability, birth or other status.”
—Article 2, UNCRC
There are four articles in the Convention that are seen as special. These are known as the ‘General Principles’. They are:
There are also articles within the Convention’s 54 articles which are particularly relevant to safeguarding and child protection. For example:
- Article 19 (protection from violence, abuse and neglect). Governments must do all they can to ensure that children are protected from all forms of violence, abuse, neglect and bad treatment by their parents or anyone else who looks after them.
- Article 39 (recovery from trauma and reintegration). Children who have experienced neglect, abuse, exploitation, torture or who are victims of war must receive special support to help them recover their health, dignity, self-respect and social life.
A summary by UNICEF of the UN Convention on the Rights of the Child can be found here: UNCRC_summary-1_1.pdf.
This summary provides a powerful reminder of the rights of children which should be embedded into all that we do to protect children from abuse and neglect as well as supporting those who are victims and survivors.References
Adverse childhood experiences
Adverse childhood experiences (ACEs) are highly stressful and potentially traumatic events or situations that occur during childhood and/or adolescence. They can be single events, or prolonged threats to (and breaches of) the young person’s safety, security, trust or bodily integrity. These experiences directly affect the young person and their environment, and require significant social, emotional, neurobiological, psychological or behavioural adaption. In other words, ACEs can affect the way young people feel, behave and view the outside world. There are examples of ACEs below.
Experiencing trauma can result in a young person struggling with their mental health. A wide range of mental health conditions and symptoms can be linked to trauma, including, anxiety, depression, obsessive compulsive disorder (OCD), eating disorders and self-harming behaviours.
ACEs can have a significant negative impact on people’s lives. However, such experiences should not be seen as placing limits on someone’s aspirations and achievements. Individuals’ experience of and response to adversity and trauma depends on a range of factors, including the existence of supportive relationships, positive community experiences, access to financial resources and other forms of support. It’s therefore not possible to determine an individual’s longer-term outcomes (like their health or education) based on the number of ACEs they have experienced.
Scotland’s National Trauma Transformation Programme highlights that “adversity is not destiny”: many people may experience some form of traumatic event in their lives; the majority of people recover well, through supportive, positive relationships with family, friends, colleagues, people in their community, service professionals, and in some cases also receiving clinical psychological interventions or therapy.
Some examples of ACEs:
- Abuse or neglect.
- Violence and coercion, e.g. domestic abuse, gang membership, being a victim of crime.
- Adjustment, e.g. migration, asylum or ending relationships.
- Prejudice, e.g. anti-LGBTQIA+, sexism, racism or disablism.
- Household or family adversity, e.g. substance misuse, intergenerational trauma, destitution or deprivation.
- Inhumane treatment, e.g. torture, forced imprisonment or institutionalisation.
- Adult responsibilities, e.g. being a young carer or involvement in child labour.
- Bereavement and survivorship, e.g. traumatic deaths, surviving an illness or natural accident.
Impact of ACEs
Those who experience four or more ACEs are:
- Two times more likely to binge drink and have a poor diet.
- Three times more likely to be a current smoker.
- Four times more likely to have low levels of mental wellbeing and life satisfaction.
- Five times more likely to have had underage sex.
- Six times more likely to have an unplanned pregnancy.
- Seven times more likely to have been involved in violence.
- 11 times more likely to have used illicit drugs.
- 11 times more likely to have been incarcerated.
Protective factors against ACEs
There are some personal, structural and environmental factors which can protect children against adverse outcomes. Examples of these are:
- Positive and supportive family environments.
- Safe and mutual relationships with peers.
- Access to a wider supportive and understanding community.
- Ability to regulate emotions and manage emotional distress.
- Acquisition of practical problem-solving skills.
- Compassionate, attuned and supportive responses from professionals.
- Early intervention from support, therapeutic or safeguarding services.
- Trauma-informed policies & systems that address bullying, harassment or victimisation.
How can general practice support patients who have experienced adverse childhood experiences?
- Be aware of adverse childhood experiences, how common they are and how they relate to health and wellbeing.
- Be able to recognise the impact, short and long term, of adverse childhood experiences.
- Be trauma informed and embed trauma informed practice routinely into your organisation and professional role. (More information on trauma informed practice is in Section 3 of the toolkit.)
- Be able to respond compassionately and supportively to those who have experienced trauma.
- Be mindful that colleagues may also have experienced adverse childhood experiences.
- Take appropriate safeguarding action when needed.
References
- Young Minds. Understanding Trauma and adversity. 2024.
- Scottish Government. Factsheet:Psychological trauma and adversity including ACEs (adverse childhood experiences). 2024.
- National Trauma Transformation Programme. Home page of NTTP. Responding to Psychological Trauma in Scotland.
Safeguarding young people aged 16 and 17 years old
There are a number of issues to consider in this age group:
- Young people who are 16 and 17 years old have significant potential to fall through the gaps between child and adult services.
- They are still legally children and should be given the same protection and entitlements as any other child.
- The fact that a child has reached 16 years of age, is living independently or is in further education, is a member of the armed forces, is in hospital or in custody in the secure estate, does not change their status or entitlements to services or protection. In Scotland, the definition of a child varies in different legal contexts. Where a young person between the age of 16 and 18 requires support and protection, services will need to consider which legal framework best fits each persons’ needs and circumstances.
- Mental capacity legislation in all UK nations applies from 16 years old.
- Professionals have to balance the rights of young people with their duty to protect them from abuse and neglect.
- No child can ever consent to their own abuse.
- Consider transitional safeguarding.
- Actively prepare, plan and advocate for transition into adulthood including into adult services.
References
- NSPCC. Children and the law. 2024.
- HM Government. Working together to safeguard children. Updated 2024.
Age of consent
In each UK nation, the age at which people can legally consent to sexual activity (also known as the age of consent) is 16-years-old. This is the same regardless of the person's gender identity, sexual identity and whether the sexual activity is between people of the same or different gender.
Sexual activity involving a child under the age of 13 should always result in a child protection referral. This includes situations where both children engaged in sexual activity are under 13 years old and even if the child under 13 has agreed to sexual activity. Anyone under 13 lacks capacity to give valid consent to any sexual act.
The law is there to protect children from abuse or exploitation. It is not designed to unnecessarily criminalise children.
Although children over the age of 16 can legally consent to sexual activity, they may still be vulnerable to harm through an abusive sexual relationship. Practitioners should assess and address their safety and wellbeing in line with safeguarding procedures.
The law gives extra protection to all under 18 year olds, regardless of whether or not they are over the age of consent. It is illegal:
- to take, show or distribute indecent photographs of a child under the age of 18 (this includes images shared through sexting or sharing nudes)
- to sexually exploit a child under the age of 18
- for a person in a position of trust (for example teachers or care workers) to engage in sexual activity with anyone under the age of 18 who is in the care of their organisation.
Regarding sexual activity, the GMC highlights in their guidance: 0-18 years: guidance for all doctors, (paragraphs 57 – 62):
- “A confidential sexual health service is essential for the welfare of children and young people. Concern about confidentiality is the biggest deterrent to young people asking for sexual health advice. That in turn presents dangers to young people’s own health and to that of the community, particularly other young people.
- You can disclose relevant information when this is in the public interest. If a child or young person is involved in abusive or seriously harmful sexual activity, you must protect them by sharing relevant information with appropriate people or agencies, such as the police or social services, quickly and professionally.
- You should consider each case on its merits and take into account young people’s behaviour, living circumstances, maturity, serious learning disabilities, and any other factors that might make them particularly vulnerable.
- You should usually share information about sexual activity involving children under 13, who are considered in law to be unable to consent. You should discuss a decision not to disclose with a named or designated doctor for child protection and record your decision and the reasons for it.
- You should usually share information about abusive or seriously harmful sexual activity involving any child or young person, including that which involves:
- a young person too immature to understand or consent
- big differences in age, maturity or power between sexual partners
- a young person’s sexual partner having a position of trust
- force or the threat of force, emotional or psychological pressure, bribery or payment, either to engage in sexual activity or to keep it secret
- drugs or alcohol used to influence a young person to engage in sexual activity when they otherwise would not
- a person known to the police or child protection agencies as having had abusive relationships with children or young people.
- You may not be able to judge if a relationship is abusive without knowing the identity of a young person’s sexual partner, which the young person might not want to reveal. If you are concerned that a relationship is abusive, you should carefully balance the benefits of knowing a sexual partner’s identity against the potential loss of trust in asking for or sharing such information.”
Fraser guidelines and Gillick competence
These two terms are often used together but there are distinct differences between them.
The Fraser guidelines apply to advice and treatment relating to contraception and sexual health.
Gillick competency is often used in a wider context to help assess whether a child has the maturity to make their own decisions and to understand the implications of those decisions.
Fraser guidelines
Fraser guidelines are used specifically to decide if a child can consent to contraceptive or sexual health advice and treatment. They can also be applied to advice and treatment for sexually transmitted infections and the termination of pregnancy.
Practitioners using the Fraser guidelines to guide care should be satisfied of the following:
- the young person cannot be persuaded to inform their parents or carers that they are seeking this advice or treatment (or to allow the practitioner to inform their parents or carers)
- the young person understands the advice being given
- the young person's physical or mental health or both are likely to suffer unless they receive the advice or treatment
- it is in the young person's best interests to receive the advice, treatment or both without their parents' or carers' consent
- the young person is very likely to continue having sex with or without contraceptive treatment.
Health professionals should still encourage the young person to inform his or her parent(s)/carers or get permission to do so on their behalf, but if this permission is not given they can still give the child advice and treatment. If the conditions are not all met, however, or there is reason to believe that the child is under pressure to give consent or is being exploited, there would be grounds to break confidentiality which may include (depending on the situation) sharing necessary and proportionate information with parents and making a child safeguarding referral.
When using Fraser guidelines for issues relating to sexual health, you should always consider any previous concerns that may have been raised about or by the young person and any potential child protection concerns:
- Underage sexual activity is a possible indicator of child sexual exploitation and children who have been groomed may not realise they are being abused.
- Sexual activity with a child under 13 should always result in a child protection referral.
- If a young person presents repeatedly about sexually transmitted infections or the termination of pregnancy this may be an indicator of child sexual abuse or exploitation.
The GMC has further guidance on sexual activity of children and young people in their document: ‘0-18 years: guidance for all doctors’ as noted above.
Gillick competence
Gillick competence is the principle used to judge capacity in children to consent to medical treatment. The Gillick test determines that children under 16 can consent if they have sufficient understanding and intelligence to fully understand what is involved in a proposed treatment, including its:
- purpose,
- nature,
- likely effects and risks,
- chances of success and
- the availability of other options.
If a child passes the Gillick test, he or she is considered ‘Gillick competent’ to consent to that medical treatment or intervention. However, as with adults, this consent is only valid if given voluntarily and not under undue influence or pressure by anyone else. Additionally, a child may have the capacity to consent to some treatments but not others. The understanding required for different interventions will vary, and capacity can also fluctuate such as in certain mental health conditions. Therefore each individual decision requires assessment of Gillick competence.
If a child does not pass the Gillick test, then the consent of a person with parental responsibility (or sometimes the courts) is needed in order to proceed with treatment.
If a young person refuses treatment, particularly treatment that could save their life or prevent serious deterioration in their health, this presents a challenge that needs to be carefully considered. The GMC in their guidance 0 – 18 years (paragraphs 30 – 33), outline what you have to consider and what steps you should take in this scenario. These include weighing up the harms to the rights of children and young person against the benefits of treatment and including other professionals such as independent advocates, safeguarding professionals and taking legal advice.
References
- NSPCC. Children and the law. 2024.
- CQC. GP Mythbuster 8: Gillick competency and Fraser guidelines. Updated 2022.
- GMC. 0-18 years: guidance for all doctors. 2024.
- NSPCC. Gillick competency and Fraser guidelines. 2022.
How does child abuse/neglect present in general practice?
Presentations of child abuse and neglect in general practice are seldom clear-cut and well-defined, and different types of abuse can overlap in the same child. The context for concerns is often more important than the identification of an 'incident'. Child protection work has been likened to a patchwork or jigsaw puzzle. Often, it is only when individuals and agencies share information together that the picture is complete. This involves effective record keeping, information-sharing and communication, both internally and between agencies.
Professional curiosity is fundamental to how we work with children and their families. Professional curiosity is a practice mindset and communication skill that involves exploring and understanding what is happening by asking questions and maintaining an open mind. It is about understanding one’s own responsibility in managing risk and safety and knowing when to act, rather than making assumptions and taking things at face value.
Liaising with other universal health services providers (for example, midwives, health visitors and school nurses) is invaluable as they may be the first health professionals to recognise when a child, young person or family member is in difficulty and can help to build a more complete picture. The value of universal service provision is that GPs and their staff see a multitude of presentations and behaviours in children and young people, the majority of whom will not require action to be taken to ensure their welfare. Thus, when there is a situation that 'does not feel quite right' practitioners' intuition and clinical acumen are, in our experience, usually well-founded.
Below are some examples of how child abuse and neglect may present in general practice. This list is not exhaustive. Children and young people may disclose abuse and neglect, although disclosure to professionals is rarely a sudden or one-off event. They may tell a relative or friend and then be brought to a GP to explore next steps.
- The child gives signs or indicators (verbal or non-verbal) that raises suspicion of abuse.
- The child shares what is happening to them.
- Physical signs, e.g. bruises, injuries.
- Behaviour changes, e.g. more withdrawn, more angry, challenging behaviour, missing school, running away from home.
- Mental health concerns, e.g. anxiety, depression, self-harm, suicidal thoughts/attempts.
- Parents/carers/family members sharing concerns.
- Child displays harmful behaviour towards others, e.g. harmful sexual behaviour.
- Parent/child interactions that give rise to concerns.
- Parental mental health/substance misuse.
- Behaviour of an adult that raises concerns about the safety of children in their care.
- Disclosures from a parent/carer about abuse in their own life, e.g. domestic abuse, that also indicates abuse to children.
- Information shared from other health colleagues or other agencies/professionals.
- ‘Was not brought’ – repeated patterns of children not being brought to health appointments.
- Behaviour of a colleague or a Person in Position of Trust that gives concerns they may be a risk to children.
- Proactive questioning, for example, assessing for risk of child sexual exploitation in a contraception review.
It is worth noting that the signs of lots of different types of abuse can be similar. For example, a child who is more withdrawn could be experiencing any type of abuse. It is therefore important for practitioners to be able to recognise signs of trauma to be able to safeguard and protect children. If practitioners are concerned about abuse and neglect, they should provide children with opportunities for disclosure (if possible dependent on age, communication needs, situation) but should not rely on disclosure before taking action to protect children from harm.
Children and young people can find it difficult to tell someone or even understand that they are being abused or neglected. However, they may communicate an emotional reaction to their experiences indirectly through their behaviour. Marked changes to a child’s behaviour, emotional state or attitude should prompt practitioners to explore concerns through a sensitive enquiry about their wellbeing, giving them space and opportunity to talk.
Marked changes in behaviour or emotional state
A change in a child's behaviour or emotional state which is not fully explained by a stressful situation that is not part of child abuse and neglect such as bereavement, parental separation or a medical cause. Examples of marked changes may include:
- recurrent nightmares containing similar themes
- extreme distress
- markedly oppositional behaviour
- withdrawal of communication
- becoming withdrawn.
Practitioners should continue to consider the possibility of child abuse or neglect as a cause for behavioural and emotional changes, even if they are seemingly explained by another cause.
Children may not tell anyone about the abuse and neglect they are experiencing for numerous reasons, including:
- they are not aware they are being abused or neglected
- they are too scared to say anything for fear of reprisals or adverse repercussions to them or their family
- they told someone before and nothing happened or the abuse got worse
- they have specific communication needs.
Creating a supportive environment for the conversation, being sensitive and asking open questions may encourage children and young people to disclose abuse or neglect when they feel ready. If practitioners are concerned about abuse and neglect, whilst providing children with opportunities for disclosure (if possible dependent on age, communication needs, situation) they should also not rely on disclosure before taking action to protect children from harm.
References
- NICE Quality standard. QS179. Child abuse and neglect. 2019.
- North Yorkshire Safeguarding Children Partnership. Professional curiosity – Practice Guidance. 2024.
Obstacles to recognising and responding to child abuse and neglect
Healthcare professionals may come across many different obstacles in the process of identifying abuse and neglect, but these should not prevent them from following the appropriate course of action to prevent further harm to the child or young person. Examples of potential obstacles include the following:
- Concern about missing a treatable disorder.
- Healthcare professionals are used to working with parents and carers in the care of children and fear losing a positive relationship with a family already under their care.
- Discomfort of disbelieving, thinking ill of, suspecting or wrongly blaming a parent or carer.
- Divided duties to adult and child patients and breaching confidentiality.
- An understanding of the reasons why the abuse and neglect might have occurred, and that there was no intention to harm the child.
- Losing control over the child protection process and doubts about its benefits.
- Stress.
- Personal safety.
- Fear of complaints.
It is important that we recognise our own personal obstacles, as well as organisational and system obstacles, to recognising and responding to child abuse and neglect so that we can overcome these and keep children at the centre of all we do.
References
- NICE guideline. CG89. Child maltreatment: when to suspect maltreatment in under 18s. Updated 2017.
Where do children experience abuse and neglect?
It can be useful to think about the different spheres of a child’s world as abuse can happen anywhere and by anyone:
Children of different ages will be impacted differently by different spheres. For example, the risk to newborn babies may come mostly from within their own home. For teenagers, risk may come much more from online or community settings.
Contextual safeguarding
Contextual safeguarding recognises that as young people grow and develop they are influenced by a whole range of environments and people outside of their family. For example in school or college, in the local community, in their peer groups or online. Children and young people may encounter risk in any of these environments. The different relationships that young people form in their neighbourhoods, schools and online can feature violence and abuse. Sometimes the different contexts are inter-related and can mean that children and young people may encounter multiple risks.
Contextual safeguarding looks at how we can best understand these risks, engage with children and young people and help to keep them safe. It is an approach to understanding, and responding to, young people’s experiences of significant harm beyond their families.
It's an approach that's often been used to apply to adolescents, though the lessons can equally be applied to younger children, especially in today's changing world.
Parents and carers have little influence over these contexts, and young people’s experiences of extra-familial abuse can undermine parent-child relationships.
References
- NSPCC. Contextual safeguarding: what is it and why does it matter? 2019.
- Durham University. Contextual safeguarding. 2024.
Children at greater risk of abuse and neglect
Any child can be at risk of abuse, however there are a number of factors that can increase a child’s vulnerability to abuse and neglect. NICE identifies these as:
Child factors:
- Age under four years old, or adolescence.
- Physical and/or mental impairment — may be due to factors such as impaired capacity to resist or avoid maltreatment, lack of effective communication, inability to understand what is happening or to seek help, and dependency on carers for personal assistance.
- Living in the care system.
- Being a twin or multiple.
- Being unwanted or failing to fulfil the expectations of parents/carers.
- Identifying as (or being identified as) lesbian, gay, bisexual, or transgender.
Parental/carer factors (which may be compounded by lack of support from family or friends):
- Substance misuse.
- A history of domestic abuse, including sexual violence or exploitation, and/or maltreatment as a child.
- Emotional volatility or having problems managing anger.
- A history of violent offending or other criminal activity.
- Mental or neurological disorders.
- Known maltreatment of animals.
- Poor education.
- Lack of parenting knowledge.
- Learning difficulties — child maltreatment may occur due to a lack of understanding of parental responsibilities and limited support.
- Low self-esteem.
Family and environmental factors:
- Poverty and financial pressures, poor housing — may be associated with a higher level of parental stress and an increased risk of child maltreatment.
- Maltreatment of other children within the family, or violence between family members.
- Family/relationship breakdown.
Community and societal factors:
- Gender and social inequality.
- Lack of adequate housing or services to support families.
- High levels of unemployment or poverty.
- Inadequate policies and programmes to prevent child maltreatment.
- Social and cultural norms that promote or glorify violence towards others or diminish the status of the child in parent/carer–child relationships.
- Social, economic, health, and education policies that lead to poor living standards or socioeconomic inequality or instability.
Risk factors for recurring or persistent child abuse and neglect include:
- refusal by the parent or carer to engage with services
- the parent or carer experiencing a mental health or substance misuse problem which has a significant impact on the tasks of parenting
- chronic parental stress
- the parent or carer experienced abuse or neglect as a child
- the child communicates in a different way – they may not know how to communicate that they are being abused
- may have never been given the words/tools to use to tell someone
- professionals/family/carers misunderstanding behaviour which may indicate abuse
- never been asked
- they are ignored
- they have multiple needs and need more care – more opportunities for abuse
- can be targeted for abuse as less likely to be able to tell
- may be unable to protect themselves due to their disabilities.
Children who may be invisible to services
Practitioners should be aware that there are children who are invisible to many services but who may present to general practice for healthcare needs. These can include:
- children who are home-schooled
- 16 and 17 year old young people not in education, training or employment
- unaccompanied asylum seeking children
- children in secure hospitals, prisons or children’s homes.
If a practitioner becomes aware that a child is not in school, training or employment, this should be noted clearly on their record.
References
- Children’s Commissioner for England report 2020. Hundreds of vulnerable ‘invisible children’ in England are being locked away without any legal protection. 2020.
Looked-after children
A child who has been in the care of their local authority for more than 24 hours is known as a looked-after child. ‘Looked-after children’ is an official government term and is widely used among professionals along with the acronym ‘LAC’. However, children report that words like ‘unit’, ‘placement’, ‘contact’, ‘respite’ and the acronym ‘LAC’ (for looked-after children) created a sense of being different, exacerbated low self-esteem and made them feel stigmatised. Children and young people often prefer the term ‘children in care’.
Every UK nation has a slightly different definition of a looked-after child and its own legislation, policy and guidance.
In general, looked-after children are:
- living with foster parents/carers
- living with prospective adoptive parents (these children remain looked-after children until the adoption order is granted)
- living with friends or relatives, through kinship foster care
- living in a residential children's home
- living in residential settings like schools, secure units or semi-independent living accommodation.
A child stops being 'looked-after' when they are adopted, return home or turn 18. However local authorities in all the nations of the UK are required to support children leaving care at 18 until they are at least 21. This may involve them continuing to live with their foster family.
Not all children in the care of someone other than their parents have ‘looked-after’ status. For example, they may be in private foster care or cared for under a special guardianship order.
Private fostering is an arrangement that is made privately (without the involvement of the local authority) for the care of a child under the age of 16 (under 18, if disabled) by someone other than a parent or close relative with the intention that it should last for 28 days or more. Private foster carers may be from the extended family such as a cousin or great aunt. However, a person who is a relative under the Children Act 1989 i.e. a grandparent, brother, sister, uncle or aunt (whether of full blood or half blood or by marriage) or stepparent will not be a private foster carer. A private foster carer may be a friend of the family, the parent of a friend of the child, or someone previously unknown to the child’s family who is willing to privately foster a child.
Privately fostered children are not looked-after children. The local authority should be notified if a professional becomes aware of a private fostering arrangement where they are not satisfied that the local authority have been, or will be, notified of the arrangement. The local authority have a duty to ensure that the welfare of the privately fostered child is satisfactorily safeguarding and promoted.
Anyone proposing to privately foster a child must notify the appropriate local authority of the proposal at least six weeks before the date on which the private fostering arrangement is to begin or immediately where the arrangement is to begin within six weeks.
Special guardianship is when a local authority places a child or young person to live with someone other than their parent(s) on a long-term basis. It aims to provide more security than long-term fostering for children where adoption is not the best option. Special guardianship orders are not available in Scotland.
Each child will have their own unique journey into care but the most common reason for becoming looked-after is abuse or neglect. Unaccompanied asylum-seeking children are also children in care. All children in care will have experienced trauma in some way.
Every child in care is a unique child with individual strengths and needs. However, the physical, emotional, and mental health of some looked-after children will have been compromised by neglect or abuse. Children in care:
- have higher rates of mental health disorders
- can experience frequent placement moves which can disrupt the support they receive, treatment plans and access to services
- are at a greater risk of poor educational outcomes
- have a higher prevalence of special educational needs
- have a higher prevalence of speech, language and communication needs
- are significantly over-represented in the criminal justice system.
Health assessments for looked-after children
When a child becomes a looked-after child, they undergo an initial health assessment (IHA). The IHA is a holistic assessment of physical and mental health needs, analysing and assessing past medical health, missed health problems and missed screening opportunities.
Children in care also subsequently have a review health assessment whilst they remain in care. These are every six months for children under five years old and annually for those over five and up to 18 years.
These assessments are completed by clinicians, such as paediatricians or nurses in Looked-After Children teams, with specialist training and are not done in general practice. However, general practice plays a vital role in sharing relevant information to the health professional undertaking the assessment and contributing to any actions required in general practice.
How can general practice support looked-after children?
General practice teams have a vital role in identifying the individual healthcare needs of children in care. GP practices should:
- ensure timely access to a GP or other appropriate health professional when a child in care requires a consultation
- provide summaries of the health history of a child who is in care, including information on immunisations and covering their family history where relevant and appropriate, and ensure that this information is passed promptly to health professionals undertaking health assessments
- maintain a record of the health assessment and contribute to any necessary action within the health plan
- make sure the GP-held clinical record for a child in care is maintained and updated and that health records are transferred quickly if the child registers with a new GP practice, such as when he or she moves into another area, leaves care or is adopted
- avoid registering a child in care as a temporary resident as the medical record is not available to the treating clinician
- be mindful of the particular challenges of parental proxy access to children’s online medical record when the child is in care and whether this should be revoked to ensure confidentiality of the placement and security of the child. (See the RCGP GP online services toolkit for more information.)
In addition, all practitioners working with children in care should be aware of the impact of trauma (including developmental trauma) and attachment difficulties and appropriate responses to these, to help them build positive relationships and communicate well.
Health assessments for prospective foster carers and adopters
This is another important area in which general practice plays a vital role. Fostering and adoption panels assess applications and make decisions on whether adults are suitable to be foster carers, kinship carers or adopters. Many children who are in the care system have a history of neglect and/or physical, sexual or emotional abuse and other adverse experiences. They are therefore likely to have a range of significant individual needs. Prospective adopters and carers must have robust physical and mental health to be able to parent these vulnerable children.
The panel make their assessments based on a wide range of information from different sources including a medical report from the prospective foster carer/adopter’s GP. Health information about prospective adopters or foster carers and its interpretation form only one part of the application and supervision process and will be set alongside other information obtained by the agency in considering the suitability of applicants. It is unusual for health issues to prevent approval as carers/parents. The information provided is also used to assist appropriate matching of carers and children. It is important that agencies satisfy themselves that applicants are able to meet the demands of parenting on a daily basis, and in the case of adoption and long-term placements, have a reasonable expectation of retaining good health to support children to adulthood.
Medical assessments are an important safeguard for both the adults and the children, and they are a statutory requirement in all four UK nations. Adults wishing to become foster carers or adopters are required by regulations to obtain a medical report during their applications process, and for foster carers at intervals during their fostering career their information needs to be updated. To ensure consistency of quality of information obtained across the UK, most adoption and fostering agencies use template documents that are produced by a professional membership organisation ‘CoramBAAF’ and this includes a standard report format to collate medical information including clinical assessment. A final decision cannot be made by the panel without a medical report being obtained and considered as part of the suitability assessment.
Care leavers
There are different definitions of a care leaver. Many young people prefer the term ‘care-experienced person’. The Care Leavers Association’s simple definition is: “any adult who has spent time in care”. The legal definition comes from the Children (Leaving Care) Act 2000 which is that the young person must have been in care for at least 13 weeks (or periods of time that add up to 13 weeks) since they reached 14, including sometime after their 16th birthday. There are specific services and support available from the local authority for those who qualify as a care leaver.
In all UK nations, children leaving care at 18 are entitled to support from their local authority until they are at least 21. Local authorities across the UK have a duty to assess and meet care leavers’ individual needs and to develop a pathway plan, setting out the support that will be provided to the care leaver once they have left care. This should include making sure the care leaver has somewhere suitable to live. In England, Wales and Northern Ireland, care leavers are also legally entitled to a personal adviser to help with the transition.
Outcomes for care leavers remain much worse than for their counterparts in the general population. There are five key issues that impact care leavers as set out in HM Government’s document: Keep on Caring. Supporting Young People from Care to Independence:
- Not being adequately prepared or supported to deal with the challenges of living independently.
- Barriers accessing education, employment and training.
- Lack of stability, safety and security.
- Difficulties in accessing the health support they need, in particular help to maintain their emotional health and well-being.
- Problems achieving financial stability.
Many of these issues are inter-related. Problems with money are often exacerbated by the fact that many care leavers are not in education, employment, or training (NEET). And the lack of a stable, safe place to live can impact negatively on a young person’s emotional health and put them at greater danger of a number of safeguarding risks, such as sexual exploitation or involvement with gangs. Care leavers also face the added challenge of having to cope with the demands of living on their own at a young age: having to manage finances, maintain a home and manage their lives independently, often without the support from families that most of us take for granted.
are leavers report particular challenges accessing adult services, especially adult mental health services. A third of young people leaving care report problems with drugs or alcohol a year later. A quarter of young women leaving care are pregnant, and nearly half become pregnant within 18 to 24 months.
How can general practice support care leavers?
Please read The Care Leavers’ Association booklet: 45 Care Leaver Friendly Ways.
This is a short guide on how to work with adolescent looked-after children and care leavers. This booklet has been created by care leavers who were involved in the Care Leavers’ Association health project. It is in their own words wherever possible. They share what would have made a difference to them now and when they were in care as a child. It is also punctuated by statistics on outcomes for care leavers so that professionals can understand how growing up in care can affect an individual for their entire life.
References
- NSPCC Learning. Why language matters: why you should avoid the acronym 'LAC' when talking about children in care. 2023.
- NSPCC. Children in care. 2024.
- Department for Education and Skills. Replacement Children Act 1989 Guidance on Private Fostering. 2005.
- NICE Guideline. NG205. Looked-after children and young people. 2021.
- Department for Education & Department of Health. Promoting the health and well-being of looked-after children: Statutory guidance for local authorities, clinical commissioning groups and NHS England. Updated 2022.
- RCPCH. Looked-After Children (LAC) resources and guidance.
- RCGP. Medical assessments for prospective foster carer and adopters in Wales statement. 2021.
- CoarmBAAF. Completion of medication reports for adoption and fostering applicants: Information for GPs. 2024.
- The Care Leavers’ Association. The Care Leavers’ Association home page.
- HM Government. UK Public General Acts. Children (Leaving Care) Act 2000.
- Nottinghamshire County Council. Local Offer for Care Leavers. 2024.
- Barnardos. Young people leaving care. 2024.
- NSPCC. Children in care. 2024.
- HM Government. Keep on caring: supporting young people from care to independence. 2016.
- The Care Leavers’ Association. 45 Care Leaver Friendly Ways. 2019.
Caring for refugee and unaccompanied asylum seeking children (UASC)
Unaccompanied asylum seeking children are young people who have journeyed to the UK accompanied by a parent or legal guardian. They are automatically a looked-after child under the care of the local authority. They have full entitlement to free NHS care and other public services. Everyone is eligible to register with a GP practice.
The Refugee Council has a glossary of terminology relating to asylum seekers and refugees in the UK.
In the year ending September 2022, the UK received 5152 applications for asylum from unaccompanied children. Many come from Sudan but also from countries such as Iran, Eritrea, Afghanistan, Vietnam, Iraq, Albania, Ethiopia and Syria. The majority are aged between 14 and 17 years but some are younger. Children are also regularly trafficked into the UK to be forced into domestic servitude, sexual exploitation and other forms of forced labour including cannabis cultivation.
This cohort of children may be particularly vulnerable and are likely to have complex physical and mental health needs as well as social needs. Formal interpreters should be used when needed. Some of the areas of health needs are listed here:
- Physical health:
- Malnutrition, including stunted growth, obesity and micronutrient deficiencies.
- Oral health.
- Unrecognised or unmanaged chronic health conditions.
- Low vaccine uptake.
- Trauma and injury, which includes FGM (female genital mutilation).
- Infections, e.g. tuberculosis, hepatitis B and C, HIV, malaria, leishmaniasis, filariasis, intestinal parasitosis, helminth infection, schistosomiasis, and sexually transmitted infections.
- Health issues related to sexual trauma/exploitation, such as pregnancy and sexually transmitted infections.
- Development.
- Lack of health screening and health promotion (e.g. newborn screening, thyroid function, hearing and vision screening, dental care).
- Mental health: there may be reactive, underlying and undiagnosed mental health needs. Below are some important issues to consider:
- Traumatic experiences can include exposure to war and conflict, torture, physical and sexual abuse, detention in the UK or in transit. This may eventually be diagnosed as PTSD (post-traumatic stress disorder), but for some children the trauma is ongoing, with concern about family and managing the immigration system. The journey to the UK is often complex and long and children can accumulate trauma along this journey.
- Exaggerated responses to normal emotional triggers may be a response to trauma and toxic stress. This needs to be taken into account when considering other conditions e.g. neurodevelopmental or trying to explain and support challenging behaviour.
- Disruption of important routines e.g. activities of family life, play, education. This can have profound impacts on children particularly at vulnerable life phases e.g. attachment in infancy, independence during puberty.
- Disruption to sleep, related to journeys and need to travel at night, fears for safety at night, flashbacks, lack of safe place, comfort toys/environment. This can have a negative impact on physical and emotional health, behaviour, and learning/development.
- Poor mental health of parents or siblings impacting on children.
UASC health has a comprehensive guide for primary care and GPs on the health needs of UASC (see references).
References
- Refugee Council. Refugee Council homepage. 2024.
- RCPCH. Refugee and asylum seeking children and young people – guidance for paediatricians. Updated 2023.
- RCGP. Asylum seekers and vulnerable migrants.
- UASC Health. Health resources and guidance.
- UASC Health. Tailored information for primary care staff.
Perinatal safeguarding
Becoming pregnant and having a baby can be an exciting time for parents and their wider families. However, this time can also be fraught with difficulties and challenges, particularly for parents with complex factors such as:
- parents who misuse substances (alcohol and/or drugs)
- parents/families who are recent migrants, asylum seekers or refugees, or who have difficulty reading or speaking English
- young parents including those in care or care leavers
- pregnant women who are experiencing any form of abuse including domestic abuse
- parents/families who are homeless or vulnerably housed
- parents who have had previous children removed from their care
- parents with pre-existing mental health issues
- parents who have experienced abuse and neglect as a child themselves
- parents who are socially isolated with little support.
Risks in this period can include:
- direct harm to the baby (before and after birth) due to alcohol/drugs or abuse
- direct harm to the mother due to alcohol/drugs or abuse
- worsening of pre-existing mental health illness which can impact the health and wellbeing of both baby and parents: this can impact the bond between parents and their baby as well as other children as well as impact the ability to care for the baby
- parents who have experienced abuse and neglect as a child themselves may feel ill-equipped to deal with parenthood and may not know what safe parenting looks like
- parents who have had previous children removed from their care may feel reluctant to engage with all services, including health, due to fears of having this baby removed as well. This can mean they don’t have the help and support they need as well as the risk of unidentified health problems during the pregnancy
- high levels of stress
- a baby that cries a lot can lead to exhaustion which can lead to anger and frustration which can then lead to a baby being shaken which can have catastrophic consequences
- a child with complex medical conditions and/or disabilities can result in difficulty bonding with the child and impact on the ability to care for the child
- pregnancy is a particularly high-risk time for domestic abuse. 30% of domestic abuse begins during pregnancy. 40 – 60% of women experiencing domestic abuse are abused during pregnancy.
There are also a number of communication and structural challenges in this area that complicate responsiveness, such as a lack of routine information sharing between GPs, midwives, and health visitors – there are many causes for this and there are different mechanisms in different areas to try and overcome this. Holistic care for these parents and families is vital, not just to identify risk and vulnerability, but to identify strengths and support available.
References
- NICE. Clinical Guideline. CG110. Pregnancy and complex social factors: a model for service provision for pregnant women with complex social factors. 2010.
- For Baby’s Sake. Domestic abuse and baby’s first 1001 days.
Unseen men
Men play a vital role in their children’s development and wellbeing and have a major influence on the children they care for. However, male caregivers and male partners sometimes go ‘unseen’ by services involved with children. Two types of unseen men have been identified in case reviews:
- Men who posed a risk to a child, which resulted in the child suffering serious harm or death.
- Men who could have protected and nurtured the child in their life but were overlooked by professionals.
Reasons for this oversight of unseen men include:
- a lack of professional engagement and curiosity
- an overly narrow focus on the quality of the care children receive from their mothers
- inadequate information sharing between services.
A report from The Child Safeguarding Practice Review Panel in 2021 entitled: ‘“The Myth of Invisible Men”. Safeguarding children under 1 from non-accidental injury caused by male carers’, found that there is an urgent need to improve how the system seems, responds to and intervenes with men who may represent a risk to the babies they are caring for. For this group of men, the role that they play in a child’s life, their history of parenting and their own experiences as children and how this affects them as adults, are too frequently overlooked by the services with responsibilities for safeguarding children and for supporting parents.
The review concluded that there are a number of contextual factors linked to non-accidental injury to infants and that their interaction heightens the risk of abuse. It identified the significance of men who have had a background of abusive, neglectful, or inconsistent parenting themselves, which can lead to poor mental health, often exacerbated by:
- substance abuse, especially use of drugs, which can encourage increased levels of stress and anxiety, sleeplessness, lowered levels of frustration tolerance, heightened impulsivity, poor emotional and behavioural regulation and poor decision making
- the co-existence of domestic abuse and the fact that some men mitigate their difficulties with others through a rapid default to violence and controlling behaviour
- living with the pressures of poverty, mounting debts, deprivation, worklessness, racism and very problematic relationships with the mothers of their children.
The NSPCC briefing: ‘Unseen men: learning from case reviews. Summary of risk factors for improved practice around ‘unseen’ men. 2022.’, highlights the key issues for learning from a sample of case reviews published since 2020 that highlight the issue of professionals not identifying or assessing key men involved in the care of children who died or suffered harm. These are:
- insufficient information sharing and record keeping
- lack of professional curiosity and engagement
- over-focus and reliance on mothers
- overlooking the ability of male carers to provide safe care.
Good practice points
- Identify men’s roles in a child’s life. See the ‘adult behind the child’.
- Seek out the child’s perspective on the men in their lives especially when there is a change in the child’s behaviour.
- Involve male caregivers – be aware that they may need education and support to help them in this role.
- When men attend with mental health or substance misuse problems, ask if they have any caring roles for children (including unborn children) and consider the impact these problems may have on their ability to parent safely.
References
- The Child Safeguarding Practice Review Panel. “The Myth of Invisible Men”. Safeguarding children under 1 from non-accidental injury caused by male carers. 2021.
- NSPCC. Unseen men: learning from case reviews. Summary of risk factors for improved practice around ‘unseen’ men. 2022.
- NSPCC. Why language matters: ‘hidden’ in plain sight. 2022.
Disguised compliance
Disguised compliance involves parents and carers appearing to co-operate with professionals in order to allay concerns and stop professional engagement. Disguised compliance, resistance and denial are common features of families with early help needs. Apparent resistance may be the result of fear, stigma, shame, denial, ambivalence, or the parent’s lack of confidence in their ability to change or lack of insight into their parenting capability and the impact on their children.
Indicators of disguised compliance can include:
- a lack of measurable progress at reviews, despite apparent effort and cooperation from parents
- parental agreement to change but not completing agreed actions to achieve it
- change occurring due to the efforts of other agencies rather than the parents
- inconsistency in the areas where change is achieved with parents opting to work with some professionals and not others or on some actions and not others; children’s views differing significantly from that of the parents
- frequent missed appointments
- exaggerated co-operation and compliance
- attempts to minimise professionals’ concerns or denial of the impact of the lived experience of the child
- aggressive or threatening behaviour when challenged
- unjustified claims of progress being made, or actions carried out, and a refusal to discuss key issues whilst focussing on others that have less or no impact for the child.
Professionals should:
- Consider the professional relationship with parents and ensure parents feel respected and avoid judgmental language or assertions about their behaviours or motivation.
- Be aware that disguised compliance could be occurring.
- Be alert to the risk of collusion with parents. Where parents appear co-operative, remain open to hearing the voice of the child throughout the process and always measure parents’ assertions there has been progress against the child’s lived experience. See and speak to the child regularly.
- Display professional curiosity when working with families and not accept information from parents and carers at face value without investigating further.
- Maintain respectful uncertainty.
- Establish the facts and gather evidence about what is actually happening or has been achieved.
- Focus on the child’s lived experience rather than the parents’ and carers’ actions.
- Share information with other professionals regularly and check on their view of progress made to challenge your assumptions.
References
- North Wales Safeguarding Board. Practice Guide. Working with people displaying disguised compliance. 2020.
- NSPCC. Disguised Compliance. 2019.
Types of child abuse and neglect
Statutory guidance across the four countries of the UK describes four main categories of abuse, and these definitions will normally be reflected in local organisations’ policies and procedures. The four main categories are: physical abuse, emotional abuse, sexual abuse and neglect.
There are a number of different types of child abuse which sit under the umbrella of the four main categories above. There can be significant overlap and children may experience more than one type of abuse at any one time. The different types include:
- physical abuse
- neglect
- emotional abuse
- sexual abuse
- child sexual exploitation
- harmful sexual behaviour
- domestic abuse
- bullying and cyberbullying
- online abuse
- child trafficking
- female genital mutilation (FGM)
- criminal exploitation and gangs
- grooming
- fabricated or induced illness
- radicalisation
- child abuse linked to faith or belief.
References
- HM Government. Working Together to Safeguard Children 2023. 2023.
- NSPCC. Types of abuse. 2024.
Physical abuse
Physical abuse is when someone hurts or harms a child or young person on purpose. It includes:
- hitting with hands or objects
- slapping and punching
- kicking
- shaking
- throwing
- poisoning
- burning and scalding
- biting and scratching
- breaking bones
- drowning.
It's important to remember that physical abuse is any way of intentionally causing physical harm to a child or young person. It also includes making up the symptoms of an illness or causing a child to become unwell.
Bruising
There are a number of possible clinical findings suggestive of abuse. These including bruising in pre-mobile children, bruises that are seen away from bony prominences and bruises that carry the imprint of an implement used or a ligature. Bruising is the most common injury in children who have been abused. It is also a common injury in non-abused children. However, the exception to this is pre-mobile infants in whom accidental bruising is rare (0-1.3%).
References
- Child Safeguarding Practice Review Panel. Bruising in non-mobile infants panel briefing paper. 2022.
Smacking
Smacking is now illegal in Wales and Scotland.
Wales – All physical punishment of children is illegal in Wales, including by parents, carers and anyone acting in loco parentis in any setting in Wales. In March 2022, the law changed to remove the use of the defence of ‘reasonable punishment’.
Scotland – All forms of physical punishment of children are against the law in Scotland. In November 2020, the law changed to remove the use of the defence of ‘reasonable chastisement’.
The RCPCH published a policy report in April 2024 calling for the same legal changes in England and Northern Ireland: Equal protection from assault in England and Northern Ireland.
References
- Wales Safeguarding Procedures. Safeguarding children in relation to the Children (Abolition of Defence of Reasonable Punishment) (Wales) Act 2020. Updated 2022.
- Mygov.scot. Smacking and children. 2020.
- RCPCH. Policy Report. Equal Protection from assault in England and Northern Ireland: The health, education and legal case for legislative change to remove the “reasonable punishment” defence and to prohibit all physical punishment of children. 2024.
Injuries to non-independently mobile children *
(*The term ’non-independently mobile children’ includes not only babies, but older children with physical disabilities who are not independently mobile.)
The likelihood of children sustaining accidental injuries increases with increasing mobility. However, Serious Case Reviews (SCR) have identified that professionals sometimes fail to recognise the highly predictive value, for child abuse, of the presence of injuries to non-independently mobile children.
Infants under 12 months are at increased risk of non-accidental injury (NAI). When examining a child who is non-independently mobile, it is important to remember 'those who can't cruise rarely bruise'. A small apparently insignificant bruise in a baby might be a marker for a serious life-threatening injury. Children under 12 months are consistently over-represented in Serious Case Reviews (SCR), almost exclusively because of severe injury or death as a result of physical abuse. This short video developed by Nottinghamshire Safeguarding Children Partnership is a useful resource.
Bruising is the most common presentation in children who have been physically abused although other injuries can include burns, fractures or unexplained bleeding.
Any injury to a child who is not independently mobile should be treated with concern. Physical abuse must be considered.
When faced with an injury or potential injury in a non-independently mobile child, practitioners should:
- Seek an explanation from the parent or carer.
- Consider if the injury is feasible given the child's age and developmental stage (bearing in mind that developmental age is not always related to chronological age).
- Consider if there has been a delay in presentation.
- Consider whether there are any other safeguarding concerns regarding the child's presentation, for example, indicators of neglect.
- Consider adult behaviours which may affect the safety of their child such as domestic abuse, mental health issues, learning disability or substance misuse.
- Consider if there is any information available regarding the child or family history which would raise concerns, for example, children subject to previous child protection plans.
- Seek further information about who is in the child's life, for example, new partner of the parent or the hidden male.
- Children should, where possible, be asked to contribute to the history taking and have an opportunity to be seen alone during a consultation if age-appropriate. Young or pre-verbal children presenting with physical indicators of harm should be fully examined.
It is important to note that even in the absence of other known safeguarding concerns such as those listed above, an injury to a non-independently mobile child must still be taken seriously – this may be the first indication that a child is suffering abuse or neglect.
Each area may have different local multi-agency safeguarding protocols regarding bruising in non-mobile babies and children. It is important that each practitioner is aware of their local pathways.
For more information on bruising and patterns of bruising in child abuse, please visit the Forensic Medicine for Medical Students website.
References
- NSPCC. Physical abuse. 2024.
- RCPCFH. Child Protection Evidence. Systematic review on Bruising. 2020.
Abusive head trauma and persistently crying babies
Abusive head trauma, previously known as Shaken Baby Syndrome, is a devastating form of abuse which can result in catastrophic injuries and death. It affects 1 in 4000 – 5000 infants every year. Males represent 70% of perpetrators. Fathers and male surrogates are nearly five times as likely as mothers to shake an infant.
Stress is an especially prominent factor in violence towards children. Stressors include background or environmental factors such as noisy environments and in particular, uncontrollable noise. A crying baby can be described as uncontrollable and its effects on parents and caregivers can be very powerful. A baby’s excessive crying can promote feelings of ‘living on the edge’, social isolation and ‘gradual introversion’ for families. Parents fear losing control.
Persistently crying babies is a common presentation in general practice with multiple possible causes. Evidence suggests that those parents and carers who complain to professionals that their baby cries excessively, actually do have a baby who cries more frequently and for longer than most. In addition, babies who cry excessively will do so despite the quality and level of parenting provided. Parents do not necessarily have an innate ability to parent effectively and most parents need support at some point.
Infant crying, along with poor sleep patterns and difficulties sleeping can have a significant impact on parents:
- Reduction in coping ability.
- Poor parent/child interaction.
- Reduction in self-esteem.
- Exhaustion.
- Frustration.
- Anger.
All of these can potentially be the trigger which, in some people, will manifest as frustration then aggression. Inconsolable crying can trigger a series of events that may lead to some parents shaking their baby with sometimes fatal consequences.
When faced with a consultation about a persistently crying baby, there are some useful steps you can take:
- CONSIDER CAUSES OF PERSISTENT CRYING
- Acutely unwell baby - follow usual procedures for management.
- Abusive head trauma suspected - arrange immediate specialist medical assessment and follow multiagency safeguarding procedures.
- Non-accidental injury suspected - follow multiagency safeguarding procedures.
- Feeding issues.
- Physical illness causes but baby is not acutely unwell.
- Cause unknown - under investigation.
- No obvious cause.
- CONSIDER IMPACT ON PARENTS/CARERS
- Exhaustion.
- Reduction in coping ability.
- Reduction in self-esteem.
- Poor parent/child interaction.
- Unsafe sleeping practices as parents may resort to this to stop the baby crying.
- Anger and frustration which could lead to some parents/carers shaking their baby.
- CONSIDER VULNERABILITIES
- Social isolation.
- Parents/carers with neurodiversity - consider impact of noise.
- Parental/carer mental health difficulties.
- Parental/carer substance misuse.
- Known safeguarding concerns e.g. domestic abuse.
- Other life stresses.
- ACTIONS
- Advise on strategies that may help to soothe a crying infant.
- NHS. Soothing a crying baby. 2022.
- Encourage parents/carers to look after their own wellbeing.
- NSPCC. Support for parents. 2024.
- Deliver the ICON message (a programme developed from the study of effective interventions and research into the prevention of Abusive Head Trauma (AHT).
- ICON. Babies cry, you can cope. 2024.
- Deliver Safe sleeping advice.
- The Lullaby Trust. Safe sleep advice. 2024.
- Consider use of the PAMIC tool (Potentiality for the Adult’s Mental Health to Impact on the Child) – see below.
- Act on any safeguarding concerns.
- Consider if a separate appointment is needed for parents/carers and their own health.
- Arrange follow-up.
- Advise on strategies that may help to soothe a crying infant.
ADDITIONAL PRACTICE POINT - When adults present with mental health difficulties and/or substance misuse difficulties, consider whether they are a current or prospective parent/carer, and ask if there is new baby in the household. Consider the impact of a new baby on parental mental health and wellbeing.
The PAMIC tool (Potentiality for the Adult’s Mental Health to Impact on the Child)
The PAMIC tool was developed by the Safeguarding Children Boards for Teeside. PAMIC stands for: Potentiality for the Adult’s Mental Ill Health to Impact on the Child. It can be used when considering how likely, and with what severity, an adult’s mental health will impact on a child. It involves the practitioner thinking about the nature of risk and also the protective factors for the child so it includes the practitioner’s professional judgement. When undertaking an assessment, consideration should always be given to any other current or previous safeguarding concerns. A summary of the tool is below:
- Delusional beliefs/ideas involving the child.
- Risk that child will be harmed as part of a suicide plan.
- The child is a target for parental aggression or rejection.
- Co-existing domestic abuse, drug or alcohol abuse.
- There is no other adult that can be depended upon to meet the needs of the child. (Children of lone parents or isolated parents are at greater risk as they are less likely to have an alternative caregiver when a parent is in crisis.)
- The child is the parent’s carer and this is impacting on the child’s welfare.
- The presenting mental ill health (including the effect of medication/treatment) is impacting on the parent/s’ capability to consistently meet the needs of the child.
- The parental mental health disorder is designated ‘untreatable’, either totally or within time-scales compatible with the child’s best interests.
- Parental learning disability rendering the child more vulnerable.
- Non-compliance or inconsistent compliance with treatment, reluctance or difficulty in engaging with necessary services, lack of insight into illness or its impact on the child.
- The child is vulnerable due to, for example, age, illness, disability or behavioural/emotional issues.
- Changes in the child’s behaviour since the onset of the parent/carer’s mental ill health.
- As events may change keep under review.
*Whilst the PAMIC tool’s original wording is ‘seek consent’, practitioners should be aware that consent is not required for a child safeguarding referral if there is a risk of significant harm to the child.
References
- NSPCC. Handle with care. 2019.
- ICON. Babies cry, you can cope. 2024.
- ICON. Abusive Head Trauma: The Case for Prevention. Updated 2023.
- NHS. Soothing a crying baby. 2022.
- Brighton and Sussex University Hospitals. Paediatric Clinical Practice Guideline: Crying and unsettled babies. 2015.
- NICE Clinical Knowledge Summaries. Colic – infantile. 2022.
- Tees Safeguarding Children Partnerships’ Procedures. Assessing & Responding to the Impact Parental Mental ill Health on Children. 2024.
Perplexing presentations and fabricated or induced illness (FII)
This is a particularly challenging area of safeguarding and there is often uncertainty about the criteria for suspecting or confirming PP/FII including how to document in medical records. The RCPCH published guidance on this area in 2021: ‘Perplexing Presentations (PP)/ Fabricated or Induced Illness (FII) in Children. RCPCH guidance.’ Whilst written primarily for paediatricians, this guidance is also of direct relevance to GPs and the RCGP were consulted during the development of the guidance.
IMPORTANT TO NOTE: Due to the challenges that cases of possible PP/FII present, if concerns about PP/FII arise within General Practice, there should be a discussion with the practice safeguarding lead and subsequently a discussion with safeguarding health professionals within the ICBs/ Health Authority/Health Board. These cases need careful multi-disciplinary involvement and no practitioner in general practice should attempt to manage these concerns on their own.
Summary of RCPCH guidance: Perplexing Presentations (PP)/Fabricated or Induced Illness (FII) in Children, relevant to general practice
Terminology has changed over time with the term ‘Munchausen syndrome by proxy’ no longer being used.
The terminology now used is:
The essence of alerting signs is the presence of discrepancies between reports, presentations of the child and independent observations of the child, implausible descriptions and unexplained findings or parental behaviour.
The parent does not necessarily intend to deceive, and their motivations may not be initially evident. Munchausen syndrome by proxy; paediatric condition falsification; medical child abuse; parent-fabricated illness in a child; (factitious disorder imposed on another, when there is explicit deception)
Features of PP and FII
Parent/caregiver motivation and behaviour
- Clinical experience and research indicate that the mother is nearly always involved or is the instigator of FII. Involvement of fathers is variable.
- FII is based on the parent’s underlying need for their child to be recognised and treated as ill or more unwell/more disabled than the child actually is (when the child has a verified disorder, as many of the children do).
- There are two possible, and very different, motivations underpinning the parent’s need: the parent experiencing a gain and the parent’s erroneous beliefs.
- In the first, the parent experiences a gain (not necessarily material) from the recognition and treatment of their child as unwell. The parent is thus using the child to fulfil their needs, disregarding the effects on the child. There are a number of different gains - some psychosocial such as the sympathetic attention they receive and some material such as financial support for care of the child, improved housing, holidays, assisted mobility and preferential car parking.
- The second motivation is based on the parent’s erroneous beliefs, extreme concern and anxiety about their child’s health (eg nutrition, allergies, treatments). This can include a mistaken belief that their child needs additional support at school and an Education Health and Care Plan (EHCP). In contrast to typical parental concern, the parent exhibiting such behaviour cannot be reassured by health professionals or negative investigations.
In FII, parents’ needs are primarily fulfilled by the involvement of doctors and other health professionals. The parent’s actions and behaviours are intended to convince health professionals, particularly paediatricians, about the child’s state of health. It is important to note that, as is common in child neglect, the parent is not usually ill-intentioned towards their child per se. Nonetheless, they may cause their child direct harm, unintentionally or in order to have their assertions reinforced and believed.
Parents engage health professionals in the following ways:
- Presenting and erroneously reporting the child’s symptoms, history, results of investigations, medical opinions, interventions and diagnoses. This is the most common form. There may be exaggeration, distortion, misconstruing of innocent phenomena in the child, or invention and deception. In their reports, the parents may not be actually intending to deceive, such as when they hold incorrect beliefs and are over-anxious, to the child’s detriment.
- Parent’s physical actions which nearly always include an element of deception. This is a less common way. Actions range from falsifying documents, through interfering with investigations and specimens such as putting sugar or blood in the child’s urine specimen, interfering with lines and drainage bags, withholding food or medication from the child and, at the extreme end, illness induction in the child. All of these are carried out in order to convince health professionals, especially paediatricians, about the child’s poor state of health or illness.
Support groups and social media provide an important source of support for parents and families where there is childhood illness. Paediatricians and parents should, however, be aware that some support groups also exist for a number of conditions about which there is divided medical opinion. Furthermore, some social media/support groups may post inaccurate information, discuss diagnoses and how to obtain them, which can lead to harm.
While parental mental ill-health is not a prerequisite for FII, if present it may help to explain the motivations and behaviours of some of the parents as well as indicating prognosis for change. Personality disorders are most likely to be found in parents who derive a clear gain from having their child regarded as ill/more ill. Anxiety disorders may lead the parent to have unfounded anxieties about their child’s health, to an extent which is harmful to the child. Rarely a psychotic illness or Autism Spectrum Disorder (ASD) in the parent may underpin fixed beliefs about the child’s ill-health. Some parents have illness anxiety disorder related to themselves, previously called hypochondriasis. Others have a somatic symptom disorder, in which the person genuinely feels pain or other symptoms which are, however, not based on any identified pathology and can be related to unrecognised or unarticulated underlying emotional difficulties and conflicts. In malingering and factitious disorder, there is unacknowledged deception about the reported symptoms and signs. Both these are associated with gain for the person, the former material gain and the latter psychological or other gain.
Doctors’ involvement
Within this challenging field of work, there is evidence that paediatricians and other health professionals play a role in inadvertently contributing to harm to the child. Most of what doctors do in the management of children, including where the presentation is not understood, is regarded as good medical practice. However, in children with unrecognised FII, some of these actions may contribute to iatrogenic harm. In children with FII, iatrogenic harm is caused by the doctor’s need and wish to trust and work with parents. Even in cases where FII might be suspected, there is still a tendency to believe parents, to avoid complaints, and sometimes uncertainty about how to proceed in what are usually complex cases. A child often has an existing medical diagnosis, or had started out with an underlying illness, which will make assessment more difficult. The parent’s accounts may therefore be true, partially true, or mixed with other accounts that are fabricated or misconstrued. This makes it more difficult to explore their credibility. There is no escaping the reality of the impact on the child in these circumstances however. All doctors need therefore to be thorough in appraising parental requests for further opinions and repeat investigations, and parental failures to bring children to appointments. A doctor’s unease, uncertainty or worry may lead to over-medicalisation of the child’s reported symptoms which must be avoided wherever possible.
Harm to the child
Harm to the child can take several forms. The following three aspects need to be considered when assessing potential harm to the child:
- The child undergoes repeated (unnecessary) medical appointments, examinations, investigations, procedures & treatments, which are often experienced by the child as physically and psychologically uncomfortable or distressing.
- Genuine illness may be overlooked by doctors due to repeated presentations.
- Illness may be induced by the parent (e.g. poisoning, suffocation, withholding food or medication) potentially or actually threatening the child’s health or life.
- The child has limited/interrupted school attendance and education.
- The child’s normal daily life activities are limited.
- The child assumes a sick role (e.g. with the use of unnecessary aids, such as wheelchairs).
- The child is socially isolated.
- The child may be confused or very anxious about their state of health.
- The child may develop a false self-view of being sick and vulnerable and adolescents may actively embrace this view and then may become the main driver of erroneous beliefs about their own sickness. Increasingly young people caught up in sickness roles are themselves obtaining information from social media and from their own peer group which encourage each other to remain ‘ill’.
- There may be active collusion with the parent’s illness deception.
- The child may be silently trapped in falsification of illness.
- The child may later develop one of a number of psychiatric disorders and psychosocial difficulties.
Severity also needs to be considered - severity of the parent’s actions and severity of harm to the child. In assessing the severity of the situation, it is important to focus on the harmful effects on the child. Potential harm to siblings also needs to be considered. There have also been reports of FII perpetrators abusing spouses or animals.
Alerting signs to possible FII
Alerting signs are not evidence of FII. However, they are indicators of possible FII (not amounting to likely or actual significant harm) and, if associated with possible harm to the child, they amount to general safeguarding concerns. Alerting signs can be recognised by a wide range of professionals such as health visitors, general practice clinicians, teachers and educational staff, paediatricians or CAMHS professionals.
The essence of alerting signs is the presence of discrepancies between reports, presentations of the child and independent observations of the child, implausible descriptions and unexplained findings or parental behaviours. Alerting signs may be recognised within the child or in the parent’s behaviour. A single alerting sign by itself is unlikely to indicate possible fabrication. It is important to look at the overall picture which includes the number and severity of alerting signs.
- Alerting signs in the child:
- Reported physical, psychological, or behavioural symptoms and signs not observed independently in their reported context.
- Unusual results of investigations (e.g. biochemical findings, unusual infective organisms).
- Inexplicably poor response to prescribed treatment.
- Some characteristics of the child’s illness may be physiologically impossible e.g. persistent negative fluid balance, large blood loss without drop in haemoglobin.
- Unexplained impairment of child’s daily life, including school attendance, aids, social isolation.
- Alerting signs in parent behaviour:
- Parent/s’ insistence on continued investigations instead of focusing on symptom alleviation when reported symptoms and signs not explained by any known medical condition in the child.
- Parent/s’ insistence on continued investigations instead of focusing on symptom alleviation when results of examination and investigations have already not explained the reported symptoms or signs.
- Repeated reporting of new symptoms.
- Repeated presentations to and attendance at medical settings including Emergency Departments.
- Inappropriately seeking multiple medical opinions.
- Providing reports by doctors from abroad which are in conflict with UK medical practice.
- Child repeatedly not brought to some appointments, often due to cancellations.
- Not able to accept reassurance or recommended management, and insistence on more, clinically unwarranted, investigations, referrals, continuation of, or new treatments (sometimes based on internet searches).
- Objection to communication between professionals.
- Frequent vexatious complaints about professionals.
- Not letting the child be seen on their own.
- Talking for the child/child repeatedly referring or deferring to the parent.
- Repeated or unexplained changes of school (including to home schooling), of GP or of paediatrician/health team.
- Factual discrepancies in statements that the parent makes to professionals or others about their child’s illness.
- Parents pressing for irreversible or drastic treatment options where the clinical need for this is in doubt or based solely on parental reporting.
Adverse childhood experiences
When working with children and their families where there are perplexing illnesses or concerns about fabricated or induced illness, professionals should explicitly explore whether the child is currently experiencing, or has previously experienced, adverse childhood experiences such as physical, sexual or emotional abuse, neglect, domestic abuse, child sexual or criminal exploitation, bereavement, parental/caregiver alcohol or drug misuse, severe parental mental health issues, or a parent going to prison. Adverse childhood experiences (ACEs) such as these can have a detrimental impact on the physical, mental and emotional wellbeing of a child. Professionals should also be mindful that parents and caregivers may themselves have experienced adverse childhood experiences.
Response to alerting signs
- An urgent safeguarding referral must be made to children’s social care as a case of likely significant harm due to suspected of actual FII. This should lead to a strategy discussion.
- Document concerns in the child’s record (mark not for online access if applicable in UK nation you work in).
- All practitioners should be mindful of situations where to inform the parents of the referral would place a child at increased risk of harm. In this situation, carers would not be informed of the referral before a multiagency discussion has taken place.
- If very urgent protection of the child is needed, the Police can also be contacted.
- This situation calls for a carefully planned response and should be led by the responsible consultant (either paediatric or CAMHS).
- If the concerns initially arise in general practice, a referral should be made to paediatrics or CAMHS (dependent on the presentation) as the response to perplexing presentations should be led by the Responsible Paediatric or CAMH Consultant with advice from the Named Doctor and health safeguarding team.
- A multi-disciplinary approach is required.
- GPs will be asked to collate the child’s medical/health information from a general practice perspective, clarifying what has been reported and what has been observed.
- Consensus about the child’s state of health needs to be reached between all health professionals involved with the child and family, including GPs, Consultants, private doctors and other significant professionals who have observations about the child, including education and children’s social care if they have already been involved. A multi-professional meeting is required in order to reach consensus.
All professionals need to reach a consensus on the following issues:
Either:
- That all the alerting signs and problems are explained by verified physical and/or psychiatric pathology or neurodevelopmental disorders in the child and there is no FII (false positives).
- Medically unexplained symptoms from the child free from parental suggestion.
- That there are perplexing elements, but the child will not come to harm as a result.
- That any verified diagnoses do not explain all the alerting signs.
- The actual or likely harm to the child and or siblings.
And agree all of the following:
- Whether further investigations and seeking of further medical opinions is warranted in the child’s interests.
- How the child and the family need to be supported to function better alongside any remaining symptoms, using a Health and Education Rehabilitation Plan.
- If the child does not have a secondary care paediatric consultant involved in their care, consideration needs to be given to involving local services.
- The health needs of siblings.
- Next steps in the eventuality that parents disengage or request a change of paediatrician in response to the communication meeting with the responsible paediatric consultant about the consensus reached and the proposed Health and Education Rehabilitation Plan.
There also needs to be a discussion and consensus on whether a referral to children’s social care is needed.
It is essential that GPs are kept fully informed and involved in the management of children with perplexing presentations or where there are concerns about FII so they can support children and their families as appropriate as well as work in partnership with other professionals involved to ensure the best outcomes for children.
There is a useful summary diagram in the RCPCH guidance on page 34.
Record keeping
- All notes about a child’s condition should clearly state who reported the concerns, what was observed, and by whom.
- Records of key discussions and safeguarding supervision notes about the child’s care should be kept within every organisation’s main health record pertaining to the child to ensure that the child does not come to further harm.
- A formal agreed consensus document or minutes of professionals’ meetings shared across all participant organisations will avoid discrepancies in individual’s recollection/recording across the multi-professional group, and is preferable to individual entries in notes.
- These records should be factual and agreed by all parties present. Records must provide a clear statement of what has and has not been discussed with parents.
- Subject access requests (SARs) from parents in PP and FII cases are not uncommon. They are easier to manage if there has been open communication with parents previously. If it is thought that the subject access request may result in concerns about the child’s welfare, appropriate legal advice needs to be sought about what material should be disclosed and any material to be withheld.
- In general practice, entries related to safeguarding concerns should all be marked not for online access.
Key points
- Working with children and families where there are medically unexplained symptoms, perplexing presentations or concerns about fabricated or induced illness, can be challenging.
- These situations require a multi-disciplinary approach and should not be managed solely in general practice – a referral to paediatrics and/or CAMHS will be needed.
- When concerns arise in general practice, there should be discussion with the practice safeguarding lead and subsequently a discussion with safeguarding health professionals within the ICBs/Health Authority/Health Board.
- When a safeguarding referral is indicated, advice should be taken from safeguarding professionals as to whether the parents should be informed or not.
- Urgent safeguarding action should be taken if there is a concern that there is an immediate serious risk to the child’s health/life. This includes making an urgent safeguarding referral to children’s social care. It can also involve contacting the police if there is an immediate threat to life.
References
Neglect
Neglect is the persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of the child’s health or development. In 2019, neglect was the most common category of abuse for child protection plans in England and the second most common for the child protection register in Wales.
Neglect can take many different forms and can include:
- Physical neglect: a failure to take care of a child’s basic needs which includes providing food, shelter, clothes and keeping the child clean and hygienic. It can also include exclusion from home or abandonment.
- Supervisory neglect: a failure to provide an adequate level of supervision and guidance to ensure a child’s safety and protection from harm.
- Nutritional neglect: a failure to provide adequate calories or nutritional intake for normal growth (also sometimes called ‘failure to thrive’). At its most extreme, nutritional neglect can take the form of malnutrition.
- Emotional neglect: a failure to meet a child’s emotional needs. It can include emotional unavailability and unresponsiveness of the parent which can be particularly damaging to a child. It can occur if the parent has mental health difficulties, substance or alcohol misuse or is persistently preoccupied with other difficulties such as domestic abuse. Emotional neglect can result in long-lasting mental health problems and is a particularly hidden form of maltreatment.
- Medical neglect: this involves a parent or carer minimising or ignoring children’s illness or health (including oral health) needs, and failing to seek medical attention or administrating medication and treatments. This is equally relevant to expectant mothers who fail to prepare appropriately for the child’s birth, fail to seek ante-natal care, and/or engage in behaviours that place the baby at risk through, for example, substance misuse.
- A failure to provide suitable education including support to attend school. This can result in poor educational achievement due to missed education.
Neglect can be really difficult to spot. It is often a chronic issue rather than an acute one. Having one of the signs of neglect doesn't necessarily mean a child is being neglected. But if you notice multiple signs that last for a while, they might show there's a serious problem. It is also important to recognise that some of these signs of neglect can overlap with living in poverty and deprivation and there should be a clear distinction in response to families living in poverty who need help and support and families where there are concerns about neglect where child safeguarding measures need to be considered alongside help and support.
Some of the challenges of neglect that make it harder for practitioners to recognise that a threshold for statutory intervention has been reached are:
- The chronic nature of this form of maltreatment practitioners can become used to how a child is presenting and fail to question a lack of progress.
- Unlike physical abuse for example, the experience of neglect rarely produces a crisis that demands obvious and immediate action.
- Neglect can in some cases be challenging to identify because of the need to look beyond individual parenting episodes and consider the persistence, frequency, extent and pervasiveness of parenting behaviour which may make them harmful and abusive.
- There is a reluctance to pass judgement on patterns of parental behaviour particularly when deemed to be culturally embedded or when associated with social disadvantages such as poverty.
- The child may not experience neglect in isolation, but alongside other forms of abuse.
- Being smelly or dirty.
- Being hungry or not given money for food.
- Having unwashed clothes.
- Having the wrong clothing, such as no warm clothes in winter.
- Having frequent and untreated nappy rash in infants.
- Anaemia.
- Body issues, such as poor muscle tone or prominent joints.
- Medical or dental issues.
- Missed medical appointments, such as for vaccinations.
- Not given the correct medicines.
- Poor language or social skills.
- Regular illness or infections.
- Repeated accidental injuries, often caused by lack of supervision.
- Skin issues, such as sores, rashes, flea bites, scabies or ringworm.
- Thin or swollen tummy.
- Tiredness.
- Untreated injuries.
- Weight or growth issues.
- Being left alone for a long time.
- Taking on the role of carer for other family members.
- Becoming clingy.
- Becoming aggressive.
- Being withdrawn, depressed or anxious.
- Changes in eating habits.
- Displaying obsessive behaviour.
- Finding it hard to concentrate or take part in activities.
- Missing school.
- Showing signs of self-harm.
- Using drugs or alcohol.
Neglect in affluence
It is important to recognise that children in affluent families can also experience neglect, in particular emotional neglect. These children often have excellent housing, a nutritious diet, first-class educational opportunities and access to a range of enrichment opportunities. A study carried out by Professor Claudia Bernard entitled “An Exploration of How Social Workers Engage Neglectful Parents from Affluent Backgrounds in the Child Protection System” highlighted some of the challenges in this area of safeguarding:
- The findings revealed that thresholds for neglect are not always understood, which posed challenges for effectively safeguarding children at risk of significant harm in privileged families.
- The vast majority of the cases described by the participants concerned emotional neglect, although other forms of maltreatment, such as sexual abuse, child sexual exploitation and emotional abuse, were also identified.
- Commonly-encountered cases involved struggling teenagers in private fee-paying and boarding schools, who were often isolated from their parents physically and emotionally, and had complex safeguarding needs.
- Participants gave many examples to show how parents had the financial resources to access psychological support through private care providers to address their children’s emotional and behavioural problems; some practitioners viewed this as a positive outcome for the child, but some saw this as a way for the parents to opt out of the statutory child protection system, and to thus slip under the radar of children’s services.
- All of the participants described difficulties in maintaining focus on the child because of the way that parents used their status and social capital to resist child protection intervention, and many also displayed a sense of entitlement to do as they pleased and that they know best.
- Participants consistently cited that highly resistant parents were more likely to use legal advocates or the complaints procedures to challenge social workers.
- All of the participants also experienced the challenges of interagency working with private fee-paying and boarding schools when child protection concerns were raised.
The study also outlined helpful practice:
- Considerable experience, practice wisdom and knowledge of neglect were essential in relation to working with highly resistant parents who had the resources to challenge social workers’ decision-making.
- Skills, knowledge and competence: all of the participants highlighted the important role that supportive managers and good supervision played in helping them to effectively intervene in affluent families.
- Participants cite the organisational cultures of support, purposeful informal conversations about the case with colleagues, good supervision, knowledge and confidence and responsive managers, themed learning activities, as key to their ability to work in this complex field.
This briefing on Safeguarding in Affluent Communities from Kingston and Richmond Safeguarding Children Partnership also gives a useful summary.
Impact of neglect
The impact of neglect can be significant and life-changing. The devastating impact of neglect, particularly in early years, is often underestimated.
The effects can be short or long-term and can include:
- problems with brain development
- taking risks, like running away from home, using drugs and alcohol or breaking the law
- getting into dangerous relationships
- difficulty with relationships later in life, including with their own children
- a higher chance of having mental health problems, including depression.
Other factors and life circumstances can make it harder for parents and carers to meet their child’s needs such as domestic abuse, parental drug or alcohol abuse, parental experience of childhood abuse including neglect, parental learning disabilities, parental mental and physical health problems, living in poverty and being isolated with little or no family or community support.
Was not brought (children)
Children not being brought to health appointments can be a sign of neglect or other abuse or that a family might need additional support. The term ‘was not brought’ is now widely used across health regarding children rather than ‘did not attend’ as it more accurately conveys that children, in general, need to be brought to health appointments (there are exceptions to this such as older teenagers who may make appointments themselves).
There are many reasons why a child may not be brought to a health appointment e.g. a parent forgot the appointment, the child is now better, a parent got the wrong appointment time/date, they did not know about the appointment (especially secondary care appointments). Generally, in most cases, a one-off missed appointment would not be a concern. However, patterns and context are very important. For example, a child who is on a child protection plan for neglect who is not brought to one health appointment should raise the practitioner's level of concern and prompt action to ensure the welfare of the child. Practices should have a practice policy relating to children not being brought to appointments.
Children not brought to appointments should be coded 'was not brought' rather than 'did not attend'.
Secondary care and other health providers should have their own ‘was not brought’ policies that they follow.
Every time a child is not brought to a health appointment, the practitioner should consider what the impact on the welfare of the child could be, whether there are any other concerns within the family and take action if necessary. A checklist of issues to consider when a child is not brought to an appointment: (practices may consider doing this with the admin/reception team to aid the clinician):
- What was the purpose of the appointment (may not be known)? If the purpose is known, what could the potential impact of the missed appointment be on the child's welfare?
- Does the child have any ongoing physical or mental health problems?
- Are there other health appointments that the child has not been brought to? Is there a pattern of missed appointments?
- Are there a high volume of Emergency Department and GP out of hours attendances?
- Is the child on a child protection plan or a looked-after child?
- Are there any safeguarding concerns documented in the child's records?
- Are there any siblings and if so, is there a pattern of health appointments that the children have not been brought to?
- Are there any concerns about the parent/carer that could impact on their ability to bring the children to health appointments, for example physical or mental health problems, drug and alcohol issues, domestic abuse, safeguarding concerns.
If there is any concern about the child following the completion of the checklist, action needs to be taken proportionate to the level of concern. This could include:
- asking the reception staff to contact the parents to arrange another appointment
- contacting the parent/child yourself to discuss why the child has not been brought and make a further assessment
- contacting other health professionals such as a health visitor, to share information and concerns to aid further decisions
- contacting Children's Social Care (Health and Social Care Trust in Northern Ireland), especially if the missed appointments are adversely impacting the child’s health.
In all cases, it is important to document your actions and reasons for them.
The video ‘Rethinking Did Not Attend’ was developed in Nottingham to encourage practitioners to identify children as ‘Was Not Brought’ rather than ‘Did Not Attend’ when they are not presented at medical appointments.
References
- Department for Education. Working together to safeguard children. Updated 2024.
- Office for National Statistics. Child neglect in England and Wales: year ending March 2019. 2020.
- Wales Safeguarding Procedures. Safeguarding children from neglect. 2021
- NSPCC. Neglect. 2024.
- Professor Claudia Bernard. Goldsmiths University of London. An Exploration of How Social Workers Engage Neglectful Parents from Affluent Backgrounds in the Child Protection System.
- Kingston and Richmond Safeguarding Children Partnership. Safeguarding in Affluent Communities.
Emotional abuse
Emotional abuse is the persistent emotional maltreatment of a child so as to cause severe and persistent adverse effects on the child’s emotional development.
It may involve conveying to a child that they are worthless or unloved, inadequate, or valued only insofar as they meet the needs of another person.
It may include not giving the child opportunities to express their views, deliberately silencing them, or making fun of what they say or how they communicate.
It may feature age or developmentally inappropriate expectations being imposed on children. These may include interactions that are beyond a child’s developmental capability, as well as overprotection and limitation of exploration and learning, or preventing the child participating in normal social interaction. It may involve seeing or hearing the ill-treatment of another.
It may involve serious bullying (including cyber bullying), causing children frequently to feel frightened or in danger, or the exploitation or corruption of children. Some level of emotional abuse is involved in all types of maltreatment of a child, though it may occur alone.
Signs of emotional abuse can be different for children at different ages.
- Being overly-affectionate to strangers or people they don't know well.
- Seeming unconfident, wary or anxious.
- Not having a close relationship or bond with their parent.
- Being aggressive or cruel towards other children or animals.
- Using language you wouldn't expect them to know for their age.
- Acting in a way or know about things you wouldn't expect them to know for their age.
- Struggling to control their emotions.
- Having extreme outbursts.
- Seeming isolated from their parents.
- Lacking social skills.
- Having few or no friends.
Impact of emotional abuse
Over time, emotional abuse can have serious long term effects on a child’s social, emotional and physical health and development and can include:
- Behaviour problems such as wanting attention, not caring how they act, trying to make people dislike them, developing risky behaviour.
- Impact on emotional development such as how they feel, express and control emotions. They can find it difficult to make and maintain healthy relationships in later life.
- Mental health problems such as depression, anxiety, suicidal thoughts, eating disorders and self-harm.
As with neglect, there are other factors and life circumstances which can make it more difficult for parents and carers to provide a safe and loving home for their children, such as relationship or family problems, money problems or unemployment, poverty, mental health issues, drug or alcohol addiction and domestic abuse.
References
- Department for Education. Working together to safeguard children. Updated 2024.
- NSPCC. Emotional abuse. 2024.
Sexual abuse
Sexual abuse involves forcing or enticing a child or young person to take part in sexual activities, not necessarily involving a high level of violence, whether or not the child is aware of what is happening. The activities may involve physical contact, including assault by penetration (for example, rape or oral sex) or non-penetrative acts, such as masturbation, kissing, rubbing, and touching outside of clothing. They may also include non-contact activities, such as involving children in looking at, or in the production of, sexual images, watching sexual activities, encouraging children to behave in sexually inappropriate ways, or grooming a child in preparation for abuse. Sexual abuse can take place online, and technology can be used to facilitate offline abuse. Sexual abuse is not solely perpetrated by adult males. Women can also commit acts of sexual abuse, as can other children.
When a child or young person is sexually abused, they're forced, tricked or manipulated into sexual activities. They might not understand that what's happening is abuse or that it's wrong for the abuser to do this to them. They might be afraid to tell someone or behave as though this is normal for them to experience, both are valid for the child to be displaying. Sexual abuse can happen anywhere – and it can happen in person or online.
It's never a child's fault they were sexually abused – it is important to make sure children know this. Knowing the signs of sexual abuse can help give a voice to children.
Research indicates that only one in three children who had been sexually abused by an adult told anyone what was happening. For those abused by another child this was even less, with five out of six not speaking to anyone. This means that the majority of children being sexually abused do not tell anyone during childhood.
There are many barriers to children sharing their experiences of sexual abuse and it isn’t likely that a child will feel able to tell professionals directly what is happening or recognise that what is happening to them is abuse. Instead children may show other emotional, behavioural and physical signs.
There are numerous signs that could indicate a child is being sexually abused. Some of these signs are not specific to sexual abuse, but can be suggestive that a child is experiencing some form of distress which could be related to experience of any type of abuse or other difficult life circumstances.
Some of the signs of sexual abuse are included in the table below.
- Avoiding being alone with or frightened of people or a person they know.
- Language or sexual behaviour you wouldn’t expect them to know.
- Having nightmares or bed-wetting.
- Alcohol or drug misuse.
- Self-harm.
- Changes in eating habits or developing an eating problem.
- Changes in their mood, feeling irritable and angry, or anything out of the ordinary.
- Change in normal behaviour for the child, for example suddenly not attending education or avoiding wanting to go home/running away.
- Bruises.
- Bleeding, discharge, pains or soreness in their genital or anal area.
- Sexually transmitted infections, including in the throat.
- Pain/soreness in throat.
- Pregnancy.
- Difficulty in walking/sitting that is not usual for the child.
- spend a lot more or a lot less time than usual online, texting, gaming or using social media
- seem distant, upset or angry after using the internet or texting
- be secretive about who they're talking to and what they're doing online or on their mobile phone
- behaving as though they have to be online at a certain time, or rushing to get on their phone
- have lots of new phone numbers, texts or email addresses on their mobile phone, laptop or tablet
- expressing the need for money, this may be used if they are being blackmailed.
The Centre of Expertise on Child Sexual Abuse is an amazing resource on preventing and better responding to child sexual abuse. Much of the information in this section of the toolkit is from their resources. They have a number of very useful resources such as:
- Signs and indicators of child sexual abuse template.
- Communicating with children guide.
- Supporting parents and carers.
- Sibling sexual abuse and behaviour.
Talking about child sexual abuse
This can seem challenging but we can apply the same communication principles that we use for many other types of difficult conversations we have in general practice. Talking about child sexual abuse: tackling professional concerns guidance aims to address some professional concerns around talking to children about child sexual abuse and give you the confidence you need to help you with these conversations.
Working with families affected by child sexual abuse
The Centre of Expertise on Child Sexual Abuse has produced a guide about working with families where sexual abuse has already been reported or concerns have already been raised. This guidance outlines that parents also need support, because discovering that their child may have been sexually abused is one of the most devastating events a parent can experience. They are likely to be overwhelmed by shock, anger, confusion and disbelief. They may find it particularly difficult to come to terms with what has happened if the abuse was carried out by their partner or another of their children. If they have other pre-existing vulnerabilities (resulting from domestic abuse, disabilities, mental ill health or substance misuse, for example), their health and wellbeing may suffer further.
Support can help parents to mitigate the abuse’s impact on their child, helps engagement with services and helps parents to protect their child from further abuse. There can be a significant impact on parents’ mental and physical health and their relationships and they will need long term support.
Online child sexual abuse and exploitation
Child sexual exploitation
The NSPCC provides useful information about Child Sexual Exploitation:
Child sexual exploitation (CSE) is a type of sexual abuse. It happens when a child or young person is coerced, manipulated or deceived into sexual activity in exchange for things that they may need or want like gifts, drugs, money, status and affection. Children and young people are often tricked into believing they're in a loving and consensual relationship so the sexual activity may appear consensual. This is called grooming and is a type of abuse. They may trust their abuser and not understand that they're being abused. CSE does not always involve physical contact, and can also occur through the use of technology.
Children and young people can be trafficked into or within the UK for sexual exploitation. They're moved around the country and abused by being forced to take part in sexual activities, often with more than one person. Young people in gangs can also be sexually exploited.
Sometimes abusers use violence and intimidation to frighten or force a child or young person, making them feel as if they've no choice. They may lend them large sums of money they know can't be repaid or use financial abuse or blackmail to control them.
Anybody can be a perpetrator of CSE, no matter their age, gender or race. The relationship could be framed or viewed as friendship, someone to look up to or romantic. Children and young people who are exploited may also be made to 'find' or coerce others to join groups.
It's important to recognise that although the age of consent is 16 years old, children and young people over the age of 16 can be exploited. Child sexual exploitation is a very complex form of abuse. It can be difficult for parents and carers to understand and hard for the young person to acknowledge that they are being exploited.
CSE can happen in person or online.
Below are some signs of child sexual exploitation which we have taken from the NSPCC.
Child criminal exploitation and gangs
Criminal exploitation is a form of child abuse where children and young people are manipulated and coerced into committing crimes.
The most common form of child criminal exploitation is ‘county lines’. This refers to gangs and organised criminal networks involved in exporting illegal drugs around the UK using dedicated mobile phone lines or other forms of a ‘deal line’. Gangs exploit children and vulnerable adults into moving drugs from a hub, normally a large city, into other markets such as suburban areas and market and coastal towns. Gangs will often use coercion, intimidation, violence (including sexual violence) and weapons.
Children as young as 12 years old have been criminally exploited into carrying drugs for gangs. This can involve children being trafficked away from their home area, staying in accommodation and selling and manufacturing drugs. This can include: Airbnb and short term private rental properties, budget hotels or the home of a drug user, or other vulnerable person, that is taken over by a criminal gang- this may be referred to as cuckooing.
Victims may have been criminally exploited even if the activity appears consensual. Child criminal exploitation does not always involve physical contact, it can also occur using technology like social media.
Common characteristics of child exploitation are:
- control, coercion, intimidation, threats of violence, and violence
- associating with other children involved in exploitation
- suffering from changes in emotional well-being and/or behaviour
- misuse of drugs and alcohol
- appearing with unexplained gifts, money or new possessions
- going missing for periods of time or regularly coming home late
- regularly missing school or education, or not taking part in education.
Gang membership is complex. For some children, it represents little more than a loose social connection - a hashtag for Instagram. Yet this is the exception. The criminal gangs operating in England are complex and ruthless organisations, which use sophisticated techniques to groom children and chilling levels of violence to keep them compliant. They prey upon marginalised children who have often been let down by multiple agencies. As well as gang members, there are many gang associates and others on the periphery, not given the status of membership but who are being groomed and exploited by gangs. Many of these children don’t feel that they have any choice about their situation.
All children can fall victim to gangs and criminal exploitation. However, the Children’s Commissioner report, ‘Keeping kids safe. Improving safeguarding responses to gang violence and criminal exploitation’, shows that on the whole gang members are highly vulnerable children with a range of factors increasing their risk of being drawn into gangs.
The children at greatest risk are children who have multiple interlinked vulnerabilities – both at the individual level (such as mental health or special educational needs) and the family level (such as abuse and neglect). Gangs exploit children experiencing three particular risk factors:
- Risks around their home environment such as domestic abuse, unstable housing, neglect or abuse, substance or alcohol misuse.
- Child-level characteristic: special educational needs, poor mental health, being bullied, being excluded from school, being denied CAMHS input.
- Children at risk because of a failure of institutions to respond adequately, for example children excluded from school or deprived of much-needed mental health support.
Once a child is within a gang, extricating them can be very difficult. While gangs may entice children with money and bribes, once children are involved, they use threats, violence and intimidation to keep children under their control. These children may need a range of interventions, but the single most important thing is for them to have a relationship with at least one trusted adult who can help divert them away from gangs and access other services. Because of this, the children most at risk are those who are isolated and invisible to the authorities, generally let down by multiple agencies.
References
- Department for Education. Working together to safeguard children. Updated 2024.
- Centre of expertise on child sexual abuse. Signs and indicators of child sexual abuse. 2024.
- Centre of expertise on child sexual abuse. Communicating with children. 2024.
- Centre of expertise on child sexual abuse. Supporting parents and carers. 2024.
- NSPCC. Sexual abuse. 2024.
- NSPCC. Child Sexual Exploitation. 2024
- NSPCC. Criminal Exploitation and Gangs. 2024.
- Children’s Commissioner. Report: Keeping kids safe. Improving safeguarding responses to gang violence and criminal exploitation. 2019.
- Home Office. Child exploitation disruption toolkit. 2022.
- Stop it now. Preventing harmful sexual behaviour.
- NSPCC. Problematic and Harmful sexual behaviour. 2024.
- Centre of expertise on child sexual abuse. Key messages from research on children and young people who display harmful sexual behaviour. 2024.
Harmful sexual behaviour
Sexual behaviours in children and young people can be seen on a continuum ranging from ‘normal’ and developmentally appropriate, from ‘inappropriate’ and ‘problematic’, to ‘abusive’ and ‘violent’.
Harmful sexual behaviour (HSB) is a term used to describe sexual actions that are outside what is safe for a young person’s stage of development. It includes actions that can harm either the child or young person themselves, or another person.
It can include:
- frequently and intentionally accessing age-inappropriate sexual material online
- using inappropriate language
- undertaking mutual sexual activity they are not ready for with peers
- sending and receiving illegal images
- sexual interactions where there are significant power differences, lack of consent, or through force or threats
- engaging in abusive or sexually violent sexual behaviour online or offline.
Peer-on-peer sexual abuse
Peer-on-peer sexual abuse is a form of harmful sexual behaviour where sexual abuse takes place between children of a similar age or stage of development. Child-on-child sexual abuse is a form of harmful sexual behaviour that takes place between children of any age or stage of development.
Research tells us:
- Under 18s are responsible for at least a third of recorded sexual offences against children and young people in the UK.
- Boys in early adolescence, around the time puberty starts, tend to display the most harmful sexual behaviour, although younger children and girls do sometimes engage in these behaviours too.
- Girls tend to be over-represented amongst the victims of harmful sexual behaviour.
- Those with learning disabilities and autism also tend to be over-represented amongst young people who have displayed harmful sexual behaviour.
- Around half of young people who have displayed harmful sexual behaviour have experienced sexual abuse themselves.
The vast majority of young people do not persist with these behaviours into adulthood. Children and young people who display harmful sexual behaviour are more likely than other young people to have a history of maltreatment and family difficulties. Some children and young people displaying harmful sexual behaviour have been sexually abused themselves, but most victims of sexual abuse do not go on to abuse others. It is a history of child maltreatment, rather than sexual abuse specifically, that is most strongly associated with later sexual offending.
Understanding the sexual behaviour of children and young people
The ‘Stop it now’ organisation has range of useful resources to help understand where a child’s sexual behaviour is expected for their age, or if it could harm other people.
Warning signs of harmful sexualised behaviour in children:
- seeks out the company of younger children and spends an unusual amount of time in their company
- takes younger children to 'secret' places or hideaways or plays 'special' games with them, for example, doctor and patient, removing clothing, especially games unusual to their age
- insists on hugging or kissing a child when the child does not want to
- tells you they do not want to be alone with a child or becomes anxious when a particular child comes to visit
- frequently uses aggressive or sexual language about adults or children
- shows sexual material to younger children
- makes sexually abusive telephone calls
- shares alcohol or drugs with younger children or teens
- views sexual images of under 18s on the internet or elsewhere
- exposes his or her genitals to younger children
- forces sex on another adolescent or child.
It is important to remember that not all sexual behaviour involving young people is problematic. Behaviour is more likely to be normative if it is:
- between young people of a similar age and developmental stage
- voluntary
- mutual
- limited in type and frequency
- balanced by a curiosity about other things
- light-hearted and spontaneous.
Responding to concerns about harmful sexual behaviour
There is little research on specific interventions for children who display harmful sexual behaviour, but there are indications that structured, holistic and family-oriented approaches are of value. Given that many young children displaying harmful sexual behaviour have themselves experienced abuse, interventions identified as effective with child victims are relevant: these include developmentally appropriate behavioural or cognitive behavioural approaches which are also trauma-informed and multi-systemic, intervening with both the child and their wider family. Research highlights the damaging effects of stigmatising young people as ‘mini adult sex offenders’, which may even increase the likelihood of reoffending.
It is important to take immediate action on any concerns about harmful sexual behaviour to:
- prevent the behaviour from escalating
- keep everyone involved safe.
Usual child safeguarding procedures should be followed.
Independent Inquiry into Child Sexual Abuse (IICSA)
The Independent Inquiry into Child Sexual Abuse was a statutory inquiry for England and Wales, established in 2015. The inquiry looked at the extent to which State and non-State institutions failed in their duty of care to protect children from sexual abuse and exploitation and makes recommendations for reform. It published 19 reports on 15 investigations covering a wide range of institutions.
The Truth Project gave victims and survivors an opportunity to share their experiences with the Inquiry and put forward suggestions for change. More than 6,000 people took part in the Truth Project.
Some of the key findings from IICSA can be found in the presentaion below.
Additional resources
- STOPCE has an extensive list of the warning signs of child exploitation Spotting the Signs tool.
- Brook and BASHH (British Association for Sexual Health and HIV) updated their Spotting the Signs tool in 2023. The tool supports professionals to identify and respond to Child Sexual Exploitation (CSE) and Child Criminal Exploitation (CCE).
- This is a useful and informative video (15 mins) on spotting the signs of child sexual exploitation produced by Health Education England.
- NSPCC. Protecting children from sexual exploitation. Updated 2024.
- RCPCH. Safeguarding guidance for children and young people under 18 accessing early medical abortion services.
Child trafficking and modern slavery
Child trafficking is child abuse and is a form of modern slavery. It’s defined as recruiting, moving, receiving and harbouring children for the purpose of exploitation. Many children are trafficked into the UK from overseas, but children can also be trafficked from one part of the UK to another. Children make up almost a third of all human trafficking victims worldwide. Refugee, migrant and displaced children are especially vulnerable to trafficking. Whether they are escaping war and violence or in search of opportunities, many children lack pathways to move regularly and safely. Children are particularly vulnerable to trafficking if they come from an area where there is poverty, war, low education levels, discrimination or persecution, political conflict and economic uncertainty.
Children are trafficked for:
- child sexual exploitation
- criminal activity, including:
- cannabis cultivation
- street crime - such as pickpocketing, begging and bag theft
- moving drugs
- benefit fraud
- immigration fraud
- selling pirated goods, such as DVDs
- forced marriage
- domestic servitude, including:
- cleaning
- childcare
- cooking
- forced labour, including working in:
- restaurants
- nail bars
- factories
- agriculture
- illegal adoption
- unreported private fostering arrangements (for any exploitative purpose).
This list is not exhaustive and children who are trafficked are often exploited in more than one way. Being trafficked is abuse in itself but children who are trafficked may experience multiple other forms of abuse such as sexual abuse and exploitation, physical abuse, emotional abuse and neglect. Child trafficking can have a devastating and lasting impact on its victims.
Signs of child trafficking
They might:
- spend a lot of time doing household chores
- rarely leave their house or have no time for playing
- be orphaned or living apart from their family
- live in low-standard accommodation
- be unsure which country, city or town they're in
- can't or are reluctant to share personal information or where they live
- not be registered with a school or a GP practice
- have no access to their parents or guardians
- be seen in inappropriate places like brothels or factories
- have money or things you wouldn't expect them to
- have injuries from workplace accidents
- give a prepared story which is very similar to stories given by other children.
Impact of child trafficking
- Poor health and illness, which may be left untreated.
- Limited or no access to education.
- Physical and mental exhaustion.
- Emotional challenges which can lead to:
- feeling isolated and lonely
- disturbed sleep patterns
- depression and/or anxiety
- headaches
- panic attacks
- eating difficulties
- self-harm and suicidal thoughts
- drug and alcohol use as a means to escape from problems
- post-traumatic stress disorder (PTSD).
Child trafficking requires a child protection response and usual safeguarding procedures should be followed.
References
- NSPCC. Child trafficking. 2024.
- NSPCC. Protecting children from trafficking and modern slavery. Updated 2024.
- UNICEF. Article: Children make up almost one-third of all human trafficking victims worldwide. 2018.
- HM Government. Safeguarding children who may have been trafficked. Practice guidance. 2011.
Female genital mutilation (FGM)
Female genital mutilation (FGM) is a procedure where the female genitals are deliberately cut, injured or changed, but there's no medical reason for this to be done. It includes procedures where the genitalia are altered without skin removal including labial elongation, and scarification. It's also known as female circumcision or cutting, and by other terms, such as Sunna, gudniin, halalays, tahur, megrez and khitan, among others.
FGM is usually carried out on young girls between infancy and the age of 15, most commonly before puberty starts.
FGM has no health benefits for girls and women and can cause severe bleeding and problems urinating, menstrual difficulties and later cysts, infections, as well as complications in childbirth and increased risk of newborn deaths.
The practice of FGM is recognised internationally as a violation of the human rights of girls and women. It is illegal in the UK and is child abuse.
It's very painful and can seriously harm the health of women and girls. There are no health benefits from FGM but many documented harms.
It can also cause long-term problems with sex, childbirth and mental health.
Types of FGM
There are four main types of FGM:
- Type 1 (clitoridectomy) – removing part or all of the clitoris.
- Type 2 (excision) – removing part or all of the clitoris and the labia minora, with or without removal of the labia majora.
- Type 3 (infibulation) – narrowing the vaginal opening by creating a seal, formed by cutting and repositioning the labia.
- Other harmful procedures to the female genitals, including pricking, piercing, cutting, scraping or burning the area and labial elongation.
FGM is often performed by traditional circumcisers or cutters who do not have any medical training. But in some countries, it may be done by a medical professional. The National FGM Centre has an interactive map which contains prevalence rates and research in different countries as well as school holidays and term times in various countries.
Anaesthetics and antiseptics are not generally used, and FGM can be carried out using knives, scissors, scalpels, pieces of glass or razor blades.
FGM often happens against a girl's will without her consent, and girls may have to be forcibly restrained.
FGM has no health benefits, and it harms girls and women in many ways. It involves removing and damaging healthy and normal female genital tissue, and it interferes with the natural functions of girls' and women's bodies. Although all forms of FGM are associated with increased risk of health complications, the risk is greater with more severe forms of FGM.
Immediate complications of FGM can include:
- severe pain
- excessive bleeding (haemorrhage)
- genital tissue swelling
- fever
- infections e.g., tetanus
- urinary problems
- wound healing problems
- injury to surrounding genital tissue
- shock
- death.
Long-term complications can include:
- urinary problems (painful urination, urinary tract infections)
- vaginal problems (discharge, itching, bacterial vaginosis and other infections)
- menstrual problems (painful menstruations, difficulty in passing menstrual blood, etc.)
- scar tissue and keloid
- sexual problems (pain during intercourse, decreased satisfaction)
- increased risk of childbirth complications (difficult delivery, excessive bleeding, caesarean section, need to resuscitate the baby) and newborn deaths
- need for later surgeries, for example, the sealing or narrowing of the vaginal opening (type 3) may lead to the practice of cutting open the sealed vagina later to allow for sexual intercourse and childbirth (deinfibulation). Sometimes genital tissue is stitched again several times, including after childbirth, hence the woman goes through repeated opening and closing procedures, further increasing both immediate and long-term risks
- psychological problems (depression, anxiety, post-traumatic stress disorder, low self-esteem).
Why is FGM performed?
The reasons vary from one region to another as well as over time and include a mixture of sociocultural factors within families and communities. Some of the reasons include:
- Where FGM is a social convention (social norm), the social pressure to conform to what others do and have been doing, as well as the need to be accepted socially and the fear of being rejected by the community, are strong motivations to perpetuate the practice.
- FGM is often considered a necessary part of raising a girl, and a way to prepare her for adulthood and marriage. This can include controlling her sexuality to promote premarital virginity and marital fidelity.
- Some people believe that the practice has religious support, although no religious scripts prescribe the practice. Religious leaders take varying positions with regard to FGM, with some contributing to its abandonment.
What does the law say about FGM?
FGM is illegal in the UK. It is illegal to carry out FGM in the UK. It is also a criminal offence for UK nationals or permanent UK residents to perform FGM overseas or take their child abroad to have FGM carried out. The maximum penalty for FGM is 14 years imprisonment. There is also an offence of failing to protect a child from FGM.
Possible signs that a girl could be at risk of FGM
These are only possible indicators and by no means indicate that a girl will definitely go on to have FGM or that there is any intention for a girl to have FGM. Practitioners should be culturally aware and approach conversations about FGM sensitively and in a non-judgemental manner. Attitudes around the world are changing towards FGM with the United Nations reporting that two-thirds of people in FGM practising countries in Africa and the Middle East are opposed to FGM, for example.
These possible indicators can be an opportunity for conversation and discussion with families.
- A girl is born to a woman who has undergone FGM.
- Mother has requested re-infibulation following childbirth.
- A girl has an older sibling or cousin who has undergone FGM.
- One or both parents or elder family members consider FGM integral to their cultural or religious identity.
- The family indicate that there are strong levels of influence held by pro-FGM elders who are involved in bringing up female children.
- A girl/family has limited level of integration within UK community.
- If a girl from a practising community is withdrawn from PSHE and/or sex and relationship education or its equivalent, she may be at risk as a result of her parents wishing to keep her uninformed about her body, FGM and her rights.
- If there are references to FGM in conversation, for example a girl may tell other children about it.
- A girl may confide that she is to have a ‘special procedure’ or to attend a special occasion to ‘become a woman’.
- A girl may request help from a teacher or another adult if she is aware or suspects that she is at immediate risk.
- Parents state that they or a relative will take the child out of the country for a prolonged period and are evasive about why.
- A girl is taken abroad to a country with high prevalence of FGM, especially during the summer holidays which is known as the ‘cutting season’.
Possible signs that a girl may have had FGM
As with the possible signs above, the signs below are only possible indicators of FGM but are not proof. These signs can also be indicative of other health needs or other types of abuse such as child sexual abuse for example. Their presence provides an opportunity for conversation and discussion with families.
- Prolonged absence from schools.
- Frequent need to go to the toilet.
- Long break to urinate.
- Urinary tract infections.
- Noticeable behaviour change.
- Talk of something somebody did to them that they are not allowed to talk about.
- Change of dress from tight to loose-fitting clothing.
- Menstrual problems.
- Difficulty in sitting down comfortably.
- Complain about pain between their legs.
Mandatory reporting of FGM
In England and Wales, regulated health and social care professionals and teachers have a mandatory duty to make a report to the police if:
- they are informed directly by a child under the age of 18 that they have undergone FGM
- they observe physical signs that an act of FGM may have been carried out on a child under the age of 18.
Mandatory reporting is only one part of safeguarding children and young people against FGM and other abuse – other safeguarding procedures still need to be followed and all their clinical needs should be met.
It is important to note that you do not need to examine a child to confirm FGM if you are told. This type of examination is highly specialist and there is significant normal variability of genital anatomy. There is also the potential for re-traumatisation.
If a parent/guardian discloses that the child has had FGM, or you consider the girl to be at risk of FGM, follow local safeguarding procedures.
If the patient is over 18:
- The duty does not apply in this case. You should signpost the woman to services offering support and advice. You may also need to carry out a safeguarding risk assessment considering children who may be at risk or have had FGM.
In Wales, there is The All Wales Female Genital Mutilation Clinical Pathway which should be completed every time a new case of FGM is identified or suspected.
Talking about FGM
Talking about FGM - GPs leaflet provides tips for better, safe, and more effective woman centred conversations about FGM in general practice. It was developed for GPs with input and advice from people with lived experience. There is also an easy read leaflet on FGM.
References
- World Health Organization. Fact Sheets. Female genital mutilation. 2024.
- NHS. Female genital mutilation. 2022.
- National FGM Centre. Female Genital Mutilation.
- NSPCC. Protecting children from female genital mutilation (FGM). 2021.
- Home Office. Mandatory Reporting of Female Genital Mutilation – procedural information. 2020.
Child abuse linked to faith or belief
Certain kinds of child abuse are linked to faith or belief. Child abuse linked to faith or belief is not confined to one faith, nationality, ethnic group or community. Cases have been recorded worldwide across various religions including Christian, Muslim, Hindu and pagan faiths among others. Not all with the belief go on to harm children. The number of known cases suggests that only a small minority of people who believe in witchcraft or spirit possession go on to abuse children. Under-reporting of abuse is, however, likely.
Abuse may happen anywhere, but it most commonly occurs within the child’s home.
Child abuse linked to faith or belief includes belief in concepts of:
- witchcraft and spirit possession, demons or the devil acting through children or leading them astray (traditionally seen in some Christian beliefs)
- the evil eye or djinns (traditionally known in some Islamic faith contexts) and dakini (in the Hindu context)
- ritual or muti murders where the killing of children is believed to bring supernatural benefits or the use of their body parts is believed to produce potent magical remedies
- use of belief in magic or witchcraft to create fear in children to make them more compliant when they are being trafficked for domestic slavery or sexual exploitation.
This is not an exhaustive list and there will be other examples where children have been harmed when adults think that their actions have brought bad fortune, such as telephoning a wrong number which is believed by some to allow malevolent spirits to enter the home.
Common features
- Wider social or community consensus that witchcraft, for example, actually exists.
- Sometimes a faith leader or other influential figure is at the centre, promoting the belief and methods of resolving the supposed problem by harming children.
- Parents or carers have also been key perpetrators in many of the known cases. This can make the abuse harder to find out about, harder to get evidence to prosecute and harder to prevent in future.
- Perpetrators may believe they are saving the child as they believe the child is the victim of a supernatural force. There may also be the belief that the child can harm others which can generate a real fear in those who would normally be expected to protect the child, including parents or close family. This fear that a child may cause harm to, or kill, siblings, parents and other family or friends can be a critical factor in the abuse.
- Children may be scapegoated to reconcile misfortune that has occurred to the family or community, such as an adult family member becoming unemployed or being in poverty. In these situations, those who are different because they have some special traits (such as being particularly bright, having difficult behaviour, having a disability or children living away from their parents) are the target of scapegoating, being accused of having caused the misfortune by supernatural means. The most vulnerable people within a group offer the least ability to resist being scapegoated, and children are a group who are inherently vulnerable, needing protection from adults around them.
Common factors and causes
A range of factors can contribute to the abuse of a child for reasons of faith or belief. Some of the most common ones are below.
- Belief in evil spirits: belief in evil spirits that can ‘possess’ children is often accompanied by a belief that a possessed child can ‘infect’ others with the condition. This could be through contact with shared food, or simply being in the presence of the child.
- Scapegoating: a child could be singled out as the cause of misfortune within the home, such as financial difficulties, divorce, infidelity, illness or death.
- Bad behaviour: sometimes bad or abnormal behaviour is attributed to spiritual forces. Examples include a child being disobedient, rebellious, overly independent, wetting the bed, having nightmares or falling ill.
- Physical and emotional differences: a child could be singled out for having a physical difference or disability. Documented cases included children with learning disabilities, mental health issues, epilepsy, autism, stammers, deafness and LGBTQ+.
- Gifts and uncommon characteristics: if a child has a particular skill or talent, this can sometimes be rationalised as the result of possession or witchcraft. This can also be the case if the child is from a multiple or difficult pregnancy.
- Complex family structure: research suggests that a child living with extended family, non-biological parents, or foster parents is more at risk. In these situations they are more likely to have been subject to trafficking and made to work in servitude.
Child abuse linked to faith or belief can include physical abuse, emotional abuse, neglect, and sexual abuse.
- Physical abuse: this can involve beating, burning, cutting, stabbing, semi-strangulating, tying up the child, or rubbing chilli peppers or other substances on the child’s genitals or eyes.
- Emotional abuse: emotional abuse can occur in the form of isolation. A child may not be allowed near or to share a room with family members, and threatened with abandonment. The child may also be persuaded that they are possessed. The act of telling a child that they are possessed by an evil spirit or told that they are a witch can be emotionally abusive.
- Neglect: in situations of neglect, the child’s family and community may have failed to ensure appropriate medical care, supervision, education, good hygiene, nourishment, clothing or warmth.
- Sexual abuse: children who have been singled out in this way can be particularly vulnerable to sexual abusers within the family, community or faith organisation. These people exploit the belief as a form of control or threat. Children could also be subject to practices through the deliverance process that are sexually abusive e.g. having to be bathed undress in the presence of others. Trafficked children from some countries have been known to be subjected to practices designed to control them. Some of these practices involve using their pubic hair and undergarments in rituals.
Children who may be more at risk of child abuse linked to faith or belief:
- Children with disability including autism, epilepsy, down’s syndrome, dyslexia etc.
- Children with albinism.
- Children living away from home in private fostering situations or in domestic servitude situations.
- Children living with a stepparent, with one of the natural parents absent or dead.
- Children whose parents have been branded as witches.
- Children who are seen as ‘naughty’ or have challenging behaviour.
- Precocious children and left handed children.
- Children who are living within complex family structures e.g. a polygamous setting or reconstituted family.
What to look out for
Indicators of child abuse linked to faith or belief include the following and can be similar to other types of abuse:
- Physical injuries, such as bruises or burns (including historical injuries/scaring).
- A child reporting that they are or have been accused of being ‘evil’, and/or that they are having the ‘devil beaten out of them’.
- The child or family may use words such as ‘kindoki’, ‘djin’, ‘juju’ or ‘voodoo’ - all of which refer to spiritual beliefs.
- A child becoming noticeably confused, withdrawn, disorientated or isolated and appearing alone amongst other children.
- A child’s personal care deteriorating (eg rapid loss of weight, being hungry, turning up to school without food or lunch money, being unkempt with dirty clothes).
- It may be directly evident that the child’s parent does not show concern for or a close bond with them.
- A child’s attendance at school or college becomes irregular or there is a deterioration in a child’s performance.
- A child is taken out of a school altogether without another school place having been arranged.
- Wearing unusual jewellery/items or in possession of strange ornaments/scripts.
Response to child abuse linked to faith or belief
As with all types of child abuse, the response to concerns about tackling this type of abuse should be focused on keeping the child safe and bringing the perpetrators to justice. The response must also involve engagement with those individuals, families and in some cases faith or other communities whose belief underlies the harm.
It is not about challenging people’s beliefs, but where beliefs lead to abuse that must not be tolerated.
Usual safeguarding procedures should be followed when abuse or neglect is suspected, ensuring you mention you are concerned the child may be a victim of abuse linked to faith and abuse and the reasons why you are concerned.
The National FGM Centre has further helpful advice on responding to concerns about child abuse linked to faith or belief.
References
- National FGM Centre. Child Abuse Linked to Faith or Belief.
- Department for Education. National action plan to tackle child abuse linked to faith or belief. 2012.
- Metropolitan Police. Child abuse linked to faith or belief. 2024.
- Department for Education. National action plan to tackle child abuse linked to faith or belief: executive summary. 2012.
Bullying and cyberbullying
Bullying is intentional behaviour that hurts someone else. It includes name calling, hitting, pushing, spreading rumours, threatening or undermining someone.
It can happen anywhere – at school, at home or online. It's usually repeated over a long period of time and can hurt a child both physically and emotionally.
Cyberbullying is bullying that takes place online. Unlike bullying offline, online bullying can follow the child wherever they go, via social networks, gaming and mobile phone. A person can be bullied online and offline at the same time.
Cyberbullying can include:
- sending threatening or abusive text messages
- creating and sharing embarrassing images or videos
- trolling – the sending of menacing or upsetting messages on social networks, chat rooms or online games
- excluding children from online games, activities or friendship groups
- shaming someone online
- setting up hate sites or groups about a particular child
- encouraging young people to self-harm
- voting for or against someone in an abusive poll
- creating fake accounts, hijacking or stealing online identities to embarrass a young person or cause trouble using their name
- sending explicit messages, also known as sexting
- pressuring children into sending sexual images or engaging in sexual conversations.
Signs of bullying can include:
- belongings getting 'lost' or damaged
- physical injuries, such as unexplained bruises
- being afraid to go to school, being mysteriously 'ill' each morning, or skipping school
- a change in how they are doing at school, including a dip in grades or not handing homework in
- asking for, or stealing, money (to give to whoever's bullying them)
- a change in behaviour, including being nervous, losing confidence, or becoming distressed and withdrawn
- a change in eating or sleeping habits
- bullying others.
The effects of bullying can last into adulthood and can drive children and young people to self-harm and suicide. They may develop mental health problems, have fewer friends, and have problems adjusting to school. Any child can be bullied for any reason.
Childline has lots of information and support for children and young people who are experiencing bullying.
References
- NSPCC. Bullying and cyberbullying. 2024.
- Childline. Bullying, abuse, safety and the law.
Part 2B: Topics covering both child and adult issues
Part 2B is applicable to both children and adults:
- Radicalisation.
- Domestic abuse.
- Transitional safeguarding.
Radicalisation (covers child and adult)
Radicalisation is a process by which an individual or group adopts increasingly extreme political, social, or religious ideals and aspirations that reject or undermine the status quo or undermine contemporary ideas and expressions of freedom of choice. Radicalisation is comparable to other forms of exploitation. It is a safeguarding issue that staff working in the health sector must be aware of.
Healthcare staff will meet and treat people who may be vulnerable to being drawn into terrorism, and all staff have a responsibility to safeguard vulnerable individuals of all ages that they come into contact with. Preventing radicalisation sits alongside long-established duties on professionals to safeguard vulnerable children, young people and adults from exploitation from a range of other harms such as drugs, gangs and physical and sexual exploitation.
If any member of staff in general practice has any concerns about a patient or colleague being radicalised they should follow their local safeguarding pathways.
Vulnerability factors to radicalisation:
They can apply to any age, social class, religion, ethnic or educational background.
- Struggling with a sense of identity.
- Distanced from their cultural or religious background.
- Difficulty fitting in with British culture.
- Questioning their place in society.
- Family issues.
- Experiencing a traumatic event.
- Experiencing racism or discrimination.
- Difficulty in interacting socially, lacking empathy, or not understanding the consequences of their actions.
- Low self-esteem.
More important than any one specific sign is the sense that something is not quite right with the person you’re worried about.
Potential signs of radicalisation:
- Being influenced or controlled by a group.
- An obsessive or angry desire for change or ‘something to be done’.
- Spending an increasing amount of time online and sharing extreme views on social media.
- Personal crisis.
- Mental health issues.
- Need for identity, meaning and belonging.
- Looking to blame others.
- Desire for status, need to dominate.
Some key indicators of radicalisation to watch out for in children:
- They are becoming increasingly isolated from family and friends.
- They are talking as if from a script.
- They are unwilling to engage about their views.
- They are becoming intolerant of other people’s views.
- They are becoming increasingly angry about issues of events they feel are unfair or unjust.
- They are secretive about who they are meeting online or in person.
Prevent
Prevent is part of the government counter-terrorism strategy CONTEST and aims to reduce the threat to the UK from terrorism by stopping people becoming terrorists or supporting terrorism. The key pillars of CONTEST are:
- Prevent: to stop people becoming terrorists or supporting terrorism.
- Pursue: to stop terrorist attacks.
- Protect: to strengthen our protection against a terrorist attack.
- Prepare: to mitigate the impact of a terrorist attack.
The objectives of Prevent are to:
- tackle the causes of radicalisation and respond to the ideological challenge of terrorism
- identify, safeguard and support those most at risk of radicalisation through early identification, intervention and support
- enable those who have already engaged in terrorism to disengage and rehabilitate.
The Prevent duty
The Prevent duty requires specified authorities such as education, health, local authorities, police and criminal justice agencies (prisons and probation) to help prevent the risk of people becoming terrorists or supporting terrorism. It sits alongside long-established safeguarding duties on professionals to protect people from a range of other harms, such as substance abuse, involvement in gangs, and physical and sexual exploitation. The duty helps to ensure that people who are susceptible to radicalisation are supported as they would be under safeguarding processes.
There is Prevent duty guidance for specified authorities in England and Wales and separate guidance for Scotland. There is no specific Prevent guidance for Northern Ireland. The health specified authorities in England and Wales are:
- an NHS trust in England and Wales
- an NHS foundation trust
- a local health board in Wales
- the Board of Community Health Councils in Wales.
The health specified authorities in Scotland are:
- A health board
- A special health board
- Healthcare Improvement Scotland.
Whilst GP practices do not fall under the Prevent duty, they still have to carry out their safeguarding responsibilities and duties regarding radicalisation.
The Home Office provides an online Prevent awareness course which gives a helpful insight into Prevent.
Channel panel
If the Prevent referral progresses and it is assessed that there is a genuine risk of radicalisation, the case is considered by a multi-agency ‘Channel panel’ of professionals who collectively assess the case and decide on a tailored package of support that can be offered to the person.
The Channel panel is chaired by the local authority and can include a variety of partners such as the police, children’s services, social services, education professionals and mental health care professionals.
If a Channel intervention is required, a tailored support package will be offered. This could include mentoring, theological guidance, education, and careers assistance to those assessed as being at risk of radicalisation and requiring support.
Channel is voluntary and people who are referred to Prevent must give consent before they can be given support.
If a person does not engage with Channel or decides not to continue with the process for any reason, alternative forms of support may be available from the local authority or other providers. Any risks are then carefully managed by the police.
References
- ACT. Action Counters Terrorism.
- NSPCC. Radicalisation and child protection. 2024.
- Home Office. Revised Prevent duty guidance: for Scotland (2015). Updated 2024.
- Home Office. Prevent duty guidance: for England and Wales. 2024.
- Home Office. Prevent and Channel factsheet – 2023. 2023.
Domestic abuse (covers child and adult)
What is domestic abuse?
Domestic abuse can include physical, sexual, economic, psychological, emotional abuse, violent or threatening behaviour, controlling or coercive behaviour. It does not matter whether the behaviour consists of a single incident or a course of conduct. It can occur between those aged 16 years or over and who are personally connected. This includes: those who are, or who have previously been, partners, in an intimate relationship; relatives; and those who have had a child together.
It includes coercive control, which is an act or a pattern of acts of assault, threats, humiliation and intimidation or other abuse that is used to harm, punish, or frighten their victim. Domestic abuse can also include stalking and harassment as well as technology facilitated abuse.
Domestic abuse is very common but is largely a hidden crime, occurring primarily at home.
It is very common – each year an estimated 2 million adults in England and Wales experience some form of domestic abuse but this is likely to be an underestimate as domestic abuse is under-reported.
GPs experience domestic abuse tooAsking about domestic abuse
Every victim and survivor of domestic abuse is on their own individual journey. Some may not recognise that they are victims of abuse, others may recognise it but not feel ready to talk about it or ask for help, others may fear the consequences of speaking out – both from their abuser but also from statutory services, for example, a fear of having their children removed from them. Some may have spoken out before and the abuse just got worse.
Asking and talking about domestic abuse should be done sensitively in a private environment. If an interpreter is needed, do not use friends, family or carers. There is no single ‘right way’ to ask about domestic abuse. The key is to be able to identify when there are signs of possible domestic abuse and then have professionally curious conversations. Each practitioner will find their own way of asking and talking about domestic abuse, keeping in mind that this will need to be adapted to each individual patient depending on communication needs and preferences.
These are some examples of questions you could use:
- Has anyone ever made you feel frightened? What do they do that scares you?
- Has anyone hurt you or threatened to?
- Does anyone at home make you feel scared?
- Do you feel safe at home/in your family/in your relationship?
- Are you ever forced to do anything you are not comfortable with?
Responding to disclosures of domestic abuse
DO:- Listen, be non-judgmental.
- Thank them for telling you, acknowledge how difficult this must be for them.
- Ask what you can do to help.
- Signpost to agencies who can help, e.g. local domestic abuse agencies, police, National Domestic Abuse Helpline (freephone number 0808 2000 247 which is run 24 hours a day, 7 days a week). Domestic abuse agencies are the experts in supporting victims and survivors of abuse – knowing the contact details of your local agency and also what they do will help you to feel more confident in asking about domestic abuse and knowing how to help your patients.
- Consider what the current level of risk is, and respond appropriately.
- Minimise or dismiss the abuse.
- Tell them what to do.
- Ask ‘why don’t you just leave?’ – this is victim blaming. Leaving is also one of the highest risk times for victims.
Role of domestic abuse agencies
Domestic abuse agencies play a vital role in supporting victims and survivors of domestic abuse. They offer a wide range of services such as providing support in the community, helplines, refuges, independent advocacy, supporting children, and supporting victims through police, legal and court processes. They are the experts in all aspects of domestic abuse including safety planning and risk assessment.
MARAC
MARAC stands for ‘Multi-agency risk assessment conference’. A MARAC is a meeting where information is shared on the highest risk domestic abuse cases. MARACs operate across the four UK nations. MARACs are attended by representatives from police, health, child protection, housing, independent domestic violence advisors (IDVAs), probation and other specialists from the statutory or voluntary sectors.
They:- share all relevant information they have about a victim
- discuss options for increasing the victim’s safety
- create a co-ordinated action plan.
The primary focus of the MARAC is to safeguard the adult victim. The MARAC will also make links with others to safeguard children and manage the perpetrator’s behaviour.
At the heart of the MARAC is the working assumption that no single agency or individual can see the complete picture of a victim’s life but they all may have insights that are crucial to the victim’s safety. The victim doesn’t attend the meeting but they are represented by an IDVA who speaks on their behalf.
Referral and information sharing processes between general practice and their local MARACs vary across different areas.
More information about MARACs, including specific guidance for each UK nation, can be found on SafeLives.
Documentation of domestic abuse in the medical record
- Documentation of domestic abuse is very important. Use the patient’s exact words when recording what they have said. Where there is patient online access, make sure all entries about domestic abuse are marked not for online access.
- The RCGP has specific guidance on documenting domestic abuse in different scenarios, including whether to record information in perpetrator records.
Identifying, understanding and responding to different levels of risk in domestic abuse including safeguarding considerations
GPs and general practice staff are not expected to be experts in domestic abuse or in carrying out domestic abuse risk assessments. However, as with any other condition or situation that potentially can cause serious harm or a risk to life, in general practice we need to be able to identify, understand and appropriately respond to different levels of risk in a domestic abuse situation. It is important to keep in mind that risk can be dynamic and fluctuate over time. In addition, the understanding the level of risk in a situation can change over time when additional information becomes available. Our response therefore needs to be flexible and adapt to changing risk.
The table below provides general principles for practitioners to help them identify, understand and respond safely to different levels of risk that might present in a domestic abuse situation.
- The person does not feel safe right now and/or they do not feel safe to go home or stay at home. In this situation, ascertain:
- Where is the alleged perpetrator?
- If there are children, where are they?
- The person has expressed fear of immediate serious harm:
- “I think he/she is going to kill me/the children.”
- In addition, there is a history of previous high risk domestic abuse, e.g. previous MARAC.
- The person is planning to leave the relationship/situation. This can be a particularly dangerous time. Women’s Aid has advice for victims wanting to leave a relationship safely.
- Support the victim to contact police on 999 or call on the victim’s behalf if they are not able to.
- Share the 999 silent solution. If someone needs the police but cannot speak, they can call 999, a recorded message will instruct callers who can’t talk to press 55 to be put through to police.
- If the patient is in the practice – find a safe place for them to stay whilst waiting for the police.
- If the patient is at home/elsewhere – is there a safe place they can go?
- If children are at school/nursery –
- contact the school/nursery to keep the children in a safe place.
- Make an immediate safeguarding referral to children’s social care by phone, followed up with a written referral.
- If the patient is an adult with care and support needs, consider adult safeguarding referral in addition to the above steps.
- Consider a referral to MARAC – seek advice if unsure.
- Arrange appropriate follow up.
- severe abuse
- escalation in frequency/severity of abuse
- use of weapons
- stalking
- sexual assault
- attempted suffocation/strangulation/drowning
- high levels of jealousy/coercive control
- pregnancy
- perpetrator behaviour:
- threats to kill the victim or others
- threats to hurt children (including unborn children)
- threats of suicide
- access to weapons
- use of alcohol/drugs
- abuse of family pet
- history of assaults
- previous/current known high risk domestic abuse including being known to MARAC
- your own professional judgement.
- Assess immediate safety.
- Give basic safety advice such as contacting the police on 999 if they are concerned their life is in danger. Share the 999 silent solution.
- Refer to the local domestic abuse agency.
- Consider a MARAC referral – seek advice if unsure.
- Make a child safeguarding referral if there are children (including unborn) in the household/situation.
- Consider an adult safeguarding referral if the adult has care and support needs.
- Arrange appropriate follow up.
- type and severity of abuse
- what the patient wants support with
- whether there are children in the household/situation
- whether the adult has care and support needs or there are adults with care and support needs in the household/situation.
- Signpost/refer to local domestic abuse agency.
- If there are children in the family/situation, consider a child safeguarding referral or an Early Help referral (dependent on the situation) to further assess the family situation and provide support.
- Consider an adult safeguarding referral if there are adults with care and support needs in the household/situation.
- Arrange appropriate follow up.
- In all cases, provide ongoing support.
- Always be mindful that you may only know about a small part of the situation. Keep an open mind regarding risk and reassess as necessary.
- Domestic abuse agencies are the agency best placed and trained to support victims of domestic abuse and their families and to carry out risk assessments. Victims of domestic abuse should always be signposted/referred to a domestic abuse agency.
- Be clear that you understand when consent is, and is not needed, for referrals to other agencies for risk assessment and support in domestic abuse situations. For further guidance refer to:
- GMC guidance: Confidentiality: Disclosures for the protection of patients and others.
- SafeLives. Multi-Agency Risk Assessment Conference (Marac) Guidance for GPs.
- Seek advice at any time when you are not sure how to proceed.
- Advice can be sought from:
- practice/organisational safeguarding lead
- safeguarding professionals such as Named/Designated professionals, safeguarding leads within health boards/authorities
- local domestic abuse agency
- MARAC co-ordinators.
- Share information with relevant other professionals such as midwives and health visitors.
- Is the alleged perpetrator a person in a position of trust or someone who works with children or adults with care and support needs?
- Seek advice from safeguarding professionals on how to proceed.
A note on the DASH risk checklist
The SafeLives DASH (domestic abuse, stalking and honour-based violence) risk checklist is widely used by specialist domestic abuse workers to identify high risk cases of domestic abuse, stalking and ‘honour’ -based abuse. It is not expected or recommended for use in general practice as dedicated training, sufficient time and domestic abuse expertise are necessary to complete this with a victim/survivor.
Why is domestic abuse a health issue?
- 75% of domestic violence results in physical injury or mental health consequences to women.
- Domestic abuse is the leading cause of morbidity for women aged 19-44, greater than cancer, war and road traffic accidents.
- There is extensive contact between women and primary care clinicians with 90% of all female patients consulting their GP over a five-year period.
- 1 in 8 of all suicides and suicide attempts by women in the UK are due to domestic abuse.
- 80% of women in a violent relationship seek help from health services, usually GPs, at least once and this may be their first or only contact with professionals.
- 30% of domestic abuse starts/escalates during pregnancy.
- 1 in 4 women in contact with mental health services are likely to be experiencing domestic abuse.
- 51,355 NHS staff are likely to have experienced abuse in the past 12 months.
On average, victims will experience abuse for three years before getting effective help and will visit their GP on average 4.3 times. In England, children are now recognised in law as victims of domestic abuse in their own right if they see, hear or otherwise experience the effects of abuse.
Some victims may face additional barriers to help and disclosure such as those who are older, disabled, LGBTQ+, or from ethnic minorities.
Who are victims of domestic abuse?
Anyone can be a victim of domestic abuse, regardless of sex, gender reassignment, age, ethnicity, socio-economic status, sexuality, or background. It can occur within a wide range of relationships. In addition, domestic abuse can manifest itself in different ways within different communities.
While both men and women can be affected by domestic abuse, females are disproportionately the victims. The majority of domestic homicide victims are women.
Domestic abuse most commonly takes place in intimate partner relationships, including same sex relationships. Intimate relationships can take different forms, partners do not need to be married or in a civil partnership and abuse can occur between non-cohabiting intimate partners. As with all forms of abuse, abuse in intimate relationships can vary in severity and frequency, ranging from a one-off occurrence to a continued pattern of behaviour.
Abuse can continue or intensify when a relationship has ended or is in the process of ending. This can be a very dangerous time for a victim including an increased risk to their physical safety. It is a highly critical period for ensuring support for victims, as they may consider returning to perpetrators during the period immediately after fleeing or ending the relationship. Separation can raise both the likelihood and consequences of risk because of the perpetrator’s perceived lack of control.
Domestic abuse may also be perpetrated by a family member: by adult children, grandchildren, parents, those with “parental responsibility”, siblings, or extended families including in-laws. Abuse within a family set up can encompass a number of different harmful behaviours. Abuse may be perpetrated as a perceived means to protect or defend the ‘honour’ of an individual, family or community against alleged or perceived breaches of the family or community’s code of behaviour. It can therefore include ‘honour’-based abuse, forced marriage, female genital mutilation, and other harmful practices such as reproductive coercion (and as part of this, forced abortion).
Young people can experience domestic abuse within their relationships. Teenage relationship abuse often occurs outside of a domestic setting. Teenage victims may find it difficult to identify abusive behaviour, for instance, controlling or jealous behaviour may be misconstrued as love.
Teenage relationship abuse is not a term defined by the Domestic Abuse Act 2021. If the victim and perpetrator are at least 16 years old, abuse in their relationship can fall under the statutory definition of domestic abuse. Whilst young people under the age of 16 can experience abuse in a relationship, it would be considered child abuse. Abusive behaviours by one young person toward another, where each are aged between 16 and 18 could be both child abuse and domestic abuse as a matter of law. Ultimately, in responding to cases of abuse involving those under 18, child safeguarding procedures should be followed.
Domestic abuse in teenage relationships can be just as severe and has the potential to be as life threatening as abuse in adult relationships.
Child victims of domestic abuse
Domestic abuse always has an impact on children. Being exposed to domestic abuse in childhood is child abuse. Children and young people may experience domestic abuse both directly and indirectly. Young people aged 16 or over can also experience domestic abuse in their own relationships.
Domestic abuse undermines a child's basic need for safety and security. It can have a serious effect on their behaviour, brain development, education outcomes and overall wellbeing.
Children and young people may experience:
- not getting the care and support they need from their parents or carers as a result of the abuse
- hearing the abuse from another room
- seeing someone they care about being injured and/or distressed
- finding damage to their home environment like broken furniture
- being hurt from being caught up in or trying to stop the abuse
- being denied access to parts of their home, such as rooms being locked
- being forced out of or losing their home.
The impact of domestic abuse on children and young people can include:
- aggression and challenging behaviour
-
depression - anxiety - including worrying about a parent’s or carer's safety
- changes in mood
- difficulty interacting with others
- withdrawal
- fearfulness, including fear of conflict
- suicidal thoughts or feelings
- not having a strong bond with their parents or carers
- hoping an abused parent will leave for safety reasons
- worrying about what might happen if their parents or carers separate
- being afraid of their parents or carers
- impact on executive functioning skills and brain architecture which can lead to overactive stress responses.
These impacts may present in general practice with problems such as:
- problems with school or with learning
- eating disorder
- anxiety and depression including separation anxiety
- alcohol and drug misuse
- nightmares or insomnia
- bedwetting
- tantrums
- antisocial behaviour
- aggression or bullying
- social withdrawal
- constant, regular sickness.
How might I know my adult patient might be experiencing domestic abuse?
There are some physical and mental health issues which have a strong link to being a victim or survivor of domestic abuse. Adult victims may present with:
- anxiety
- depression
- PTSD
- chronic pain
- difficulty sleeping
- facial or dental injuries
- alcohol/drug misuse
- chronic pain or fatigue
- pregnancy and miscarriage
- unexpected injuries, for example to breasts or abdomen
- genital injuries
- sexually transmitted infections
- urinary tract infections
- unprotected sex
- nipple lesions
- requests for a termination.
When patients, adults or children, present with any of the problems we have just identified, we should ask about domestic abuse. We also need to bear in mind that these problems can also be indicative of many different forms of abuse and neglect.
Coercive control
“Coercive control is an act or pattern of acts of assault, threats, humiliation and intimidation or other abuse that is used to harm, punish, or frighten their victim. This controlling behaviour is designed to make a person dependent by isolating them from support, exploiting them, depriving them of independence and regulating their everyday behaviour". Women's Aid.
Coercive control is a criminal offence.
Some examples of coercive behaviour are:
- isolation from friends and family
- deprivation of basic needs, such as food
- monitoring how time is spent
- monitoring via online communication tools or spyware
- threatening to publish or share private information
- taking control over aspects of everyday life, such as where someone can go, who they can see, what they can wear and when they can sleep
- depriving access to support services, such as medical services
- preventing access to transport or work
- repeatedly putting someone down, such as saying they are worthless
- humiliating, degrading or dehumanising someone
- controlling finances
- making threats to hurt or kill someone, including their children or other family members
- sexual assault.
Honour-based abuse
Honour-based abuse is a crime or incident committed to protect or defend the 'honour' of a family or community.
If a family or community think someone has shamed or embarrassed them by behaving in a certain way, they may punish that person for breaking their 'honour code’.
People who carry out honour-based abuse are often close family members but also extended family or community members.
There isn't one specific crime of honour-based abuse. It can involve a range of crimes and behaviours, such as:
- forced marriage
- domestic abuse (physical, sexual, psychological, emotional or financial)
- sexual harassment and sexual violence (rape and sexual assault or the threat of)
- threats to kill, physical and emotional violence and murder
- pressure to go or move abroad
- being kept at home with no freedom
- not allowed to use the telephone, internet, or have access to important documents like your passport or birth certificate
- isolation from friends and members of your own family.
Support for victims of honour-based abuse
- Victim Support
- Southhall Black Sisters. Highlights and challenges violence against black (Asian and African-Caribbean) women. They offer a range of services.
- IKWRO. A charity providing advice and support in Arabic, Kurdish, Turkish, Dari and Farsi to women, girls and couples living in Britain, in particular helping women facing domestic violence, forced marriage and honour-based violence.
- Karma Nirvana. Provides support and advice on protecting yourself if you are experiencing forced marriage or honour-based violence.
Forced marriage
A forced marriage is where one or both people do not or cannot consent to the marriage and pressure or abuse is used to force them into marriage. It is also when anything is done to make someone marry before they turn 18. It is a harmful practice that disproportionately affects women and girls globally, preventing them from living their lives free from all forms of violence. Forced marriage cannot be justified on either religious or cultural grounds, every major faith condemns it and freely given consent is a prerequisite of marriage for every religion.
A forced marriage is not the same as an arranged marriage. In an arranged marriage the families take a leading role in choosing the marriage partner, but the marriage is entered into freely by both parties.
Forced marriage is illegal in the UK. It is a form of domestic abuse and a serious abuse of human rights and for those under 18, child abuse.
In the majority of cases of forced marriage, the marriage takes place abroad. Forced marriage is a global issue that affects many different cultures and nationalities.
The pressure put on people to marry against their will may be physical, emotional, psychological or financial.
Child marriage is any marriage where at least one of the parties is under 18 years of age. Child marriage is considered to be a form of forced marriage. Child marriage is also often accompanied by early and frequent pregnancy and childbirth, resulting in higher than average maternal morbidity and mortality rates.
The Forced Marriage Unit (FMU) is a joint Foreign, Commonwealth and Development Office (FCDO) and Home Office unit which leads on the government’s forced marriage policy, outreach and casework. It operates both inside the UK (where support is provided to any individual) and overseas (where consular assistance is provided to British nationals, including dual nationals). The FMU operates a public helpline for victims, potential victims and professionals.
SafeLives has a useful practice briefing “Identifying and engaging with young people at risk of forced marriage ” which outlines warning signs, aggravating factors, best practice and safety planning.
Non-fatal strangulation
Strangulation is defined as asphyxia by closure of the blood vessels and/or air passages of the neck as a result of external pressure on the neck. There are three main categories: hanging, ligature strangulation and manual strangulation. Non-fatal strangulation (NFS) is where the patient has not died.
Non-fatal strangulation is common, especially in domestic and sexual abuse/rape and suicide attempts. NFS can have serious consequences such as carotid artery dissection, stroke and acquired brain injury.
A trauma informed approach is required and patients are unlikely to spontaneously give a history of strangulation. Intercollegiate guidance has been developed for clinical management of non-fatal strangulation.
Domestic abuse during pregnancy
Pregnancy is a particularly high-risk time for domestic abuse. For Baby’s Sake (an organisation who work with parents experiencing domestic abuse) highlights:
- 30% domestic abuse begins during pregnancy.
- 40-60 % of women experiencing domestic abuse are abused during pregnancy.
- 82% of health visitors reported an increase in domestic violence and abuse during Covid-19.
- 50,000 children aged 0 – 5, including 8300 babies under one, are living in households where all three of domestic abuse, alcohol or drug dependency and severe mental ill-health were present.
Exposure to domestic abuse in the first 1001 days of life is associated with adverse outcomes for babies and mothers:
- Potential antenatal and postnatal depression.
- Poor obstetric outcomes.
- Disrupted neurodevelopment.
- Poor mental and physical health.
- Lower academic achievement.
- Impaired social development and emotional regulation.
It is therefore vitally important that everyone in general practice is aware of this high-risk period and clinicians proactively ask about domestic abuse during this time so that families can receive the support and help they need.
Resources for parents
- The Baby Buddy app is for mums, dads and caregivers during pregnancy, birth and the baby’s first year. Safer Beginnings (a joint programme of work by Best Beginnings and the White Ribbon Alliance UK) content has been embedded into the Baby Buddy app on themes such as ‘safer care’ and ‘safer relationships’. The resources offer support, guidance and practical tools for parents and parents-to-be, particularly those who have experienced trauma or harm. Topics include self-advocacy in maternal care, emotional safety, stress responses, FGM/FGC, sexual abuse and domestic abuse.
Stalking
The four warning signs of stalking are:
- fixated
- obsessive
- unwanted
- repeated.
It is behaviour that makes the victim feel pestered and harassed. It includes behaviour that happens two or more times, directed at or towards the victim by another person, causing them to feel alarmed or distressed or to fear violence might be used against them.
Stalking can go on for a long time, making the victim feel constantly anxious and afraid. Cyber-stalking and online threats and harassment can be just as intimidating. Stalking is a crime in all four UK nations and must be taken seriously. Stalking is a warning marker for violent behaviour.
Stalking can happen to anyone. A stalker can be a current of former partner, an acquaintance, work colleague or a stranger. Professionals, including healthcare staff, can be stalked by clients/patients.
Stalking may include:
- regularly following someone
- repeatedly going uninvited to their home
- checking someone’s internet use, email or other electronic communication
- hanging around somewhere they know the person often visits
- interfering with their property
- watching or spying on someone
- identity theft (signing-up to services, buying things in someone's name).
Social networking sites, chat rooms, gaming sites and other forums are often used to stalk and harass someone, for example:
- to get personal information
- to communicate (calls, texts, emails, social media, creating fake accounts)
- damaging the reputation
- spamming and sending viruses
- tricking other internet users into harassing or threatening
- identity theft
- threats to share private information, photographs, copies of messages.
The National Stalking Helpline is a service set up to provide advice and advocacy to residents from across the United Kingdom.
Child to parent Abuse
Child-to-parent abuse is where a child displays harmful behaviours towards parents/caregivers. Child-to-parent abuse can involve children of all ages, including adult children, and abuse toward siblings, grandparents, aunts, uncles as well as other family members such as those acting as kinship carers. If the child is 16 years of age or over, the abuse falls under the statutory definition of domestic abuse in the 2021 Act.
There is currently no agreed definition for this type of harm of abuse. The harmful behaviour can be physical, verbal, economic, digital, coercive or sexual. Behaviours can encompass, but are not limited to, humiliating and belittling language, violence and threats, jealous and controlling behaviours, damage to property, stealing and heightened sexualised behaviours. Child-to-parent abuse appears gendered, with the majority of cases being perpetrated by sons against their mothers, although men and boys are victims too.
These situations are often complex, difficult to identify and talk about. Parents/caregivers will often feel ashamed, disappointed, humiliated and blame themselves for the situation meaning they are less likely to report the abuse to the police. There can also be an element of denial. It can cause parents to feel fearful and isolated and can have a profound and devastating impact on families. In addition, Parents may fear being blamed, disbelieved, or conversely having their child taken away from them or criminalised leaving them reluctant to seek help.
There are often no simple solutions to these situations. Victims should receive appropriate domestic abuse response and support. As part of any professional response, it is important that any child who displays harmful behaviour receives a safeguarding response and steps taken to understand the child’s behaviour.
Domestic homicide reviews
Domestic homicide reviews (DHRs) are done when the death of a person aged 16 or over has, or appears to have, resulted from violence, abuse or neglect by either:
- a relative
- a spouse, partner or ex-partner
- a member of the same household.
This includes deaths by suicide.
The purpose of a domestic homicide review is to:
- help identify lessons we can learn from the death
- prevent further domestic abuse
- improve services for victims of domestic abuse.
GPs and general practice may be asked to contribute to domestic homicide reviews when it involves one of their patients. The GMC in their guidance, ‘Confidentiality: good practice in handling patient information (paragraph 71)’, state:
“You must also consider seriously all requests for information needed for formal reviews (such as inquests and inquiries, serious or significant case reviews, case management reviews, and domestic homicide reviews) that are established to learn lessons and to improve systems and services.”
References
- For Baby’s Sake. Domestic abuse and baby’s first 1001 days. 2021.
- SafeLives. Pathfinder Profile: General Practitioners. Guidance for General Practitioners responding to domestic abuse.
- Women’s Aid. What is coercive control? 2024.
- Refuge. Coercive control. 2017.
- ManKind Initiative. Statistics on Male Victims of Domestic Abuse. 2024.
- Karma Nirvana. What is Honour Based Abuse? 2023.
- Metropolitan Police. What is honour-based abuse? 2024.
- Home Office. Guidance: Forced Marriage. Updated 2023.
- United Nations Human Rights. Office of the High Commissioner. Child and forced marriage, including in humanitarian settings.
- HM Government. Forced marriage factsheet and guidance.
- SafeLives. ‘Honour’-based violence and forced marriage spotlight.
- Institute for Addressing Strangulation. Guidelines for clinical management of non-fatal strangulation in acute and emergency care services. 2024.
- NSPCC. Protecting children from domestic abuse. 2024.
- Barnado's. Children affected by domestic abuse. 2024.
- Women's Aid. What isdomestic-abuse? 2024.
- SafeLives. Resources for identifying the risk victims face.
- SafeLives. Multi-Agency Risk Assessment Conference (Marac) Guidance for GPs.
- GMC. Confidentiality: good practice in handling patient information. 2024.
- Best Beginnings. Safeguard Beginnings content to enable, educate and support people on maternity journeys.
- Best Beginnings. The Baby Buddy App.
- Victim Support. Stalking.
- Metropolitan Police. What is stalking and harassment. 2024.
- Suzy Lamplugh Trust. National Stalking Helpline. 2019.
- SafeLives. Responding to Counter allegations: Guidance – A review of practice. 2023.
- Home Office. Consultation: Defining child to parent abuse. Consultation description. 2023.
- Home Office. Domestic Abuse. Statutory Guidance. 2022.
- Respect. Child and Adolescent to Parent Violence and Abuse.
- PEGS (Parental Educational Growth Support). Child to Parent Abuse: Supporting parents and professionals. 2021.
- Home Office. Domestic Homicide Review Library. 2023.
The RCGP would like to thank Professor Gene Feder (Professor of primary health care, Bristol Medical School, University of Bristol) and Medina Johnson (CEO, IRISi) for their invaluable input into the development of this section on domestic abuse.
Summary of RCGP domestic abuse resources
GPs experience domestic abuse too
Research suggests that healthcare professionals may be more likely to experience domestic abuse than people in the general population. Recognising that GPs can also experience domestic abuse will help general practice play its part in working together with other agencies to improve safety, reduce mental health and financial harms caused by domestic abuse and improve support around work.
- The GPs experience domestic abuse too resource highlights the specific support-seeking barriers faced by GPs who are experiencing domestic abuse, how GP victim-survivors can be heard and supported by colleagues and employers and signposts to sources of support.
Knowledge and competencies
- Knowledge and competencies around domestic abuse and all aspects of child and adult safeguarding are expected for all GPs and general practice staff. These can be found in the RCGP safeguarding standards for general practice.
- Staff requiring level 3 safeguarding training have specific domestic abuse knowledge and competencies, as do practice managers – all can be found in the safeguarding standards.
Guidance on identifying and responding to domestic abuse
- The RCGP Safeguarding toolkit has an extensive section on domestic abuse – Part 2B: Domestic abuse (covers child and adult).
Recording domestic abuse safely in the patient electronic medical record
- Guidance on recording domestic abuse information in the patient electronic medical record can be found in Part 4 of the RCGP Safeguarding toolkit: Documenting safeguarding concerns and information.
- RCGP guidance on recording of domestic abuse in the electronic medical record
Managing and mitigating risks related to online access to records
- Guidance on managing the risks victims of domestic abuse can face when using patient online access can be found in the RCGP GP online services toolkit: Clinical safety.
eLearning
- Domestic abuse and Women’s Health. This eLearning module considers how domestic abuse may present in the context of women’s health clinical presentations in general practice.
Need help and support for domestic abuse? Here are some national charities:
England
- Refuge. National Domestic Abuse Helpline.Freephone, 24-hour National Domestic Abuse Helpline 0808 2000 247.
- Women’s Aid. Homepage of Women's Aid. National charity working to end domestic abuse against women and children.
- Galop - the LGBT+ anti-abuse charity. Homepage of Galop. Support for LGBT+ people who have experienced abuse and violence.
- ManKind Initiative - Supporting Male Victims of Domestic Abuse. Homepage of Mankind.
- Karma Nirvana. Homepage of Karma Nirvana. Support for victims of Honour Based Abuse.
Northern Ireland
- nidirect. Northern Ireland domestic abuse helpline.24-hour helpline 0808 802 1414.
- Women’s Aid Federation Northern Ireland. Homepage of Women's Aid.
- MAPNI - Men’s Advisory Project. Homepage of MAPNI. Provides counselling services for men experiencing domestic abuse.
Scotland
- Scottish Women’s Aid. Scotland’s Domestic Abuse Helpline.24-hour helpline 0800 027 1234.
- Homepage of Scottish Women’s Aid.
- Safer Scotland. Where to get support for domestic abuse (includes links for support for men, LGBT community and other groups).
Wales
- Welsh government. Live Fear Free Helpline.24-hour helpline 0808 80 10 800.
- Welsh Women’s Aid. Find your local service.
- Dyn Project - Supporting men affected by domestic abuse in Wales. Help for men.
Transitional safeguarding
“Abuse and exploitation doesn’t end at 18 years of age, and yet many of our services for adults are designed to support only those people with ongoing care and support needs. This doesn’t reflect the evidence regarding people’s needs during this developmental life stage and is why many local areas are seeking to adopt a more transitional approach to safeguarding.” (Fran Leddra, Chief Social Worker for Adults, 2021).
What is transitional safeguarding?
- Transitional safeguarding is not simply about safeguarding processes for young people transitioning between services or out of a service -it is about the transition to adulthood itself, which is a journey rather than an event.
- Safeguarding systems for those aged under 18 and those over 18 operate to different thresholds, legislative frameworks and eligibility criteria. This binary approach does not serve young people well and many face a ‘cliff edge’ as they approach age 18 and they risk being left without support during this critical life-stage.
- Transitional safeguarding recognises that the nature of risks and harm may change as children go through adolescence and emerge into adulthood, including greater exposure to risks outside the home, such as criminal or sexual exploitation, drug trafficking and community violence.
- Transitional safeguarding recognises that every young person experiences their transition into adulthood differently, and at different ages, according to their individual circumstances, life history, experiences and maturation.
- Transitional safeguarding is not a set of defined activities but is a systemic approach and way of thinking.
What can general practice do to support transitional safeguarding?
- General practice is a unique service as we care for all age groups, and over a period of time.
- We are skilled in providing holistic, life-long care so are ideally placed to recognise when there is a need for transitional safeguarding.
- Recognise that young people who are being abused and exploited may continue to be abused and exploited when they become 18 years old.
- Recognise when young people may need ongoing safeguarding input once they become 18 years old and highlight this as early as possible to other services involved with the child.
- If the young person is under multi-agency child safeguarding/protection processes, ask what plans are in place for when the young person becomes 18 years.
- Engage with transition plans to ensure children who are on child protection plans or who are in care, and have health needs, e.g. diabetes, asthma, mental health difficulties, are supported to manage their health when they move over to adult health services where they may not get the same intensive input as child services.
- Take a person-centred and human rights-based approach.
- Discuss with the young person what their needs may be when they become 18 years. For example, mental health needs, physical health needs, housing needs (be alert to risks of homelessness), education/work opportunities.
- Signpost or refer young people as needed. For example, arranging an appointment with the practice social prescriber as soon as they become 18 years (as many social prescribers are not able to see anyone under 18 years old).
References
- Department of Health and Social Care. Bridging the gap: transitional safeguarding and the role of social work with adults. 2021.
Part 2C: Identifying adult abuse and neglect
Adult safeguarding is about more than simply keeping someone safe. It is about respecting and protecting an individual’s needs, aspirations and integrity, both mental and physical. It is about making sure the environments they inhabit, and the people and services they encounter with them, reflect the same ideals.
It is important to remember that people are the experts on their own lives and it is our role to work alongside them to identify strengths-based and outcomes-focused solutions – making safeguarding personal. We must work in a way that enhances individual involvement, choice and control as part of improving quality of life, wellbeing and safety.
Making safeguarding personal
Making safeguarding personal involves developing a safeguarding culture that focuses on a person centred and outcome focused approach to safeguarding work. It means adult safeguarding is:
- person-led
- outcome-focused
- engages the person and enhances involvement
- gives choice and control
- improves quality of life, wellbeing and safety
- shifts the focus from process to people.
The six principles of adult safeguarding (embedded in The Care Act 2014) are:
- Empowerment. People being supported and encouraged to make their own decisions and informed consent.
- Prevention. It is better to take action before harm occurs.
- Proportionality. The least intrusive response appropriate to the risk presented.
- Protection. Support and representation for those in greatest need.
- Partnership. Local solutions through services working with their communities. Communities have a part to play in preventing, detecting, and reporting neglect and abuse.
- Accountability. Accountability and transparency in safeguarding practice.
The table below combines the six principles of safeguarding with how the individual should experience them:
Safeguarding adults and human rights
Safeguarding adults and human rights are intrinsically linked and you cannot have one without the other.
“Human rights are the basic rights and freedoms that belong to every person in the world, from birth until death.
They apply regardless of where you are from, what you believe or how you choose to live your life.
They can never be taken away, although they can sometimes be restricted – for example if a person breaks the law, or in the interests of national security.
These basic rights are based on shared values like dignity, fairness, equality, respect and independence.
These values are defined and protected by law.
In Britain our human rights are protected by the Human Rights Act 1998.”
—The Equality and Human Rights Commission
Like with children, there are human rights that are particularly relevant in safeguarding adults:
- Article 2: Right to life.
- Article 3: Freedom from torture and inhuman or degrading treatment.
- Article 4: Freedom from slavery and forced labour.
- Article 5: Right to liberty and security.
- Article 8: Respect for your private and family life, home and correspondence.
- Article 14: Protection from discrimination in respect of these rights and freedoms.
References
- Department of Health and Social Care. Revisiting safeguarding practice. 2022.
- Local Government Association. Making Safeguarding Personal toolkit. 2024
- SCIE. Making Safeguarding Personal (MSP).
- Hampshire Safeguarding Adults Board. One Minute Guide to Making Safeguarding Personal.
- SCIE. What are the six principles of safeguarding?
- CQC (Care Quality Commission). Our updated human rights approach. Updated 2023.
- Equality and Human Rights Commission. Human Rights.
- Department of Health. Safeguarding Adults & the Role of Health Services. Analysis of the Impact on Equality. 2011.
Types of adult abuse
There are ten different types of adult abuse:
- Physical abuse.
- Domestic violence or abuse (see Part 2B).
- Sexual abuse.
- Psychological or emotional abuse.
- Financial or material abuse.
- Modern slavery.
- Discriminatory abuse.
- Neglect or acts of omission.
- Self-neglect.
- Organisational or institutional abuse.
Physical abuse
This includes:
- assault, hitting, slapping, punching, kicking, hair-pulling, biting, pushing
- rough handling
- scalding and burning
- physical punishments
- inappropriate or unlawful use of restraint
- making someone purposefully uncomfortable (e.g. opening a window and removing blankets)
- involuntary isolation or confinement
- misuse of medication (e.g. over-sedation or unauthorised covert medication)
- forcible feeding or withholding food
- unauthorised restraint, restricting movement (e.g. tying someone to a chair).
Signs and indicators include:
- no explanation for injuries or inconsistency with the account of what happened
- injuries which are inconsistent with the person’s lifestyle
- bruising, cuts, welts, burns and/or marks on the body or loss of hair in clumps
- frequent injuries
- unexplained falls
- subdued or changed behaviour in the presence of a particular person
- signs of malnutrition
- failure to seek medical treatment or frequent changes of GP.
Sexual abuse
This includes:
- rape, attempted rape or sexual assault
- inappropriate touch anywhere
- non- consensual masturbation of either or both persons
- non- consensual sexual penetration or attempted penetration of the vagina, anus or mouth
- any sexual activity that the person lacks the capacity to consent to
- inappropriate looking, sexual teasing or innuendo or sexual harassment
- sexual photography or forced use of pornography or witnessing of sexual acts
- indecent exposure.
Signs and indicators include:
- bruising, particularly to the thighs, buttocks and upper arms and marks on the neck
- torn, stained or bloody underclothing
- bleeding, pain or itching in the genital area
- unusual difficulty in walking or sitting
- foreign bodies in genital or rectal openings
- infections, unexplained genital discharge, or sexually transmitted diseases
- pregnancy in a woman who is unable to consent to sexual intercourse
- the uncharacteristic use of explicit sexual language or significant changes in sexual behaviour or attitude
- incontinence not related to any medical diagnosis
- self-harming
- poor concentration, withdrawal, sleep disturbance
- excessive fear/apprehension of, or withdrawal from, relationships
- fear of receiving help with personal care
- reluctance to be alone with a particular person.
Psychological or emotional abuse
This includes:
- enforced social isolation – preventing someone accessing services, educational and social opportunities and seeing friends
- removing mobility or communication aids or intentionally leaving someone unattended when they need assistance
- preventing someone from meeting their religious and cultural needs
- preventing the expression of choice and opinion
- failure to respect privacy
- preventing stimulation, meaningful occupation or activities
- intimidation, coercion, harassment, use of threats, humiliation, bullying, swearing or verbal abuse
- addressing a person in a patronising or infantilising way
- threats of harm or abandonment
- cyber bullying.
Signs and indicators include:
- an air of silence when a particular person is present
- withdrawal or change in the psychological state of the person
- insomnia
- low self-esteem
- uncooperative and aggressive behaviour
- a change of appetite, weight loss/gain
- signs of distress: tearfulness, anger
- apparent false claims, by someone involved with the person, to attract unnecessary treatment.
Financial or material abuse
This includes:
- theft of money or possessions
- fraud, scamming
- preventing a person from accessing their own money, benefits or assets
- employees taking a loan from a person using the service
- undue pressure, duress, threat or undue influence put on the person in connection with loans, wills, property, inheritance or financial transactions
- arranging less care than is needed to save money to maximise inheritance
- denying assistance to manage/monitor financial affairs
- denying assistance to access benefits
- misuse of personal allowance in a care home
- misuse of benefits or direct payments in a family home
- someone moving into a person’s home and living rent free without agreement or under duress
- false representation, using another person’s bank account, cards or documents
- exploitation of a person’s money or assets, e.g. unauthorised use of a car
- misuse of a power of attorney, deputy, appointeeship or other legal authority
- rogue trading, e.g. unnecessary or overpriced property repairs and failure to carry out agreed repairs or poor workmanship.
Signs and indicators include:
- missing personal possessions
- unexplained lack of money or inability to maintain lifestyle
- unexplained withdrawal of funds from accounts
- power of attorney or lasting power of attorney (LPA) being obtained after the person has ceased to have mental capacity
- failure to register an LPA after the person has ceased to have mental capacity to manage their finances, so that it appears that they are continuing to do so
- the person allocated to manage financial affairs is evasive or uncooperative
- the family or others show unusual interest in the assets of the person
- signs of financial hardship in cases where the person’s financial affairs are being managed by a court appointed deputy, attorney or LPA
- recent changes in deeds or title to property
- rent arrears and eviction notices
- a lack of clear financial accounts held by a care home or service
- failure to provide receipts for shopping or other financial transactions carried out on behalf of the person
- disparity between the person’s living conditions and their financial resources, e.g. insufficient food in the house
- unnecessary property repairs.
Modern slavery
This includes:
- human trafficking
- forced labour
- domestic servitude
- sexual exploitation, such as escort work, prostitution and pornography
- debt bondage – being forced to work to pay off debts that realistically they never will be able to.
Signs and indicators include:
- signs of physical or emotional abuse
- appearing to be malnourished, unkempt or withdrawn
- isolation from the community, seeming under the control or influence of others
- living in dirty, cramped or overcrowded accommodation and or living and working at the same address
- lack of personal effects or identification documents
- always wearing the same clothes
- avoidance of eye contact, appearing frightened or hesitant to talk to strangers
- fear of law enforcers.
The Helen Bamber Foundation have developed this ‘Quick Guide to Modern Slavery and Human Trafficking’ which outlines what modern slavery and human trafficking is, how to identify those who might be victims and how to respond.
Discriminatory abuse
This includes:
- unequal treatment based on age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion and belief, sex or sexual orientation (known as ‘protected characteristics’ under the Equality Act 2010)
- verbal abuse, derogatory remarks or inappropriate use of language related to a protected characteristic
- denying access to communication aids, not allowing access to an interpreter, signer or lip-reader
- harassment or deliberate exclusion on the grounds of a protected characteristic
- denying basic rights to healthcare, education, employment, and criminal justice relating to a protected characteristic
- substandard service provision relating to a protected characteristic.
Signs and indicators include:
- the person appears withdrawn and isolated
- expressions of anger, frustration, fear, or anxiety
- the support on offer does not take account of the person’s individual needs in terms of a protected characteristic.
Neglect and acts of omission
This includes:
- failure to provide or allow access to food, shelter, clothing, heating, stimulation and activity, personal or medical care
- providing care in a way that the person dislikes
- failure to administer medication as prescribed
- refusal of access to visitors
- not taking account of individuals’ cultural, religious, or ethnic needs
- not taking account of educational, social and recreational needs
- ignoring or isolating the person
- preventing the person from making their own decisions
- preventing access to glasses, hearing aids, dentures, etc.
- failure to ensure privacy and dignity.
Signs and indicators include:
- poor environment – dirty or unhygienic
- poor physical condition and/or personal hygiene
- pressure sores or ulcers
- malnutrition or unexplained weight loss
- untreated injuries and medical problems
- inconsistent or reluctant contact with medical and social care organisations
- accumulation of untaken medication
- uncharacteristic failure to engage in social interaction
- inappropriate or inadequate clothing.
Self-neglect
Self-neglect is an extreme lack of self-care, it is sometimes associated with hoarding and may be a result of other issues such as addictions.
Self-neglect includes:
- lack of self-care to an extent that it threatens personal health and safety
- neglecting to care for one’s personal hygiene, health or surroundings
- inability to avoid self-harm
- failure to seek help or access services to meet health and social care needs
- inability or unwillingness to manage one’s personal affairs.
Signs and indicators include:
- very poor personal hygiene
- unkempt appearance
- lack of essential food, clothing or shelter
- malnutrition and/or dehydration
- Living in squalid or unsanitary conditions
- neglecting household maintenance
- hoarding
- collecting a large number of animals in inappropriate conditions
- non-compliance with health or care services
- inability or unwillingness to take medication or treat illness or injury.
Self-neglect can be as a result of:
- a person’s brain injury, dementia, or other mental disorder
- obsessive compulsive disorder or hoarding disorder
- physical illness which has an effect on abilities, energy levels, attention span, organisational skills or motivation
- reduced motivation as a side effect of medication
- addictions
- traumatic life change.
It is not always possible to establish a root cause. Hoarding and self-neglect do not always appear together, and one does not necessarily cause the other.
People who neglect themselves often decline help from others; in many cases they do not feel that they need it. Family or neighbours can sometimes be critical of professionals because they don’t do anything to improve the situation of the individual. But there are limitations to what others can do if the adult has mental capacity to make their own decisions about how they live. Sometimes, even when all agencies have done everything in their power to support an individual, they may die or suffer significant harm as a result of their own action or inaction. It is therefore vital that all efforts to engage with and support an individual are clearly recorded.
Barriers to working with and caring for individuals who self-neglect
- Can be challenging & alarming.
- Support/help may be refused.
- Risks are high.
- Intervention options limited.
- Lack of clarity on who takes responsibility including when help is refused.
- Resources and work patterns don’t support long-term relationship-based work.
- Lack of resources.
- Safeguarding responses not always appropriate if don’t have care & support needs.
- May be no decision-making forum.
- Information sharing can be problematic.
- Limited legal literacy.
- Assessment of capacity/ application of mental capacity legislation can be very complex (See Part 3 in the toolkit for further guidance on assessing capacity in self-neglect).
Best practice
Research has shown that those who self-neglect may be deeply upset and even traumatised by interventions such as ‘blitz’ or ‘deep cleaning’. When developing an approach it is important to try to understand the individual and what may be driving their behaviour. There are some general pointers for an effective approach:
- Multi-agency – work with partners to ensure the right approach for each individual.
- Person centred – respect the views and the perspective of the individual, listen to them and work towards the outcomes they want.
- Acceptance – good risk management may be the best achievable outcome, it may not be possible to change the person’s lifestyle or behaviour.
- Analytical – it may be possible to identify underlying causes that help to address the issue.
- Non-judgemental – it isn’t helpful for practitioners to make judgements about cleanliness or lifestyle; everyone is different.
- Empathy – it is difficult to empathise with behaviours we cannot understand, but it is helpful to try.
- Patience and time – short interventions are unlikely to be successful, practitioners should be enabled to take a long-term approach.
- Trust – try to build trust and agree small steps.
- Reassurance – the person may fear losing control, it is important to allay such fears.
- Bargaining – making agreements to achieve progress can be helpful but it is important that this approach remains respectful.
- Exploring alternatives – fear of change may be an issue so explaining that there are alternative ways forward may encourage the person to engage.
- Always go back – regular, encouraging engagement and gentle persistence may help with progress and risk management.
Other considerations:
- Risk assessment – have effective, multi-agency approaches to assessing and monitoring risk.
- Assess capacity – ensure staff are competent in applying the Mental Capacity Act in cases of self-neglect.
- Mental health assessment – it may, in a minority of cases, be appropriate to refer an individual for Mental Health Act Assessment.
- Signpost – with a multi-agency approach people can be signposted to effective sources of support.
- Contact family – with the person’s consent, try to engage family or friends to provide additional support.
- Decluttering and cleaning services – where a person cannot face the scale of the task but is willing to make progress, offer to provide practical help.
- Utilise local partners – those who may be able to help include the RSPCA, the fire service, environmental health, housing, voluntary organisations.
- Occupational therapy assessment – physical limitations that result in self-neglect can be addressed.
- Help with property management and repairs – people may benefit from help to arrange much needed maintenance to their home.
- Peer support – others who self-neglect may be able to assist with advice, understanding and insight.
- Counselling and therapies – some individuals may be helped by counselling or other therapies. Cognitive behaviour therapy, for example, may help people with obsessive compulsive disorder, hoarding disorder, or addictions.
References
- Social Care Institute of Excellence. Types and indicators of abuse. 2020.
- Social Care Institute of Excellence. Self-neglect at a glance. 2024.
Organisational abuse
Organisational abuse (also known as institutional abuse) includes neglect and poor care practice within a specific care setting. This could be a hospital or care home but also the care someone receive in their own home. The abuse can either be a one-off incident or an ongoing culture of ill-treatment. The abuse can take many forms, including neglect. It can affect one person or many residents. Some aspects of organisational abuse may be hidden (closed cultures) and staff may act differently when visitors are there (disguised compliance). It can be difficult to differentiate between poor practice and ongoing organisational abuse.
Organisational abuse is distinct from other forms of abuse or neglect because it is not directly caused by individual action or inaction. Instead, it is a cumulative consequence of how services are managed, led and funded. This also therefore means that there is no on size fits all approach for managing and responding to organisational approach. This is because of the huge range of actions and inactions that may contribute to organisational abuse, at all managerial and financial levels within organisations. Organisational abuse can also be caused by a single act of neglect or omission.
Organisational abuse is particularly important for GPs and all general practice staff to be aware of because many of our adults at risk of harm will live permanently, or spend time, in institutions such as nursing/residential homes or homes for adults with learning disabilities. They may also spend time in healthcare facilities such as hospitals (NHS or private). Many will also receive care at home.
Types of organisational or institutional abuse:
- Discouraging visits or the involvement of relatives or friends.
- Run-down or overcrowded establishment.
- Authoritarian management or rigid regimes.
- Lack of leadership and supervision.
- Insufficient staff or high turnover resulting in poor quality care.
- Abusive and disrespectful attitudes towards people using the service.
- Inappropriate use of restraints.
- Lack of respect for dignity and privacy.
- Failure to manage residents with abusive behaviour.
- Not providing adequate food and drink, or assistance with eating.
- Poor care of hygiene resulting in pressure areas and pressure sores.
- Not offering choice or promoting independence.
- Misuse of medication.
- Failure to provide care with dentures, spectacles or hearing aids.
- Not taking account of individuals’ cultural, religious, or ethnic needs.
- Failure to respond to abuse appropriately.
- Interference with personal correspondence or communication.
- Failure to respond to complaints.
Signs and indicators of organisational or institutional abuse:
- Lack of flexibility and choice for people using the service.
- Inadequate staffing levels.
- People being hungry or dehydrated.
- Poor standards of care.
- Lack of personal clothing and possessions and communal use of personal items.
- Lack of adequate procedures.
- Poor record-keeping and missing documents.
- Absence of visitors.
- Few social, recreational, and educational activities.
- Public discussion of personal matters.
- Unnecessary exposure during bathing or using the toilet.
- Absence of individual care plans.
- Lack of management overview and support.
Common safeguarding challenges in care homes:
- Maladministration of medication.
- Pressure sores.
- Falls.
- Rough treatment, being rushed, shouted at, ignored.
- Lack of social inclusion.
- Institutionalised care.
- Physical abuse between residents.
- Financial abuse.
Further information can be found at Social Care Institute for Excellence.
Underlying causes of safeguarding challenges in care homes:
- Recruitment.
- Staffing levels.
- Adherence to policy and procedure.
- Training.
- Choice of service.
- Record keeping.
- Dehumanisation.
Dehumanisation is closely related to burnout. Dehumanisation can be experienced in different ways:
- Discriminated against or treated differently to others.
- Isolated, dismissed or ignored.
- Disrespected, mocked or belittled.
- Deprived of dignity and privacy.
- Deprived of choice and control.
- Stripped of one’s identity.
- Deprived of basic needs (e.g. food).
- Abused physically, sexually or in any other way.
NICE guideline [NG189]: Safeguarding adults in care homes
NICE guideline outlines in detail the possible indicators of institutional abuse and actions to take. Within the guideline, the terms ‘consider’ and ‘suspect’ are used to define the extent to which an indicator suggests abuse or neglect, with 'suspect' indicating a stronger likelihood of abuse or neglect. None of the indicators are proof of abuse or neglect on their own.
Indicators that should lead to ‘considering’ organisational abuse and neglect:
- Policy and governance issues.
- Failing contractual or regulatory standards.
- Mismanagement of safeguarding concerns and poor record keeping.
- Staffing problems.
- Poor quality of care.
- Failure to refer residents for care.
- Financial mismanagement.
- Physical signs and lack of openness.
Actions to take if you are considering organisational abuse or neglect:
- Raise the matter with the care home manager, in writing if possible.
- If the care home manager is believed to be part of the problem, go to the group manager, regional manager, owner or board of trustees.
- If the care home manager is the sole owner, follow the actions to take if you suspect abuse or neglect.
- Explain the impact on residents, or the likely impact if the situation continues.
- Ask for a response within a specified period of time (for example two weeks)
- If the manager agrees to make changes, make sure these happen.
- After taking these steps, if the situation does not improve, raise your level of concern to 'suspect'.
Indicators that should lead to ‘suspecting’ organisational abuse or neglect:
- Incidents of abuse or neglect not reported.
- Evidence of falsified or missing records.
- Multiple hospital admissions leading to safeguarding enquiries.
- Residents repeatedly cannot access medical/dental care.
- Frequent unexplained deterioration in residents’ health and wellbeing.
- Misuse of residents’ money.
- Sudden increase in safeguarding concerns.
- Residents repeatedly evicted, or they and their families feel victimised, when they complain.
- Care home fails to improve in response to reviews, inspections or audits and deteriorates over time.
Action to take if you suspect organisational abuse or neglect:
- Make an adult safeguarding referral following your local multi-agency safeguarding processes.
Management of concerns about organisational abuse
It is important to acknowledge that this is a complex area and there are many different professionals and organisations who may be involved such as local authority, police, safeguarding professionals across health and social care, commissioners and independent regulators. Any practitioner who has concerns about organisational abuse should seek prompt safeguarding advice if they are unsure how to proceed or unsure if their observations are indicators of abuse.
Good practice points to consider
- Within your practice/organisation, is there a regular and formal discussion about care homes attached to your practice (for example, nursing and residential homes and homes for adults with learning disabilities; it can also include children’s homes)?
- How are early or minor concerns about care homes being recorded within the practice/organisation including when these are not about a specific patient?
- Is there a clear pathway within the practice/organisation to raise concerns about a care home as it may be any member of the team who may have concerns including medication/pharmacy teams?
References
- Social Care Institute of Excellence. Types of organisational or institutional abuse. 2020.
- Ann Craft Trust. What is Organisational Abuse? 2024.
- NICE Clinical Knowledge Summaries. What is abuse and neglect? Updated 2022.
- NICE guideline. NG189. Safeguarding adults in care homes. 2021.
- Social Care Institute of Excellence. Commissioning care homes: common safeguarding challenges. 2012.
Adults at greater risk of abuse and neglect
Any adult can be a victim of abuse and neglect and many adults (including some adults with additional needs/care and support needs) are able to protect themselves from abuse or take appropriate action to prevent or stop abuse happening to them. However, some adults are unable, or less likely to be able, to protect themselves from abuse. This can include:
- people with care and support needs, such as older people or people with disabilities, are more likely to be abused or neglected -they may be seen as an easy target and may be less likely to identify abuse themselves or to report it
- people with drug or alcohol addiction
- people with mental health difficulties
- people with brain injuries
- people with dementia
- people from marginalised groups such as sex workers and refugees
- people with communication difficulties can be particularly at risk because they may not be able to alert others.
Sometimes adults may not even be aware that they are being abused, and this is especially likely if they have a cognitive impairment.
References
- Social Care Institute for Excellence. What is safeguarding?
- Refugee Action. Safeguarding. 2016.
- Amnesty International. Sex Workers’ Rights. 2017.
- The Law Society. Financial Abuse. 2023.
How does adult abuse/neglect present in general practice?
Like child abuse, presentations of adult abuse and neglect in general practice are seldom clear-cut and well-defined. Adults may not recognise that what they are experiencing is abuse and individuals can experience multiple different types of abuse at the same time.
Below are some examples of how adult abuse and neglect may present in general practice. This list is not exhaustive.
- Disclosures from the adult.
- Physical signs, e.g. bruises, injuries.
- Behaviour changes e.g. more withdrawn, more angry, challenging behaviour.
- Mental health concerns, e.g. anxiety, depression, self-harm, suicidal thoughts/attempts.
- Drug and alcohol issues.
- Family/carers sharing concerns.
- Interactions between the adult and others such as family or carers that causes concern.
- The adult displays harmful behaviour towards others.
- Disclosures from a family member/carer about abuse in their own life, e.g. domestic abuse, that also indicates abuse to the adult.
- Indicators of institutional abuse/neglect in places such as care homes and residential homes.
- Information shared from other health colleagues or other agencies/professionals.
- Missed appointments – repeated patterns of adults not being brought to health appointments or missing appointments.
- Behaviour of a colleague or a Person in Position of Trust that gives concerns they may be a risk to adults with care and support needs.
It is worth noting that the signs of lots of different types of abuse can be similar. For example, an adult who presents with mental health difficulties and substance misuse issues could be experiencing any type of abuse. It is therefore important for practitioners to be able to recognise the signs that can indicate potential abuse and neglect in adults to be able to ask appropriate questions and take appropriate safeguarding action.
Safeguarding those who are homeless
“Homelessness is devastating, dangerous and isolating.”
—Crisis
Those who experience homelessness are members of our communities who have high levels of need but also experience marked barriers to services and the support they need, including health services.
Homeless people have significantly lower life expectancy. According to the Census 2021 data, the average age of death of a homeless man is 45 years. The average age of death of a homeless woman was 43 years.
People sleeping on the street are almost 17 times more likely to have been victims of violence. More than one in three people sleeping rough have been deliberately hit or kicked or experienced some other form of violence whilst homeless.
Homeless people are over nine times more likely to take their own life than the general population.
Findings from an audit carried out by Homeless Link found that:
- people experiencing homelessness suffer worse physical and mental health than the general population
- 63% of respondents reported they had a long-term illness, disability, or infirmity
- there is a substantial increase in the number of people with a mental health diagnosis – 82%
- 45% respondents reported they are self-medicating with drugs or alcohol to help them cope with their mental health
- there are significant barriers to healthcare and that people experiencing homelessness are over reliant on emergency health care services
- for those who had been admitted to hospital, 24% had been discharged to the streets
- nutrition presents a big challenge – a third of respondents reported they only eat one meal/day on average.
Types of homelessness:
- Rough sleeping: this is the most visible form of homelessness.
- In temporary accommodation: this includes night/winter shelters, hostels, B&Bs, women’s refuges, private and social housing.
- Hidden homelessness such as staying with family or friends, sofa surfing or living in unsuitable housing such as squats or in ‘beds in sheds’ situations.
- Statutory homelessness: families or individuals who are accepted as being owed support by their local council because they are likely to become homeless or are homeless.
Multiple exclusion homelessness
Definition:
“People who have been ‘homeless’ (including experience of temporary/unsuitable accommodation as well as sleeping rough) and have also experienced one or more of the following additional domains of deep social exclusion – ‘institutional care’ (prison, local authority care, psychiatric hospitals or wards); ‘substance misuse’ (drug problems, alcohol problems, abuse of solvents, glue or gas); or participation in ‘street culture activities’ (begging, street drinking, ‘survival’ shoplifting or sex work).”
Multiple Exclusion Homelessness. A Safeguarding Toolkit for Practitioners.
Adults experiencing multiple exclusion homelessness face:
- significant increased risk of serious abuse, exploitation and neglect
- an escalation of their health and care needs
- a reduction to their life expectancy.
They also have hidden vulnerabilities which include:
- problems stemming from childhood trauma
- acquired brain injuries
- chronic mental and physical ill-health
- limited mobility
- severe addiction: “individuals experiencing multiple exclusion homelessness are in a life threatening double bind, driven addictively to avoid suffering through ways that only deepen their suffering.” (Adult safeguarding and homelessness: experience informed practice by Local Government Association).
Many people who are at risk of, or who are experiencing, long term homelessness have been exposed to trauma. Trauma is prevalent in the narrative of many people’s pathways to homelessness. Research has shown that people who are homeless are likely to have experienced some form of trauma, often in childhood. 85% of those in touch with the criminal justice system, substance misuse and homelessness services have experienced trauma as children.
People who are homeless are vulnerable to all types of abuse. The safeguarding issues surrounding them are often highly complex and can include experience of abuse and trauma as a child and an adult, ongoing vulnerability to abuse, exposure to violence and high risk of death from treatable medical causes, violence, suicide, and/or drug overdoses. Where someone may present a risk of harm to others this has to be carefully managed. Some may also be parents and therefore safeguarding of children must always be taken into consideration.
Safeguarding people experiencing homelessness
Safeguarding people experiencing homelessness should follow the same principles as safeguarding any adult which are set out in section 3 of this toolkit: Responding to abuse and neglect. Additional risks and needs of this population also need to be taken into account which are set out in Homeless Link Safeguarding Adults at Risk guidance.
Interpersonal and personal:
- Mental health needs.
- Dependence on alcohol and/or drugs.
- Brain damage.
- Lack of purposeful activity.
- Odd, anti-social or embarrassing behaviour.
- Difficulty in communicating.
- Impact of trauma and adverse experiences.
- Poverty.
External:
- Staff working in isolation.
- Unconscious bias, stereotyping and prejudice.
- Community disengagement, fear and resentment.
- Lack of access to safe and adequate housing.
- Lack of access to wrap-around support to address health and social care needs.
- Victim of gatekeeping and inflexible policies.
GP Registration
A particular barrier to healthcare for people experiencing homelessness can be difficulty registering with a GP. This however should not be the case. EVERYONE in England, Northern Ireland, Scotland and Wales is eligible to register with a GP and receive primary care services free of charge. Homeless patients are entitled to register with a GP using a temporary address, which may be a friend’s address or a day centre. The practice address may also be used to register them which can mean letters about appointments, for example, can be sent on proactively or opportunistically.
Relevant guidance on patient registration is available here:
- England
- BMA. Patient registration. 2024.
- Care Quality Commision. GP mythbuster 29: Looking after homeless patients in General Practice.2024.
- Wales
- Cardiff and Vale University Health Board. Registering with a GMS Practice.
- Scotland
- NHS Inform. Registering with a GP practice.
- Northern Ireland
- nidirect. Your local doctor (GP).
Doctors of the World also have a helpful briefing on GP registration:
“Refugee and migrant communities, people experiencing homelessness, and Gypsy Roma and Traveller communities, have low levels of GP registration and are often incorrectly prevented from registering with a GP surgery. Everyone in England, Scotland, and Wales is eligible to register with a GP and receive primary care services free of charge, regardless of immigration status. This is because immigration status is not relevant for primary care, and anyone can register and use primary care services. Some surgeries may ask to provide documents, such as proof of address, proof of identity or proof of immigration status, or an NHS number in order to register, but they should not refuse to register if these can’t be provided. If individuals can’t provide these documents, they should say that they don’t have these documents but that they do live within the practice boundary and would like to register with the GP as a patient.”
Doctors of the World also have a Safe Surgeries Toolkit to support GP practice staff in ensuring everyone in their community can access the healthcare they need.
References
- Crisis. About homelessness.
- Homeless Link. Unhealthy State of Homelessness 2022: Findings form the Homeless Health Needs Audit. 2022.
- Crisis. Types of homelessness.
- Homeless Link. Guidance on Safeguarding. 2024.
- Expert Citizens CIC. Multiple Exclusion Homelessness. A Safeguarding Toolkit for Practitioners. 2023.
- Office for National Statistics. Census 2021. Deaths of homeless people in England and Wales: 2021 registrations. 2022.
Was not brought (adult)
Just as with children, adults with care and support needs who are not being brought to health appointments can be a sign of neglect or other abuse, a sign that a family or carers might need additional support, or a sign that an adult needs reasonable adjustments to be able to access healthcare. The term ‘was not brought’ is now widely used across health regarding children and is also now being used with regards to adults with care and support needs.
There are many reasons why an adult with care and support needs may need help and support to attend healthcare appointments.
Practices and organisations should have a process in place for whenever any adult does not attend an appointment or review (such as annual learning disability reviews) in general practice. This is in order to identify:
- adults with care and support needs who needed to be brought to the appointment
- adults with care and support needs who may need reasonable adjustments to be able to access general practice independently
- what the purpose of the appointment was and what is the subsequent impact of the missed appointment or review on that adult’s health and wellbeing
- reasons why the adult with care and support needs was not brought to the appointment or was not able to attend the appointment independently
- what follow up is required
- any reasonable adjustments that need to be made for the adult with care and support needs
- any additional support the adult or their families/carers may need such as a carer’s assessment
- any safeguarding concerns.
To identify whether this missed appointment is part of wider safeguarding concerns, the following questions should be considered:
- What is known about the level of severity of care and support needs the adult has?
- What is known about the capabilities of the adult?
- What was the purpose of the appointment (which may not be known)? If the purpose is known, what could the potential impact of the missed appointment be on the adult's health and welfare?
- Does the adult have any ongoing physical or mental health problems?
- Could this missed appointment indicate a worsening of the adult’s health issues such as dementia?
- Are there other health appointments that the adult has not been brought to/has not attended? Is there a pattern of missed appointments?
- Is there a high volume of emergency department and GP out of hours attendances?
- Are there any safeguarding concerns documented in the adult's records? If so, how does this missed appointment fit into the wider picture? If not, could this missed appointment be an indicator of emerging safeguarding concerns?
- Are there any other adults with care and support needs, or children, within the household/family/residence? If so, are there any safeguarding concerns relating to them? For example, if all the residents of a residential home for adults with learning disabilities are registered with your practice, are there any other safeguarding concerns about any of the other residents which might indicate a wider concern about abuse or neglect within the home?
- Are there any concerns about the family/carers that could impact on their ability to bring the adult to health appointments, for example physical or mental health problems, drug and alcohol issues, domestic abuse, safeguarding concerns?
- Is there evidence of carer strain?
If there are any safeguarding concerns about the adult, action needs to be taken proportionate to the level of concern. This could include:
- the practice contacting the adult/family/carers to arrange another appointment
- the clinician contacting the adult/family/carers yourself why the adult has not been brought and make a further assessment
- contacting other professionals who may be involved with the adult, such as the learning disability team or social worker, to share information and concerns to aid further decisions
- considering an adult safeguarding referral.
In all cases, it is important to document your actions and reasons for them.
Adults without documented care and support needs who do not attend appointments
It is important to also recognise the adults who may not have documented care and support needs but have known safeguarding concerns or vulnerabilities that should prompt further exploration and concern when they do not attend an appointment. For example, someone who is known to be a victim of domestic abuse or someone who is homeless.
Prevention of Adult Not Brought Strategy, North East and Cumbria Learning Disability Network
The North East and Cumbria Learning Disability Network’s ‘Prevention of Adult Not Brought Strategy’ has a wide range of resources to support general practice including Top Tips for Primary Care, a Reasonable Adjustments flowchart and a Reasonable Adjustments Level of Concern tool.
Part 3A: Responding to abuse and neglect
Presentations of abuse in general practice are seldom clear-cut and well-defined, and different types of abuse can overlap in the same child or adult. The context for concerns is often more important than the identification of an 'incident'. Safeguarding is often likened to a jigsaw puzzle. Often, it is only when individuals and agencies share information together that the picture is complete. This involves effective record keeping, information-sharing and communication, both internally and between agencies.
Building up a picture of what is life is like for a child, or an adult at risk of harm is key to keeping them safe, alongside ensuring that the ‘voice’ of the child or adult is central to everything that we do.
As outlined in the previous section of the toolkit, ‘Identification of abuse and neglect’, abuse can present in lots of different ways to general practice. There are many similarities to the presentations of the different types of abuse. For example, mental health difficulties can be a common presentation of all types of abuse in children or adults.
As GPs we have a unique and privileged role. Patients and their families allow us into their lives, often at times of great distress, in order to support and help them. This is a great privilege, which comes with great responsibility. The area of safeguarding is an area of clinical care where these two roles, privilege and responsibility, very clearly meet. Combining these roles enables us to be powerful advocates for our most vulnerable patients.
How should we respond when we have concerns that a child or adult is experiencing abuse?
The response will depend on the individual, their circumstances and the context. Some situations will be very straightforward. For example, if a 12 year old girl tells you her dad is sexually abusing her or you witness a carer hitting an 88 year old man living in a care home, it is very clear that an urgent safeguarding referral will need to be done. However, abuse rarely presents in such an obvious way. This is why it is so important to be aware of the indicators of potential abuse so that we are able to identify those who are experiencing abuse in order for them to be protected and receive the right support.
Our response will also depend on where we work. For example, a GP working in an out of hours setting or in an independent GP clinic, may not have the same access to information about the individual, their family or carers and wider context than a GP who works in an NHS practice will have. Therefore, thresholds for safeguarding referrals may need to be lower for those who have safeguarding concerns about an individual when their job role means that building up a picture over time or reviewing information held in multiple family member’s records, is not possible.
Responding appropriately and effectively in general practice to concerns about abuse
The following are key knowledge and capability principles to responding appropriately and effectively in general practice to concerns about abuse:
KNOWLEDGE
- Knowing the indicators of abuse:
- If we do not know the indicators of abuse then we will not recognise it and not respond appropriately.
- Knowledge of local safeguarding referral processes:
- Knowing your local safeguarding referral processes is fundamental to responding effectively to concerns about abuse. Not knowing how to make referrals can be a substantial barrier. You should know:
- how to find the referral forms for child and adult safeguarding referrals
- how to find phone numbers to use for safeguarding advice or making urgent safeguarding referrals, including outside of working hours
- the process for Early Help referrals
- how to make referrals to local domestic abuse agencies
- how to make multi-agency risk assessment conference (MARAC) referrals
- how to manage allegations against staff/persons in positions of trust
- how and when to carry out the mandatory reporting duty of female genital mutilation (FGM) (England and Wales)
- how to make Prevent referrals (England, Wales and Scotland) as these processes can vary from place to place.
- Knowing your local safeguarding referral processes is fundamental to responding effectively to concerns about abuse. Not knowing how to make referrals can be a substantial barrier. You should know:
- Knowledge that it is not the role of a GP or anyone in general practice to investigate allegations or concerns about abuse – that is the role of other agencies such as social care and the police.
- Knowing when and how to ask for help.
- Knowing how and when to challenge:
- Critical thinking and challenge within and between agencies is essential to safeguarding work. The lack of this was highlighted as a factor in the National review into the murders of Arthur Labinjo-Hughes and Star Hobson.
- Knowing when and how to escalate safeguarding concerns:
- Knowing how and when to escalate safeguarding concerns is essential. These situations can occur when you have concerns about the multi-agency response to your safeguarding concerns such as a safeguarding referral not being accepted or closed without further action. You should know:
- who to seek advice from
- how to escalate concerns.
- Knowing how and when to escalate safeguarding concerns is essential. These situations can occur when you have concerns about the multi-agency response to your safeguarding concerns such as a safeguarding referral not being accepted or closed without further action. You should know:
CAPABILITIES
- Assessing risk and vulnerability:
- If we only take situations at face value, we may significantly underestimate the risk of abuse that a child or adult may be facing. Any concern should not be viewed in isolation, but put into context, including by exercising our professional curiosity.
- It is vital to understand personal or life characteristics which can make an individual more vulnerable to abuse. Understanding these characteristics help us to develop a more accurate picture of the risk of abuse that an individual might face.
- Seeing the wider picture:
- A ‘think family’ approach when considering the needs of children. This approach means thinking about the needs of the whole family – as individuals and as a unit without losing sight of the need for individual care. For example, this may mean addressing the health needs of parents or involving other professionals and agencies to support the family with social needs.
- When treating adults, it is important to always consider whether they have caring responsibilities for children or adults with care and support needs and what the impact of the adult’s health. ‘Seeing the child behind the adult’ is an important principle to follow.
- This approach is also important when considering adults at risk of harm and how best to support and protect them. For example, considering and addressing the needs of carers for example is vital to supporting the adult they are caring for. This includes young carers.
- Be aware that general practice only have one part of the safeguarding jigsaw puzzle.
- Being confident in issues surrounding consent and confidentiality:
- Concerns around consent and confidentiality can present some of the biggest challenges to responding effectively to abuse but should not be a barrier to sharing information in order to safeguard children, and adults at risk of harm, from abuse and neglect. Part 5 of this toolkit (Information sharing and multiagency working) provides further guidance on these difficult areas.
- Robustly assessing mental capacity:
- Assessing capacity when there are safeguarding concerns can be challenging especially in situations when capacity fluctuates, where there are alcohol or drugs involved, when coercive control is suspected or there is self-neglect. Capacity can also be significantly impacted by previous experiences of trauma.
- If we do not fully and accurately assess capacity, including executive capacity (ie the ability to not just make, but also carry out, a decision), then adults at risk of harm may not receive the protection and support they need.
- The use of the phrase ‘lifestyle choice’ should be used with extreme caution as this risks professionals under-estimating risk. This phrase is often used for individuals who are self-neglecting, are homeless or who have alcohol or drug addiction. It is important to resist this narrative as the reality is usually complex. It is also important to guard against assumptions that individuals can protect themselves in these complex situations.
- Differentiation between inability and unwillingness to care for oneself, and capacity to understand the consequences of one’s actions, are crucial determinants of response.
Talking to children, adults, families and carers about abuse
Talking to patients about your concerns about abuse and safeguarding referrals can seem daunting and at times uncomfortable, even for those who are experienced clinicians. However, many of the skills needed to have these conversations are skills we already have as GPs and general practice clinicians. Some good practice points to consider when talking about concerns about abuse are:
- Meet language and communication needs – this is particularly important when talking about abuse. If an interpreter is needed, this should be an independent interpreter, not family members or carers. Choice of interpreter is also important. Phone interpreters can allow anonymity which can be helpful.
- As far as is possible, communicate directly with the child/adult you are concerned about. This may include arranging to speak with them alone, dependent on age, maturity, communication needs as well as their care and support needs.
- Actively listen to the child/adult you are concerned about.
- Start the conversation by asking open questions.
- Listen without judging.
- Remain calm.
- Be honest and transparent about your concerns (as long as this will not increase the risk of harm to the child or adult at risk of harm).
- Offer support including signposting to any relevant external support.
- Don’t collude with, or excuse, any harmful behaviour.
- It is not the role of a GP or anyone in general practice to investigate allegations or concerns about abuse.
- Be aware that you may have only have one part of the safeguarding jigsaw puzzle.
- Understand that for families and carers the realisation that their child or loved one may be being abused can be devastating news and that reactions can vary significantly.
- Be clear about your professional duties regarding safeguarding children and adults at risk of harm.
- Be clear about confidentiality and its limits.
- Be prepared to have more than one conversation.
- Focus on the rights of children and adults to live free from harm and fear.
- Reflect on your conversations, especially if it has been difficult – this could be with a colleague or organisational safeguarding lead for example.
- Take time for yourself.
References:
- GMC. Protecting children and young people: The responsibilities of all doctors. Communication and support. 2024.
- GMC. Leaflet: What to expect if your doctor is worried about your child’s safety. 2012.
- Ann Craft Trust. What should I say…? Advice for Starting Difficult Conversations. 2022.
- Age UK. How to have an open conversation. 2024.
- Open the Door Cheshire. Opening up the conversation. 2022.
Trauma-informed practice
“Trauma results from an event, a series of events, or set of circumstances that is experienced by an individual as harmful or life threatening. The experience of trauma can cause lasting adverse effects, limiting the ability to function and achieve mental, physical, social, emotional or spiritual well-being.”
Definition of trauma-informed practice:
“An approach to health and care interventions which is grounded in the understanding that trauma exposure can impact an individual’s neurological, biological, psychological and social development.”
Trauma-informed practice requires practitioners, organisations and systems to look beyond presenting behaviour and ask ‘what happened to this person?’ rather than ‘what is wrong with this person?’.
Experience of trauma can:
- impact physical and mental health
- impact education
- impact behaviour
- lead to behaviour which is perceived as ‘challenging’ or ‘difficult’
- impact accessing healthcare, such as: making appointments, keeping appointments, expressing yourself, having invasive investigations, use of language
- lead to fear of other services becoming involved
- impact ability to care for self and others
- impact ability to regulate own emotions
- impact family support
- lead down a path to criminal activity.
How can we be trauma-informed and carry out trauma-informed practice in general practice?
- Be aware how common trauma related to abuse is.
- Be mindful that current or past trauma may impact any of your patients.
- Understand that examinations and investigations may be particularly triggering for those who have experienced trauma. The Survivors Trust have a campaign ‘Check with me first’ which highlights three small actions to help survivors of sexual abuse to feel more comfortable and empowered if being examined during healthcare appointments. While these are about examination, the principles could be applied to all aspects of a healthcare consultation:
- CHECK. Ask the individual if they are comfortable before and during each step of the examination.
- EXPLAIN. Help the service-user feel at ease by explaining each step of the examination before you do it and encourage them to ask questions.
- REASSURE. Remind the individual that they can stop the procedure at any time – they are in control.
Trauma-informed practice is:
- asking about abuse/trauma in a sensitive way
- providing opportunities for disclosure of abuse when appropriate
- listening
- giving choice
- empowering
- taking a strengths-based approach
- giving control back
- not putting everything down to abuse/trauma.
Principles of trauma-informed practice:
- people knowing they are safe or asking what they need to feel safe
- there being reasonable freedom from threat or harm
- attempting to prevent re-traumatisation
- putting policies, practices and safeguarding arrangements in place.
- the organisation and staff explaining what they are doing and why
- the organisation and staff doing what they say they will do
- expectations being made clear and the organisation and staff not overpromising.
- ensuring service users and staff have a voice in the decision-making process of the organisation and its services
- listening to the needs and wishes of service users and staff
- explaining choices clearly and transparently
- acknowledging that people who have experienced or are experiencing trauma may feel a lack of safety or control over the course of their life which can cause difficulties in developing trusting relationships.
- using formal and informal peer support and mutual self-help
- the organisation asking service users and staff what they need and collaboratively considering how these needs can be met
- focussing on working alongside and actively involving service users in the delivery of services.
- validating feelings and concerns of staff and service users
- listening to what a person wants and needs
- supporting people to make decisions and take action
- acknowledging that people who have experienced or are experiencing trauma may feel powerless to control what happens to them, isolated by their experiences and have feelings of low self-worth.
- offering access to gender responsive services
- leveraging the healing value of traditional cultural connections
- incorporating policies, protocols and processes that are responsive to the needs of individuals served.
References
- Office for Health Improvement & Disparities. Guidance: Working definition of trauma-informed practice. 2022.
- Home Office. Trauma informed practice: learning from experience. 2024.
- NAPAC (The National Association for People Abused in Childhood). What are the six key principles of a trauma-informed approach? 2023.
- The Survivors Trust. Resources for Healthcare Services.
- The Survivors Trust. About #CheckWithMeFirst.
Part 3B: Responding to concerns about child abuse
The child’s voice
Children are clear what they want from an effective safeguarding system. Children have said that they need
- Vigilance: to have adults notice when things are troubling them.
- Understanding and action: to understand what is happening; to be heard and understood; and to have that understanding acted upon.
- Stability: to be able to develop an ongoing stable relationship of trust with those helping them.
- Respect: to be treated with the expectation that they are competent rather than not.
- Information and engagement: to be informed about, and involved in procedures, decisions, concerns and plans.
- Explanation: to be informed of the outcome of assessments, and decisions and reasons when their views have not met with a positive response.
- Support: to be provided with support in their own right as well as a member of their family.
- Advocacy: to be provided with advocacy to assist them in putting forward their views.
- Protection: to be protected against all forms of abuse, exploitation, and discrimination, and the right to special protection and help if a refugee.
Responding to concerns about child abuse is a five step process
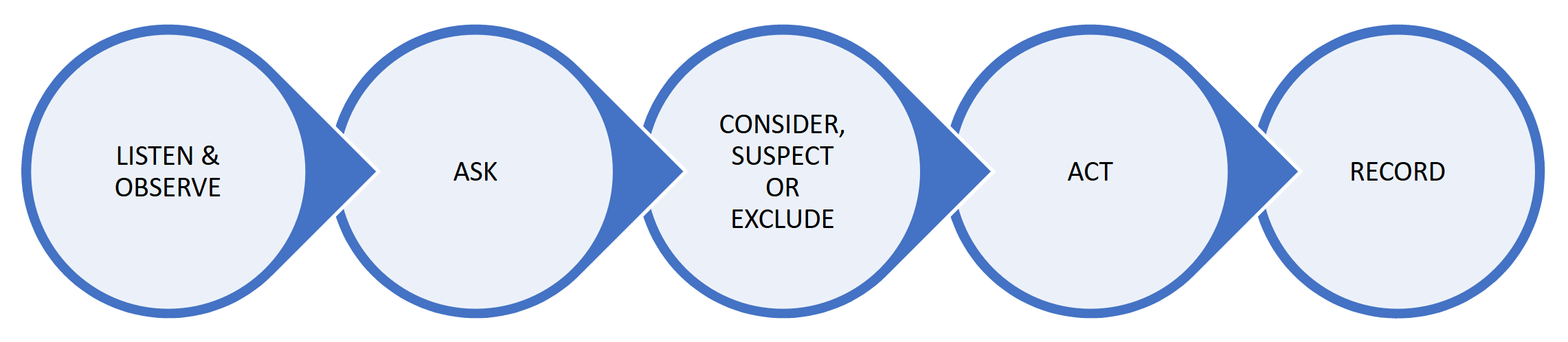
Step 1: Listen and observe.
Piece together information you already have:
- Any history, disclosure, physical signs, symptoms, investigation results.
- Child’s appearance, behaviour or demeanour.
- Interactions between parent/carer and child/young person.
- Concerns from parents/carers.
- Previous or current safeguarding concerns.
- Any known additional vulnerabilities in the child e.g. disability, the child is a ‘looked after child’.
- Information you hold about the family already e.g. parental/carer history, mental health, substance misuse, domestic abuse.
Carry out any appropriate examinations. In cases where there is a concern about non-accidental injuries (NAI), carry out a full body examination. The purpose of examination in these situations in general practice is to try and get a clear picture of what is happening/might have happened to the child and to ascertain the current health and wellbeing of the child in order to take appropriate action.
Note that child protection or forensic medicals should not be carried out by GPs or any general practice clinician in a general practice setting.
Step 2: Ask.
Seek an explanation for any injury, presentation, or concern from both the parent or carer and the child/young person (if possible dependent on age, communication needs, disabilities). For example, if you are concerned that a child has not been brought to multiple health appointments in general practice, you should speak to the parent/carer to discuss your concerns and try to ascertain why this is happening.
Step 3: Consider, suspect or exclude.
- Consider – child abuse is one possible explanation for the concerns and is included in your differential diagnosis.
- Suspect – you have a serious level of concern about the possibility of child abuse (you do not need to have proof).
- Exclude – a suitable explanation is found for your concern.
Step 4: Act.
- If you suspect child abuse, you should follow your local multi-agency safeguarding processes and make a safeguarding referral to children’s social care (Health and Social Care Trust in Northern Ireland).
- If you are considering child abuse, you should decide on what further action needs to be taken:
- Reconsider what you already know about the child and the family, such as health history, any factors which might make the child more vulnerable to abuse, previous safeguarding concerns, parental/carer history, mental health issues, substance misuse, domestic abuse.
- Consider whether your current concerns add to an already concerning picture.
- Consider additional support for the child and family, e.g. early help services, emotional and wellbeing services for the child.
- Gather collateral information from other colleagues and professionals, e.g. colleagues in the practice who might know the family well, practice safeguarding lead, health visitor/school nurse and other health, social care or early help professionals.
- Discuss your concerns with a more experienced colleague, practice safeguarding lead, safeguarding professionals such as named or designated safeguarding professional or health board safeguarding leads.
- Ensure your concerns are documented clearly in the record.
- Arrange review of the child at a date appropriate to the concern, looking out for repeated presentations of worrying features potentially representing child abuse/neglect.
- As time goes on, if concerns persist even at a low level, consider referral to children’s social services for further assessment of the needs of the child.
- If you have excluded child abuse at this time, you should continue to exercise professional curiosity and be prepared to once again consider or suspect child abuse should the situation change, or new information come to light.
Note for practitioners working in Wales: all practitioners working in Wales need to be aware of the statutory duty to report.
Step 5: Record.
- Ensure clear documentation in the child’s record.
- Record exactly what is observed and from whom and when.
- Record exactly what has been said by the child/adult/parents/carers.
- Record all examination findings.
- Record your concerns.
- Record what actions you are going to take.
- Code appropriately.
- Record in other family member records as appropriate.
- Mark clinical entry ‘not for online access’ (where applicable to the UK nation you work in).
References
- NICE. CG89. Child maltreatment: when to suspect child maltreatment in under 18s. Updated 2017.
Safeguarding in Wales: Statutory duty to report:
There is a duty to report to the local authority, which will be taken to mean a referral to social services who, alongside the police, have statutory powers to investigate suspected abuse or neglect.
A report must be made whenever a practitioner has concerns about a child under the age of 18 years who:
- is experiencing or is at risk of abuse, neglect or other kinds of harm; (for further explanations of harm see Section 3 part 1 on significant harm) and has needs for care and support (whether or not the authority is meeting any of those needs).
If any person has knowledge, concerns or suspicions that a child is suffering, has suffered or is likely to be at risk of harm, it is their responsibility to ensure that the concerns are referred to social services or the police who have statutory duties and powers to make enquiries and intervene when necessary.
References
- Wales Safeguarding Procedures. Children and young people at risk of harm. 2024.
Early help
Early help and early intervention are forms of support aimed at improving outcomes for children or preventing escalating need or risk. Because of this they are also sometimes referred to as prevention or preventative services.
Early help is support for children of all ages, that improves a family’s resilience and outcomes or reduces the chance of a problem getting worse. It is not an individual service, but a system of support delivered by local authorities and their partners working together and taking collective responsibility to provide the right provision in their area.
Some early help is provided through ’universal services’, such as education and health services. They are universal services because they are available to all families, regardless of their needs. Other early help services are coordinated by a local authority and/or their partners to address specific concerns within a family and can be described as targeted early help. Examples of these include parenting support, mental health support, youth services, youth offending teams and housing and employment services.
Early help may be appropriate for children and families who have several needs, or whose circumstances might make them more vulnerable.
Early help is a voluntary approach, requiring the family’s consent to receive support and services offered.
Early help and early intervention services can be provided at any stage in a child or young person's life, from the early years right through to adolescence. Services can be delivered to parents, children, or whole families.
Professionals should be alert to the potential need for early help for a child who:
- is disabled
- has special educational needs (whether or not they have a statutory education, health and care plan - EHCP)
- is a young carer
- is bereaved
- is showing signs of being drawn into anti-social or criminal behaviour, including being affected by gangs and county lines and organised crime groups and/or serious violence, including knife crime
- is frequently missing/goes missing from care or from home
- is at risk of modern slavery, trafficking, sexual and/or criminal exploitation
- is at risk of being radicalised
- is viewing problematic and/or inappropriate online content (for example, linked to violence), or developing inappropriate relationships online
- is in a family circumstance presenting challenges for the child, such as drug and alcohol misuse, adult mental health issues and domestic abuse
- is misusing drugs or alcohol themselves
- is suffering from mental ill health
- has returned home to their family from care
- is a privately fostered child
- has a parent or carer in custody
- is missing education, or persistently absent from school, or not in receipt of full-time education
- has experienced multiple suspensions and is at risk of or has been permanently excluded.
Professionals should also have consideration for specific needs such as family members who may have learning difficulties/disabilities or those whose first language is not English, are care experienced, young parents, fathers or male carers, and parents who identify as LGBTQI+.
What if a family does not consent to an early help assessment?
In these situations, professionals should seek to understand why this is the case so they can provide reassurance to the family about their concerns.
They should ensure the family has understood the consensual nature of support, and range of services available to meet their needs. The professional should consider how the needs of the child could otherwise be met, for example, through provision by universal services that the family already engages with. The family should also be reviewed regularly and if there are indicators that the situation is deteriorating, consideration needs to be given as to whether a safeguarding referral is now indicated.
Professionals then need to consider if there are concerns that a child has suffered, or is likely to suffer, significant harm and therefore they suspect child abuse. If so, a safeguarding referral should be made using the locally agreed multi-agency referral pathways. This does not require consent (under the common law – see Part 5 of the toolkit for further information). If professionals are considering child abuse as a possibility, they should follow step 4 as set out in the five step process of responding to concerns about child abuse in the previous section.
References
- NSPCC. Early help and early intervention. Updated 2023.
- HM Government. Working Together to Safeguard Children 2023. 2023.
Making a child safeguarding referral
The mechanism of referrals to children's social care may vary depending on locality. In some areas, referrals can be made by telephone in the first instance but should be followed up in writing within 24 hours. In other areas, referrals may be made by email or via the local authority website. In some areas, children’s social care, police, health and other services are working together to provide a 'front door' for referrals that may be known as a multi-agency safeguarding hub/team (MASH or MAST). Local authorities may have a proforma for inter-agency referrals; this can act as an aide-memoire and help to ensure that the referral is comprehensive and complete.
You must make a safeguarding referral if you are concerned that a child is at risk of, or is suffering, abuse or neglect. You should follow your local safeguarding referral processes.
Top tips for making a child safeguarding referral and writing safeguarding reports – The five Cs
The ‘five Cs’ are relevant to any referral or report written by general practice for the purpose of safeguarding children. This includes safeguarding/child protection referrals as well as reports for strategy meetings and child protection conferences. It is good practice to share the report with parents/carers (and the child/young person if relevant and appropriate) however this is not always possible within the short timescales required for a statutory report.
Clarity
Be clear about who you are, your role and relationship to the child, the source of your concern, what is fact and what is opinion, and what your concerns are.
Child
Include relevant information about the child’s health, wellbeing, especially any vulnerability factors. Where possible, include the child’s thoughts and feelings about what is happening to them – use their words as much as possible. Information to include (if known):
- Demographics of the child.
- Details of parents, carers, siblings.
- Is the child looked after or adopted?
- Details of nursery/school. Is the child home-schooled? Are there any documented concerns about school attendance?
- Known health issues.
- Known disabilities.
- Medication – consider if these are being requested and taken appropriately.
- Vaccinations – consider if these are up to date or if there are any missing.
- Outstanding general practice health reviews such as annual asthma reviews.
- Involvement of other healthcare providers such as paediatrics or child and adolescent mental health services (CAMHS). Provide details of these services so children’s social care can contact them for information.
- Number of ‘was not brought’ appointments.
- Engagement with health. Consider if health appointments are being attended or not, if appointments are frequently cancelled, if medical advice is being followed.
- If there is lack of engagement with health, what is the potential impact on the child, e.g if not being brought to appointments or following medical advice?
- If the child has been seen in general practice, has the child expressed their view on the current situation? If yes, please give details of what the child has said.
Concerns
Describe and explain your concerns in detail, explaining medical terminology. Be clear about the indicators of abuse that you have observed that have led to your concerns. Be explicit about what harm you believe has happened to the child or is at risk of happening.
Context
Include relevant information that general practice holds about the wider context of the child’s life. Be clear about any additional vulnerability factors that you are aware of, that add to your concern such as parental/carer factors, family/environmental factors, community/societal factors or previous safeguarding concerns.
- Relevant information about parents/carers might include:
- Significant and relevant health issues including any mental health issues.
- Any disabilities.
- Medication – consider if it is being requested and taken appropriately. Also consider any addictive medication or any which would impact on their ability to safely parent their child.
- Alcohol or drug misuse.
- Outstanding general practice health reviews.
- Involvement with other relevant healthcare teams e.g. mental health, drug and alcohol teams.
- Engagement with health. Consider if health appointments are being attended or not, if appointments are frequently cancelled, if medical advice is being followed and what the potential impact is on the adult and on parenting.
- History of experiencing abuse when they were a child.
- Previous and current safeguarding concerns including any domestic abuse.
- Known family situation/dynamics (consider any known family stresses, parental separation/conflict, conflict between parents and young people, significant family events, parent in prison).
- Known vulnerabilities (consider poverty, experience of racism, socio-economic factors, refugee/asylum status, housing instability, social isolation, English not their spoken language).
- Transitional safeguarding: if the child is 15 years or older, consider what needs they have approaching adulthood.
- Known family/carer strengths such as supportive family networks, child being brought to health appointments when needed, parents/carers seeking help and support for their own health needs.
Consent
You should be clear in your referral whether consent has been sought or not and whether the referral has been discussed with the child and/or parents/carers (which is expected practice, unless it is thought that doing so would place the child at additional risk).
The issue of whether information can be shared without consent can often be challenging. Consent can be a complex issue and there can be a lot of misunderstanding amongst all agencies about how it is used. In health, consent needs to be considered under the common law duty of confidentiality. Consent is used in a different way in the common law and in data protection law and it is important to understand the differences and how each should be used. Consent is generally not relied upon as the legal basis for information sharing under data protection law. Part 5 of this toolkit provides further explanation and guidance on this issue. The GMC gives clear guidelines on this issue in their guidance ‘Protecting children and young people: The responsibilities of all doctors’. Some excerpts from this guidance are below, but all doctors should have knowledge of the entirety of this guidance.
“Get advice if you are concerned about the possibility of abuse or neglect, but do not believe that the child or young person is at risk of significant harm.
You must tell an appropriate agency, such as your local authority children’s services, the NSPCC or the police, promptly if you are concerned that a child or young person is at risk of, or is suffering, abuse or neglect unless it is not in their best interests to do so. You do not need to be certain that the child or young person is at risk of significant harm to take this step. If a child or young person is at risk of, or is suffering, abuse or neglect, the possible consequences of not sharing relevant information will, in the overwhelming majority of cases, outweigh any harm that sharing your concerns with an appropriate agency might cause.
Ask for consent to share information unless there is a compelling reason for not doing so. Information can be shared without consent if it is justified in the public interest or required by law. Do not delay disclosing information to obtain consent if that might put children or young people at risk of significant harm. Do not ask for consent if you have already decided to disclose information in the public interest.
Tell your patient what information has been shared, with whom and why, unless doing this would put the child, young person or anyone else at increased risk.
Get advice if you are not sure what information to share, who to share it with or how best to manage any risk associated with sharing information.
You can share confidential information without consent if it is required by law, or directed by a court, or if the benefits to a child or young person that will arise from sharing the information outweigh both the public and the individual’s interest in keeping the information confidential. You must weigh the harm that is likely to arise from not sharing the information against the possible harm, both to the person and to the overall trust between doctors and patients of all ages, arising from releasing that information.
If a child or young person with capacity, or a parent, objects to information being disclosed, you should consider their reasons, and weigh the possible consequences of not sharing the information against the harm that sharing the information might cause. If a child or young person is at risk of, or is suffering, abuse or neglect, it will usually be in their best interests to share information with the appropriate agency.”
Working with parents and carers when there are safeguarding concerns about their children/the children they care for
This can feel like one of the most challenging aspects of responding to concerns about abuse, especially when these are about abuse happening within the home and/or by family members.
‘Working Together to Safeguard Children 2023’ outlines principles for working with parents and carers. These are that there should be a child-centred approach with partnership and collaborative working with parents and carers as far as possible, but keeping the wishes and feelings of the child and what is in their best interest central to decision-making. The four principles that should underpin work with parents and carers are:
1. Effective partnership working with parents and carers happens when practitioners build strong, positive, trusting, and co-operative relationships by:
- approaching families and their wider family networks and communities with empathy, respect, compassion, and creativity
- avoiding reinforcing family shame, suffering, and blaming
- using strength-based approaches, working with parents and carers to identify what is working well and how their strengths could support them to effect positive change
- ensuring they work sensitively with parents, carers, and children, to identify and understand the impact of adversity and trauma in their lives; seek to understand how adversity and trauma might manifest and affect children and parents’ engagement and use their expertise to adapt their response with care and compassion
- adapting their responses to meet the diverse needs of parents and carers, including fathers and male carers, and the specific challenges being faced, including parents and carers of disabled children, and where harm is outside the home
- ensuring they understand the families’ background, ethnicity, religion, financial situation, ability, education, sex, ages and sexual orientation, and potential barriers these create in seeking and accessing help and support
- being alert and recognising where parents or carers may not be acting in the best interest of the child or where children may be experiencing abuse, neglect, and exploitation as a result of actions by parents, carers, or other individuals in their lives; practitioners use their skills and expertise to adapt their response to secure engagement
- being mindful of negative stereotypes when making decisions which might lead to false assumptions.
2. Verbal and non-verbal communication should be respectful, non-blaming, clear, inclusive, and adapted to parents and carers needs. Practitioners should ensure that all materials provided to children, parents, carers, and families are jargon free, developmentally appropriate and in a format that is easily understood. Where appropriate, material provided to children, parents, carers, and families should be made accessible and translated into their first language if necessary. Professional interpreters should be provided where needed. Practitioners should not need to rely on family members or partners for interpretation services, including British Sign Language.
3. Practitioners empower parents and carers to participate in decision-making to help, support and protect children by:
- creating a culture of ‘no surprises’, for example, making parents and carers aware of who will attend meetings and discussions, if the child will be invited to participate and the format of the meeting or discussion
- explaining that parents and carers can bring a family member, a friend or supporter to meetings
- giving parents and carers adequate preparation at every stage, relevant information, a safe and appropriate environment for participation and suitable access arrangements
- signposting parents and carers to sources of help and support available locally or through the local authority
- helping parents and carers to understand what the issues are and how these impact on the child, what decisions could be made, what changes need to be made, why and how, timescales and possible outcomes.
4. Practitioners involve parents, carers, families, and local communities in designing processes that affect them, including those focused on safeguarding children. They value their contributions, expertise and knowledge reflecting them in service design and continuously seek feedback from parents, carers, family networks, children, and local communities to inform service improvements. Practitioners use feedback from parents and carers to reflect on their own practice.
The GMC has a resource for parents which explains why doctors who are concerned that a child or young person is at risk of abuse or neglect, must take steps to ensure the child or young person is protected: GMC leaflet: What to expect if your doctor is worried about your child’s safety.
Child protection systems in the UK
Each of the four nations in the UK has their own child protection system and laws to protect children from abuse and neglect. The NSPCC provide up-to-date information on each nation's laws, guidance, frameworks and practice.
What happens after a child protection/safeguarding referral has been made?
The referral will be reviewed often by a multi-agency team with representatives from social care, police and health – sometimes called multi-agency safeguarding team (MAST) or multi-agency safeguarding hub (MASH).
Across the devolved nations, there are different arrangements to investigate concerns about a child and assess the risk of harm.
Depending on the information in the referral, the next steps might be:
- Emergency action if the child is thought to be at immediate danger.
- Other agencies and professionals contacted for further information.
- If initial assessments suggest the child is at risk of significant harm, child protection procedures may commence which can include urgent gathering of information from other agencies, holding strategy meetings where professionals meet to share information and discuss concerns and arrange for a child protection case conference to be held.
- If initial assessments conclude that the child is not in immediate danger or at risk of significant harm, children’s social care and other agencies may offer other help and support such as Early Help services, family support workers, single agency-based support such as through school or the health visitor. These services all depend on parental consent.
- Close the referral without any further action.
If initial multi-agency assessments suggest that a child is at risk of significant harm, child protection procedures may commence which can include urgent gathering of information from other agencies, holding strategy meetings where professionals meet to share information and discuss concerns and arrange for a child protection case conference to be held.
A child protection case conference brings together family members (and the child/children where appropriate), supporters/advocates and those professionals most involved with the child and family to make decisions about the child's future safety, health and development.
The purpose of a child protection case conference is to:
- bring together information about the child and parents from multi-agency partners
- analyse parents’/carers’ capacity to respond to the child’s needs, ensure the child’s safety and promote the child’s health and development
- consider the family history, strengths, network, present and past family functioning to decide if the child is at risk of significant harm
- recommend what action is needed to safeguard and promote the welfare of the child, including the child becoming a subject of a child protection plan
- appoint a lead social worker and identify a core group of professionals and family members to develop, implement and review the progress of the child protection plan
- put contingency plans in place.
Conferences can also be held when the risk to the child is outside the family, e.g. child sexual exploitation/child criminal exploitation.
An initial child protection conference is convened when a child is suspected to be, or likely to be, suffering significant harm. At this meeting, professionals have to decide whether the child is, or is likely to be, suffering significant harm and if so, the child is placed on a child protection plan/child protection register. This multi-agency decision is based on the multi-agency information shared, along with the family and child’s views.
A review child protection conference (three months after the initial child protection conference and then six monthly thereafter) reviews the risk and developmental progress against the child protection plan outcomes.
Police, health and social care representatives attend, along with other professionals involved with the child or family. Health representatives can include health visitors, midwives, school nurses, paediatricians, mental health professionals, and GPs. Other professionals can include education, family support workers, support workers for the child/young person, youth justice workers and drug and alcohol teams. There may also be legal representatives for the family or social care.
What is the role of professionals in a child protection conference?
- Professionals who attend are usually senior within their organisation and/or are directly involved with the family.
- There are no passive roles – each professional who attends must actively engage, give opinions and be involved in the decision-making process.
- Professionals in attendance need to be able to respectfully challenge views.
- The role of the GP is to explain and interpret health information the implications for child’s safety and wellbeing. It is also, along with all the other professionals present, to analyse and assess risk to the child in light of all the information presented.
What happens at a child protection case conference?
- All reports from professionals are available to everyone present including parents/carers.
- Information will be shared, usually by the lead social worker, on what the concerns are, what harm to the child has already occurred or is likely to happen.
- Each professional will be asked to share their views on the strengths of the family as well as the risks and worries.
- Parents are given the opportunity to share their views and question professionals.
- The conference will focus on the child’s circumstances and what they mean for the child’s lived experience. In circumstances where the concerns are about harm within the home, the conference will ascertain whether parents/carers understand this and what needs to change.
- Professionals are asked to decide whether they think significant harm has occurred, or is likely to occur, to the child and whether the child should be on a child protection plan (England) or added to a child protection register (Northern Ireland, Scotland and Wales) and if so, under what category (physical abuse, emotional abuse, sexual abuse, neglect).
- A plan is then drawn up of next steps, what needs to happen to keep the child safe and which professional/agency is taking responsibility for each action. For general practice this may include arranging appointments at the practice for any outstanding health reviews or to address any physical and mental health needs for the child or parents/carers.
- The aim of a child protection plan is:
- ensure the child is safe from harm (including inside and outside of the home, and online) and prevent them from suffering further harm
- promote the child’s health and development
- support the parents, family, and the family network to safeguard and promote the welfare of the child
- set out the support and resources to be provided by each agency to safeguard and promote the welfare of the child.
Child protection conference reports
- General practice will be asked to provide a report on the child and parents/carers for all child protection conferences. General practice has specific and relevant knowledge relating to children and families in their care which is integral to the overall multi-agency assessment. Information that general practice has no concerns about a family is as important to the conference as a long list of concerns about a family.
- It is good practice the report is shared with the parents/carers prior to the conference. This can however be challenging for initial child protection conferences due to the very tight timescales involved.
- If you have concerns that the information you need to share is not suitable to be shared with all individuals at the conference due to its highly sensitive nature, discuss this with the chair of the conference prior to the conference.
- It may be that some information will only be shared with key partners, and not wider family members who may be present. For example, GP records about a parent containing a report detailing the parent’s forensic sexual offending behaviour as a teenager: this is likely to be very relevant information to ensure the safety of the child involved, however is too sensitive to share with everyone at the conference, which may include wider family members. This should be discussed with the chair of the conference. A possible solution would be that a very brief statement or summary about the concern is put into the conference report that is seen by everyone, but a more detailed summary ,or the report in full, is provided to the chair of the conference and the social worker.
- Other examples could include a parent’s HIV positive status or transgender status. In these examples, discussion should take place with the parent themselves to ascertain whether they are happy for this information to be shared (depending on the situation, it may not be relevant for this information to be shared). If the parent does not wish this information to be shared but the clinician believes it is relevant, proportionate and necessary, they should discuss this with the parent and also have a discussion with the chair of the conference and the social worker about limiting the sharing of the information.
What does the GMC say about participating in child protection procedures
- If you are asked to take part in child protection procedures, you must co-operate fully. This should include going to child protection conferences, strategy meetings and case reviews to provide information and give your opinion. You may be able to make a contribution, even if you have no specific concerns (for example, GPs are sometimes able to share unique insights into a child or young person’s family).
- If meetings are called at short notice or at inconvenient times, you should still try to go. If this is not possible, you must try to provide relevant information about the child or young person and their family to the meeting through a telephone or video conference, in a written report or by discussing the information with another professional (for example the health visitor), so they can give a verbal report at the meeting.
Part 3C: Responding to concerns about adult abuse
Responding to concerns about adult abuse can seem complex and challenging, but it is a key part of the holistic care we give our patients. It is a privilege to be able to work alongside our most vulnerable patients to empower and support them, be their advocate and play our part in protecting the basic human rights of all in our communities, particularly those who are unable to protect themselves from harm.
The complexity of adult safeguarding can be summed up in the Department of Health & Social Care ‘Care and support statutory guidance’ (updated October 2023):
“Safeguarding means protecting an adult’s right to live in safety, free from abuse and neglect. It is about people and organisations working together to prevent and stop both the risks and experience of abuse or neglect, while at the same time making sure that the adult’s wellbeing is promoted including, where appropriate, having regard to their views, wishes, feelings and beliefs in deciding on any action. This must recognise that adults sometimes have complex interpersonal relationships and may be ambivalent, unclear or unrealistic about their personal circumstances.”
There are a number of issues to consider when responding to concerns about adult abuse – refer to the following pages for guidance.
1. Concern about abuse
There are lots of different types of adult abuse, as described in the ‘Identification of abuse and neglect’ section of this toolkit. As with child abuse, concerns about adult abuse can emerge over time or not be particularly clear. There can be more than one type of abuse occurring at the same time. There can also be situations where it is unclear who is the perpetrator of abuse and who is the victim of abuse. In addition, a victim of abuse can also perpetrate abuse towards others.
Knowing the indicators of all the different types of abuse as well as using our professional curiosity to find out what life is like for any adult where there are concerns about abuse, is vital to supporting and protecting adults at risk of harm.
If you are unsure whether an adult is experiencing, or at risk of experiencing, abuse, talk to others within the healthcare team who may know the adult better and/or be able to provide another piece of the safeguarding jigsaw. You can also have a discussion with your organisational safeguarding lead or your local safeguarding professionals.
2. The views of the adult
The views and wishes of the adult are essential to any adult safeguarding process which should be transparent and collaborative. The adult should be asked:
- What are their views on what is happening in their life?
- What changes would they like to see?
- What would make a difference to their situation?
- Who would they like to support them?
- What would they like you to support them with?
If the adult is unable to express their views, e.g. due to severe dementia or profound learning disability, then the views of another appropriate person should be sought. The ‘appropriate person’ will vary depending on the situation but may be family, carers, Power of Attorney or an Independent Mental Capacity Advocate (IMCA).
3. Is the adult an ‘adult at risk of harm’?
Central to adult safeguarding legislation and policy across the UK is the concept of whether an adult is ‘an adult at risk of harm/adult in need of protection’ (in some legislation and policy, ‘adult at risk’ is used instead).
The first step in determining whether an adult is ‘an adult at risk of harm/adult in need of protection’ is understanding whether the adult is at risk of, or is currently, experiencing abuse.
The second step is understanding whether the adult has additional needs/care and support needs. These are personal or life circumstances which may be permanent, transitional or fluctuate over time. ‘Care and support’ and other similar terms are used to describe the help some adults need to live as well as possible with any illness or disability they may have The help needed can be practical, financial or emotional or can be a mixture of all three.
Examples of care and support needs are:
- physical disability
- learning disability
- mental health needs
- physical health needs
- long or short term illness
- alcohol or substances misuse/dependence
- elderly frail.
The third step is to understand whether the adult with care and support needs is able to protect themselves from abuse, due to their care and support needs. This includes being able to protect their own wellbeing, property, assets, rights or other interests.
Only adults at risk of harm/adults in need of protection are eligible for consideration of adult safeguarding referrals following local multi-agency processes.
Definition of an adult at risk of harm/adult in need of protection
Someone is considered an adult at risk of harm/adult in need of protection if they meet all of the following criteria:
- Aged 18 years and over in England, Wales and Northern Ireland, or 16 years and over in Scotland.
- Is at risk of, or is currently experiencing abuse.
- Has care and support needs.
- Is unable to protect themselves from harm due to their care and support needs.
Of course there can be adults who are experiencing abuse who are not adults at risk of harm/adults in need of protection. An example of this is an adult with no care and support needs who is experiencing domestic abuse in their relationship. In this situation, and any situation where an adult is experiencing abuse but is not an ‘adult at risk of harm’, there is still a lot of help and support that can be given even though an adult safeguarding referral is not indicated. Examples of support that can be given include:
- consideration of what help and support the adult currently needs and wishes
- signposting to local support agencies such as domestic abuse agencies
- provision of general practice care, or appropriate secondary care referrals, for any physical or mental health difficulties
- consideration given to any others who might be at risk in this situation such as children or ‘adults at risk of harm’. Safeguarding referrals may be necessary to protect others
- consideration given to other agency involvement such as referral to MARAC (if there are concerns about high risk domestic abuse (see section on domestic abuse for further information)
- continue to monitor the situation as risk can change over time, as can the adult’s ability to protect themselves.
It is important to understand, however, that just because an individual is not eligible for a safeguarding response under safeguarding legislation, there are always ways to support people.
4. Assessing mental capacity
Mental capacity is about being able to make your own decisions. It is decision and time specific therefore statements such as ‘an individual lacks capacity’ is, in law, meaningless.
Issues around capacity in adult safeguarding often cause the most challenges for all professionals involved, especially in situations where capacity fluctuates, where there is alcohol or substance addiction, where there is self-neglect and in situations where there are concerns about coercion. Central to adult safeguarding is the rights of adults and mental capacity legislation underpins these rights.
Each of the UK nations have legislation on mental capacity and you should be familiar with the relevant legislation for the UK nation you work in.
IMPORTANT TO NOTE: This section of the RCGP Safeguarding toolkit is intended as a guide only and gives a summary of the principles of mental capacity and issues to be aware of. It is not intended to replace legal or safeguarding advice which should be sought from the relevant professionals/agencies when necessary.
Mental Capacity legislation in the UK:
- The Mental Capacity Act 2005 applies in England and Wales.
- Adults with Incapacity (Scotland) Act 2000 applies in Scotland.
- Mental Capacity Act (Northern Ireland) 2016 is being implemented in stages in Northern Ireland.
- All mental capacity legislation applies to people aged 16 years and over.
The following GMC documents outline the core principles of mental capacity:
Summary of mental capacity principles
The principles of mental capacity are:
- Presumption of capacity.
You must start with the presumption that every adult has capacity to make decisions. A person has capacity if they can do all the following:- understand information relevant to the decision in question
- retain that information – if information can be retained long enough for the individual to make a decision, then that is sufficient, even if this is only for a short period of time
- use the information to make their decision
- communicate a decision.
- Individuals being supported to make their own decisions.
Individuals should be given all practicable steps to help them make a decision. This includes considering:- method of communication that the individual is most familiar with
- best time of day and best location for the individual
- whether it would be helpful to have another person present, taking into account whether the individual has expressed a wish to a particular person to be, or not to be, present
- what the individual requires to learn about and understand the information relevant to the decision
- Whether it is it possible to complete the assessment in one go, or is it necessary to come back and see the individual on more than one occasion whether something can be done which might mean the individual would be able to make the decision (this includes helping the individual to understand they can make decisions).
It is important to be clear about the line between supporting a person to make a decision and making a disguised best interests decision. If the support required is, in truth, so integral to the decision-making process that the person is in effect carrying out the instructions of others rather than (for instance) responding to prompts, then it is likely that what is going on is best interests decision-making, and should be recognised as such.
- Unwise decisions.
Individuals cannot be treated as unable to make a decision for themselves purely because they make an unwise decision.- An individual may not agree with the advice of professionals, but that does not mean they lack capacity to make a decision.
- Each individual will have their own values and outlook which may be very different to our own or others’. It is important to seek to understand the individual’s values and life story as it relates to the decision in question.
- Best interests. Anything done for or on behalf of a person who lacks mental capacity must be done in their best interests.
- Least restrictive option. Someone making a decision or acting on behalf of a person who lacks capacity must consider whether it is possible to decide or act in a way that would interfere less with the person’s rights and freedoms of action, or whether there is a need to decide or act at all. Any intervention should be weighed up in the particular circumstances of the case.
Assessing capacity
A capacity assessment is, in many ways, an attempt to have a real conversation with the person on their own terms and applying their own value system.
The very act of deciding to carry out a capacity assessment is not, itself, neutral, and the assessment process can often be (and be seen to be) intrusive. You must always have grounds to consider that one is necessary. Conversely, you must also be prepared to justify a decision not to carry out an assessment where there appeared to be a proper reason to consider that the person could not take the relevant decision.
Whilst the presumption of capacity is a founding principle, you should not hide behind it to avoid responsibility for a vulnerable individual. The more serious the issue, the more one should document the risks that have been discussed with the individual and the reasons why it is considered that they are able and willing to take those risks.
Steps to follow in assessing capacity:
- Define what the specific decision is and what question needs to be answered. Ensure this precise question is asked of the individual during the assessment.
- Identify the information relevant to the particular decision. This includes the reasonably foreseeable consequences of deciding one way or another, or failing to make the decision. Those reasonably foreseeable consequences can include not just the consequences for the individual, but also, where relevant, the consequences for others.
- If the decision could have serious or grave consequences, you must test whether the individual can understand, retain, use and weigh those consequences.
- Take all practical steps to help the individual before concluding that they are unable to make a decision (see section above on Individuals being supported to make their own decisions).
Lacking capacity
A reminder that a person lacks capacity if (at the time the specific decision has to be made), they are unable to make the decision in question because of an impairment of, or disturbance in the functioning of, the mind or brain.
Decisional capacity and executive capacity
There are two elements involved in capacity: decisional capacity and executive capacity.
- Decisional capacity is the ability to understand and reason through the elements of a decision in the abstract.
- Executional capacity is the ability to realise when a decision needs to be put into practice and execute it at the appropriate moment – the ‘knowing/doing association’. It is the planning initiation, organisation, self-awareness and execution of tasks.
In adult safeguarding, both of these elements are really important:
- Attention should be paid to whether a person has clear decisional and executional ability (i.e. to both make and action decisions) to safeguard themselves in the specific context.
- In all circumstances, it should be considered that even where a person can make a decision, are they able to action that decision to safeguard themselves?
Factors that can impact executive functioning
Executive functioning and self-regulation depend on three types of brain function: working memory, mental flexibility, and self-control. These functions are highly interrelated, and the successful application of executive function skills requires them to operate in coordination with each other.
Each type of executive function skill draws on elements of the others.
- Working memory governs our ability to retain and manipulate distinct pieces of information over short periods of time.
- Mental flexibility helps us to sustain or shift attention in response to different demands or to apply different rules in different settings.
- Self-control enables us to set priorities and resist impulsive actions or responses.
Harvard University, Center on the Developing Child, goes on to outline that children aren’t born with these skills—they are born with the potential to develop them. Some children may need more support than others to develop these skills. In other situations, if children do not get what they need from their relationships with adults and the conditions in their environments—or (worse) if those influences are sources of toxic stress—their skill development can be seriously delayed or impaired. Adverse environments resulting from neglect, abuse, and/or violence may expose children to toxic stress, which can disrupt brain architecture and impair the development of executive function.
Executive functioning can be further broken down into different elements. These are needed by individuals to make appropriate decisions, employ problem solving abilities and have the ability to carry out their own wishes and decisions. Disruption of any of these functions can result in difficulties in all these areas.

There are a number of factors which can impact executive function. Ellie Atkins’ (Aspiring practitioner academic with NHS Research & Development Northwest & Adult Social Care: Complex needs services, Manchester City Council), research paper ‘Opening the door for people with hidden disabilities and differences’, highlights the hidden disabilities and differences that are often undiagnosed but can impact on executive function:
- Childhood trauma, complex trauma.
- Post-traumatic stress disorder.
- Neurogenetic conditions (e.g. Fragile X).
- Neurodevelopmental conditions.
- Foetal alcohol spectrum conditions.
- Neurodivergence.
- Acquired brain injury.
- Traumatic brain injury.
- Epilepsy.
- Stroke.
- Alcohol-related brain damage.
- Mental health conditions.
Atkins found that “understanding people’s life stories was critical to developing a deeper understanding of how people present”.
It is therefore of great importance that when we are assessing capacity, especially executive capacity, we are always mindful of these possible hidden disabilities and differences and use our professional curiosity to try to understand the reasons for behaviours in others that we can’t make sense of.
Unwilling to safeguard or unable to safeguard?
The Adult Support and Protection (Scotland) Act 2007: Code of Practice, outlines one of the key challenges in safeguarding which is being able to distinguish between an adult who is unable to safeguard themselves and an adult who is unwilling to safeguard themselves. In practice, this distinction can be very difficult to make and requires careful consideration. The Code of Practice explains this further:
“All adults who have capacity have the right to make their own choices about their lives and these choices should be respected if they are made freely. However, for many people the effects of trauma and/or adverse childhood experiences may impact upon both their ability to make and action decisions, and the type of choices they appear to make. In this context it is reasonable to envisage situations in which these experiences, and the cumulative impact of them through life, may very well have rendered some people effectively unable, through reliable decision making or action, to safeguard themselves.
Similar considerations apply to coercive control or undue pressure. In such situations the control exercised over a vulnerable person may also effectively render them unable to take or action decisions that would protect them from harm.
It is therefore important, as part of any capacity assessment, to understand the person's decision-making processes. This should include an understanding of any factors which may have impacted upon them with the effect of impinging on, or detracting from, their ability to make and action free and informed decisions to safeguard themselves. This could therefore mean that in these circumstances they should be regarded as unable to safeguard themselves.
Other circumstances can impact on the extent to which a person is meaningfully able to safeguard themselves. Refusing to give a random stranger money is, for example, very far removed from the situation where it is the person's relative who is making such a request, and where the adult is dependent upon that relative for support. For fear of repercussions or removal of support, they may feel afraid of refusing the request.
It is also important to bear in mind that an inability to safeguard oneself is not the same as an adult lacking mental capacity. For example, a person may have relevant mental capacity, but also have physical limitations that restrict their ability to implement actions to safeguard themselves. Capacity applies to both decision-making and the implementation of decisions. A person can have the capacity to make a particular decision but, through illness or infirmity, may not have the physical capacity to implement that decision.”
Practitioners must therefore take a person’s overall circumstance into account, and take great care, before determining whether or not an adult is genuinely able to take and implement decisions about safeguarding themselves.
Assessing capacity in complex situations
As already outlined above, assessment of capacity can at times be challenging and complex. For example, in situations where:
- there is self-neglect
- capacity fluctuates
- there is alcohol or drug misuse
- there is homelessness, especially multiple exclusion homelessness (see section on homelessness)
- there are concerns about coercion, for example in the context of domestic abuse, modern slavery or trafficking, or criminal and sexual exploitation
- there is a history of trauma (past or present) and/or adverse childhood experiences.
In these circumstances, there may be a number of different decisions that GPs and general practice clinicians my be faced with assessing capacity about such as:
- decisions about health issues including treatments
- decisions about referral to, and involvement of, other health professionals and teams such as mental health teams
- decisions about referral to, and involvement of, other agencies such as social care (Health and Social Care Trusts in Northern Ireland)
- decisions about making an adult safeguarding referral where it is established that the adult is an ‘adult at risk of harm’.
Below are some useful steps to consider in these situations in addition to following the mental capacity principles:
Ask for help – that could be from a more experienced colleague, the safeguarding lead in your organisation, safeguarding professionals within your ICB/health authority or similar.
- What is this person’s back story? What circumstances/life experiences have led to the current situation?
- Is there a history of trauma?
- Could this person have a hidden disability?
- Could there be factors influencing executive function?
- Is there any coercion?
- Is there alcohol or drug misuse?
- Does the individual know that they can make a choice and make decisions? (Individuals may feel powerless due to previous experiences.)
- What does the individual understand their choices to be? What are their actual choices?
- What does this individual understand about ‘safeguarding’? Remember some adults’ view of ‘safeguarding’ may be rooted in childhood experiences which may be very negative. It is important to explain the personalised approach of adult safeguarding and also understand that the individual may be very distrustful of professionals.
- ‘Real world’ evidence – do the individual’s actions back up their decisions?
Consider the individual’s decision making process - how and why have they come to their decisions?
Consider information from others who know the individual - this could be other professionals, support workers, carers, or family/friends as appropriate.
Assessing capacity in self-neglect
Assessing capacity in self-neglect is complex. A study from The University of Bristol on Mental Capacity, Self-Neglect, and Adult Safeguarding Practices: Evidence Synthesis and Agenda for Change explored what Safeguarding Adult Reviews (SARs) can tell us about how to improve adult safeguarding in England, with a focus on mental capacity and self-neglect. The key findings are relevant to all practice across the UK:
-
People experiencing self-neglect are more at risk if professionals fail to assess mental capacity.
- Misinterpretation of the Mental Capacity Act 2005 led to mental capacity assessments not being carried out, even when professionals observed concerning events, such as service-users disengaging with service provision, making significant unwise decisions, and/or having diagnoses which may have impacted upon their decision-making.
- Mental capacity assessments were often not recorded in writing and often lacked detail and clarity about who carried out the assessment and its outcome.
-
Safeguarding processes failed to protect people with capacity.
- Professionals sometimes used capacity to justify not intervening in cases of probable self-neglect, therefore leaving people at considerable risk.
- Promoting autonomy and supporting protection should not be mutually exclusive but balanced to best serve people experiencing self-neglect.
-
Assessments lacked nuance and scope.
- Professionals appeared to have given little consideration to long-term impacts of trauma on cognition, interpersonal relationships, and people feeling overwhelmed in moments of crisis, and the possible implications for mental capacity.
- Consideration of the long-term impacts of substance misuse and addiction on decision-making was limited.
- Assessments lacked a thorough consideration of executive capacity.
- Self-neglect may develop through a series of ‘non-decisions’. Simplistic notions of capacity and choice may have limited applicability where people are reproducing the only lifestyle they know. People may be encouraged or discouraged from accepting support because of features of their relationships with professionals. Professionals may empower individuals by informing them of a variety of appropriate options for meeting their self-care needs, or conversely decrease the person’s motivation to engage by failing to offer personalised support.
- Professionals were noted to lack confidence in assessing capacity. In a number of cases some professionals incorrectly believed assessment of capacity not to be their responsibility.
References
- GMC. Mental capacity. 2024.
- 39 Essex Chambers. Mental Capacity Guidance Note: Assessment and Recording of Capacity. 2023.
- 39 Essex Chambers. Mental Capacity guidance note: Relevant information for different categories of decision. 2024.
- 39 Essex Chambers. Mental Capasity Resources.
- Social Care Institute for Excellence. Mental Capacity Act 2005 at a glance. Updated 2022.
- University of Bristol. Mental Capacity, Self-Neglect, and Adult Safeguarding Practices: Evidence Synthesis and Agenda for Change.
- Atkins E. THE CAPACITY TO ACT ……? Opening the door for people with hidden disabilities and differences. 2023.
- Center on the Developing Child, Harvard University. Executive Function & Self-Regulation.
- Local Government Association. Adult safeguarding and homelessness: experience informed practice. 2021.
- Scottish Government. A dult Support and Protection (Scotland) Act 2007: Code of Practice. 2022.
Giving medication covertly
Medication given covertly is medication given without the adult’s knowledge or consent, e.g. hidden in food or drink. Adults should not be given medication covertly unless they have been assessed as lacking the mental capacity to makes decisions about their health or medication.
When a person has mental capacity to make the decision about whether to take a medication, they have the right to refuse that medication. They have this right, even if that refusal appears ill-judged to staff or family members who are caring for them.
Covert administration is only likely to be necessary or appropriate where:
- a person actively refuses their medication and
- that person is assessed not to have the capacity to understand the consequences of their refusal, and
- the medication is deemed essential to the person’s health and wellbeing.
Covert administration must be the least restrictive option after trying all other options. It is important to try and understand why the person is refusing to take their medication.
Organisations, such as care homes, should have a process in place for giving medication covertly. This process should include:
- mental capacity assessment
- best interests meeting
- keeping records
- making a plan
- regular reviews.
There are a number of different people and professionals who may be needed in the decision to give medicines covertly when an adult lacks the capacity to make decisions about their medication:
- care staff
- the prescriber
- the pharmacist
- a lasting power of attorney for health and welfare
- IMCA – Independent Mental Capacity Advocate.
References
5. Is a safeguarding referral needed?
The table below summarises the steps 1 – 4 outlined above and provides guidance on making decisions about adult safeguarding referrals.
- If you are unsure, seek further advice from a colleague, your organisational safeguarding lead or local safeguarding professionals.
- Ensure the patient is safe and deal with any immediate medical needs.
Is the adult an 'adult at risk/adult at risk of harm'?
YES: consider an adult safeguarding referral and follow steps 4 & 5 below.
NO: consider:- other sources of support for the adult
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation if new relevant information comes to light
- continue to monitor the situation as risk and the ability to safeguard themselves may change over time.
Does the adult at risk of harm have capacity to make a decision about a safeguarding referral?
NO: proceed with an adult safeguarding referral.
YES and they consent to a referral: proceed with an adult safeguarding referral.
YES but they do not consent to a referral: consider:- whether they need more information on the safeguarding adult process, which might address any concerns they have
- what other sources of support are available
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation at appropriate intervals as risk can change as can an adult’s ability to protect themselves
- reassess the situation if new relevant information comes to light.
UNCERTAIN: discuss with a colleague, your organisational safeguarding lead or local safeguarding professionals.
NOTE FOR PRACTITIONERS WORKING IN WALES – all practitioners working in Wales should be aware of the statutory ‘duty to report’.
What should happen if an adult at risk of harm has capacity but does not want any safeguarding procedures and is unwilling to take steps to safeguard themselves?
These circumstances can bring high levels of professional anxiety and evoke feelings of helplessness. Here are some principles about managing these difficult situations.
- What does the adult want? Are there small actions that can be taken which might help the adult whilst also building trust in professionals?
- Reconsider if the adult is actually unable to safeguard themselves due the effects of trauma and/or adverse childhood experiences or coercion, rather than being unwilling. A referral can be done without consent, under these circumstances.
- Consider if there are others who are at risk of harm such as children or other adults and take safeguarding action as necessary.
- Are there other professionals already involved with the adult who you can discuss concerns with?
- Keep reassessing the situation – risk can be fluid and dynamic.
- Keep the door open – let the adult know they can change their mind at any time. Also let them know that you are still here to support and help them, regardless of any decisions they make.
- You are never alone in these situations – seek advice and support from your colleagues, your organisational safeguarding lead or your local adult safeguarding team. You can ask for advice without disclosing the name of the patient.
- Some areas have a MARAM process (Multi-Agency Risk Assessment and Management). This is a multi-agency approach to reduce risk in areas such as fire safety, alcohol/drug dependence, non-compliance or challenging behaviour, self-neglect, hoarding, failure to engage with services.
- If you believe the adult is at risk of serious harm you should always seek urgent advice if you are unsure what to do. Consider if a safeguarding referral would be justified in the wider public interest. The GMC advises: “You may be able to justify disclosing information without consent, where it is necessary to prevent a serious crime such as murder, manslaughter or serious assault or there is clear evidence of an imminent risk of serious harm to the individual and no alternative (and less intrusive) methods of preventing that harm. This is an uncertain area of law and, if you can, you should seek independent legal advice before making such a disclosure without consent.”
Wales Safeguarding Procedures: the statutory duty to report an adult at risk of abuse and/or neglect
A duty to report to the local authority will be taken to mean a referral to social services who, alongside the police, have statutory powers to investigate suspected abuse or neglect.
A report should be made whenever there are concerns for an adult at risk who:
- is experiencing or is at risk of abuse or neglect
- has needs for care and support (whether or not the authority is meeting any of those needs) and
- as a result of those needs is unable to protect himself or herself against the abuse or neglect or the risk of it.
(Section 126 of the Social Services and Well-being Act 2014).
The use of the term ‘at risk’ means that actual abuse or neglect does not need to have occurred, rather early interventions to protect an adult at risk of abuse should be considered to prevent actual abuse and neglect.
References
- Wales Safeguarding Procedures. Adults at risk. 2024.
‘Making safeguarding personal’
Making Safeguarding Personal is an approach to adult safeguarding than ensures the focus is on meaningful improvement to an adult’s life. It sits within the Department of Health’s Care and Support Statutory Guidance. It means safeguarding adults:
- is person-led
- is outcome-focused
- engages the person and enhances involvement, choice and control
- improves quality of life, wellbeing and safety.
Safeguarding should be done with patients, not to them. However, patients are likely to be unfamiliar with safeguarding processes. Therefore, you will need to explain what the process is, who will be given information and what information that will be. When an adult safeguarding process starts, there may be several new professionals who want to speak to the patient. This can be very daunting and frightening for patients so informing them of who the professionals may be can be very helpful.
There are six core adult safeguarding principles outlined in The Care Act (England) and the table below outlines what these are and what how they should be experienced by the adults they affect
– the ‘I’ statements:
Making an adult safeguarding referral
The process of making an adult safeguarding referral can vary from place to place. Each local area will have their own agreed multi-agency referral pathway and many local authorities will have their own adult safeguarding referral form that all professionals should use.
It is essential that you are aware how to make an adult safeguarding referral in your area.
If the person you are concerned about is in danger and immediate action is required, you should ring the emergency services on 999.
Top tips for making an adult safeguarding referral and writing safeguarding reports – The five Cs
Clarity
Be clear about who you are, your role and relationship to the adult, the source of your concern, what is fact, what is opinion and what your concerns are.
Care and support needs
Include information about the adult’s care and support needs/personal and/or life characteristics as well as the reasons why the adult is unable to protect themselves from harm, therefore meaning they are an adult at risk of harm. Include relevant information about the adult’s health and wellbeing as well as their views on what is happening to them, what they would like to change and what help and support they would like/need.
Concerns
Describe and explain your concerns in detail – be explicit about what harm you believe has happened to the adult or is at risk of happening. Give as much detail as possible. Explain medical terminology. Highlight if you believe others to be at risk also.
Context
Include relevant information about the wider context of the adult’s life. Be clear about any additional vulnerability factors that add to your concern such as any experience of trauma and/or adverse childhood experiences, evidence of coercion, family/environmental factors, community/societal factors or previous safeguarding concerns. You should also include known personal/family/carer/environmental/community strengths.
Capacity
Be clear about whether the adult has capacity with regards to the safeguarding concerns and referral. Outline any mental capacity assessments that have been carried out and what the outcomes of these are. In addition, be clear whether consent has been given by the adult for the referral. If there is no consent, outline clearly the reasons for making the referral.
Adult safeguarding processes
There are different safeguarding arrangements in each UK nation to make enquiries and carry our investigations if an adult is, or is suspected to be, experiencing, or at risk of experiencing abuse or neglect. These arrangements are often multi-agency.
Adult safeguarding processes should be rights-based, person-centred, empowering, proportionate, collaborative, transparent and include prevention and protection.
Following receipt of an adult safeguarding referral, the local authority (Health and Social Care Trust in Northern Ireland) may first seek further information from safeguarding partners (including general practice) and seek to speak to the adult at risk of harm to ascertain their views.
Adult safeguarding/protection/support and protection/case conferences (terminology varies by nation) may then be convened. These conferences are multi-agency and often include the adult at risk of harm. Agencies may have been asked to prepare a report for the conference. The conferences are generally split into different sections:
- Setting the scene which includes background and summary of concerns.
- Information sharing from agencies.
- Wishes of the adult at risk.
- Outcomes of any investigations and implications for the adult at risk.
- Assessment of abuse and/or neglect including agreeing on severity.
- Decision making and agreement on outcomes which includes which agencies will be involved, whether legal advice is needed, whether any statutory and/or regulatory action is necessary and what plan is needed. There may be specific actions for general practice resulting from an adult safeguarding conference.
Outcomes from an adult safeguarding conference can include:
- No further action – this may happen if there is no further risk of harm or if other support has been put in place that is keeping the adult safe.
- Ongoing Police investigations if a crime has been committed or is suspected of being committed.
- Further discussion with the adult at risk of harm by professionals involved to get to know them and their situation better so that a more in-depth understanding can be gathered about the adult and the risk. This may include capacity assessments.
- Referrals for further specialist input may be required. For example, arranging for a Home Fire Safety Visit if there is substantial hoarding and fire safety is a concern.
- Further adult safeguarding conferences may be held when there is ongoing risk. These conferences enable professionals to continue to share information and assess ongoing risk and support.
In complex adult safeguarding situations such as where there is self-neglect, drug and alcohol addiction, homelessness or concerns about capacity, the adult safeguarding process can continue for many months. In these situations, the GP may be one of the most trusted professionals within the process.
Part 3D: Contributing to the lifelong holistic care of victims and survivors of abuse
Responding to abuse does not start and finish with a safeguarding referral. The impact of abuse can be lifelong regardless of whether it happens as a child or adult or both. There may be ongoing physical and mental health needs that persist for years after abuse has stopped. General practice therefore has an important ongoing role in supporting victims and survivors of abuse. Developing trauma-informed practice is key to providing ongoing support.
Part 3E: Responding to allegations of abuse regarding staff or persons in a position of trust (PiPoT)
The GMC guidance: Raising and acting on concerns about patient safety - professional standards states that:
- You must take prompt action if you think patient safety, dignity or comfort is being compromised.
- In this guidance we explore who the best person or organisation is for you to raise your concerns with. It also covers how to raise your concerns and how you can overcome any barriers that might be preventing you.
- There is also a section on how to handle concerns that are brought to you.
- If you have concerns that a colleague may not be fit to practise and may be putting patients at risk, you must ask for advice from a colleague, your defence body or us. If you are still concerned you must report this, in line with our guidance and your workplace policy, and make a record of the steps you have taken.
Why is this important?
GPs and all practice staff are in a unique and privileged position with access to children, young people and vulnerable adults as well as access to information about them. Whilst the vast, vast majority of staff would never abuse this position of privilege, we have to be alert to the possibility that some might.
Who are ‘persons in a position of trust’?
This term refers to adults who work/volunteer (including students) with children or adults with care and support needs. For example: doctors, teachers, social workers, care workers, faith group leaders, sports coaches.
Concerns can arise when a staff member or a person in a position of trust:
- has behaved in a way that has harmed, or may have harmed an adult or child, possibly committed a criminal offence against, or related to, an adult or child
- behaved towards an adult or child in a way that indicates that they may pose a risk of harm to children or adults with care and support needs.
It is important to note that the concern does not need to be about behaviour towards a child or adult with care and support needs that the adult has contact with within their work/volunteer/student role. For example, an allegation made about a doctor sexually abusing their own children would (along with the standard child protection procedures regarding those children) also need consideration as to whether the doctor may pose a risk to their patients.
In general practice, allegations and concerns about abuse by a person in a position of trust may arise from:
- disclosures from patients
- staff who raise concerns about a colleague
- members of the public who raise concerns about a staff member
- information from other agencies such as the local authority or police or Health and Social Care Trusts (Northern Ireland).
Allegations and concerns of abuse involving persons in a position of trust are complex to manage and may require three different parallel processes:
- safeguarding processes around the child or adult at risk of harm
- police investigations
- employer investigations and procedures.
Each UK nation and each locality will have their own multi-agency processes for managing these allegations. This can include involvement of LADOs (Local Authority Designated Officer) who oversees the response to allegations made about people who work with children or equivalent roles who oversee the response to allegations made about people who work with vulnerable adults/adults at risk of harm.
Any allegations or concerns about abuse by a person in a position of trust must be taken seriously and acted on immediately. Reporting and acting on concerns and allegations does not infer guilt, it ensures that both patients and professionals are protected and supported as needed.
When an allegation or concern raised about a person in a position of trust who is not a member of the general practice team:
- This should be acted on immediately by following the local multi-agency safeguarding processes in place. This may include making a child or adult safeguarding referral depending on the situation.
- If unsure how to proceed, seek advice and guidance as soon as possible from the organisational safeguarding lead and/or your local safeguarding professionals in health or social care.
When an allegation or concern raised about a person in a position of trust who is a member of the general practice team (self-employed, employee, volunteer or student):
- Follow practice/organisational procedures including whistle-blowing policy if necessary.
- The safeguarding lead/practice manager/other relevant senior individual should take the following actions so that safe and proportionate responses are made dependent on the situation and the nature or the concern or allegation:
- seek immediate advice from the LADO or equivalent individual within the local authority/health and social care trust/safeguarding team
- seek immediate advice from the practice HR/employment advisors.
- If there is uncertainty about how to proceed, seek advice from:
- practice/organisational safeguarding lead/practice manager/partner
- safeguarding colleagues such as Named GPs for Safeguarding or Designated Health Professionals
- The professional in local safeguarding board/partnerships who has responsibility for overseeing allegations against those who work with children or adults at risk of harm e.g. the LADO (Local Authority Designated Officer)
- medical defence organisations (MDO)
- regulatory body.
- All GPs should be aware of the GMC guidance: ‘Raising and acting on concerns about patient safety’ and adhere to these professional standards.
- The person about whom the concern/allegation is made should be treated fairly and signposted to support.
Practice procedures
All practices/organisations should have clear policies and processes on disciplinary procedures and managing allegations about staff which includes how the staff member should be supported.
Support for a member of staff under investigation
If an concern/allegation has been raised against you, you should:
- be offered support
- be treated fairly
- seek support (dependent on role) from your union, defence union, your GP, NHS Practitioner Health, BMA, LMC.
Safer recruitment
All practices should follow safe recruitment procedures which includes:
- Disclosure and barring/criminal record checks (via Disclosure and Barring Service [DBS] in England and Wales, via Disclosure Scotland in Scotland or via Access NI in Northern Ireland).
- References.
- Safeguarding included in all job descriptions.
- Obtaining evidence of a person’s right to work in the UK.
These procedures are only one part of safe recruitment and safe staffing.
All staff should be alert to any behaviours of colleagues (inside and outside of work) that could indicate a risk to patients or the wider public.
The practice has a legal duty to refer information to the relevant disclosure service (as outlined above) if an employee has harmed, or poses a risk of harm, to vulnerable groups and where they have dismissed them or are considering dismissal. This includes situations where an employee has resigned before a decision to dismiss them has been made . It also includes situations where the harmful behaviour has taken place outside of work or the organisation only finds out about it after the person has left.
Part 4: Documenting safeguarding concerns and information
This section covers the key principles of documenting safeguarding concerns and information in the patient electronic medical record as well as a list of essential safeguarding codes to ensure a common safeguarding language and understanding across general practice.
Documenting and coding safeguarding information in the electronic medical record
The general practice electronic patient medical record has undergone significant changes in recent years and is ever evolving. In some parts of the UK, patients are now able to access their entire medical record via their phone or computer. In addition, multiple professionals including other health and social care organisations may also access the patient record. There is also an increasing amount of information from other agencies, such as social care, now held within the record. GP IT systems are also increasingly sophisticated. These changes have brought into sharp focus the need for robust, safe management of safeguarding information within the electronic patient record. Safe management includes high quality records that are accurate, unambiguous, timely, accessible and complete, as well as security and confidentiality of records.
Key principles of documenting safeguarding concerns and information in the patient electronic medical record
- High quality documentation of safeguarding information is fundamental to safeguarding children and adults in order to:
- ensure victims and survivors of abuse have the healthcare and support they need
- allow a picture to be built over time of emerging concerns
- manage and share information about risk appropriately
- allow for effective information sharing when required
- allow for discussions with patients about online access where there are safeguarding concerns.
- Experiencing abuse and/or neglect as a child or adult has significant implications on health and wellbeing so therefore needs to be documented.
- Concerns about safeguarding should be documented clearly on all relevant family health records, not just the individual child/adult. Using the appropriate codes (see table below).
- All safeguarding information should be stored within the medical record, not separate to it.
- Any documents containing third party information should be flagged as such with the appropriate code.
- It is not necessary to black out information within safeguarding documents before putting into the patient record.
- The use of coding to record key safeguarding information is important to be able to easily find the relevant information when needed in the future or for audit purposes.
- Safeguarding information should be managed safely to reduce the risk of perpetrators using any disclosures of abuse from victims (or any information in the medical record) to further abuse them.
- If any member of staff is unsure how to manage safeguarding information, they should always seek advice from the practice safeguarding lead/Caldicott guardian/information governance lead/Data Protection Officer.
- All safeguarding information should be redacted from patient online access and clearly marked ‘not for online access’.
Who is responsible for managing safeguarding information in the practice/organisation?
- Everyone has a role to play – clinical, secretarial and administrative staff.
- Each practice/organisation should have robust procedures in place for how safeguarding information is handled.
- Each practice should have a safeguarding administrator who manages or oversees, the recording and coding of safeguarding information coming in and out of the practice.
What is ‘safeguarding information’?
Information about abuse and neglect which can be:
- possible or confirmed
- recent or non-recent (also known as historical)
- about the risk of, or vulnerability to, abuse and neglect
- a wide continuum of safeguarding activity ranging from prevention and early intervention, to risk assessment and management, including investigation and protective intervention.
The information can be held within the record as coded information, free text in consultation records or attached to coded information, records of conversations with other professionals, letters and documents.
Sources of safeguarding information
- From patients themselves, their families or carers.
- From healthcare colleagues.
- From other professionals/agencies such as children and adult social care (Health and Social Care Trusts in Northern Ireland), police, education, and other bodies such as domestic abuse organisations.
- From child protection/adult safeguarding conferences.
- From multi-agency processes such as MARAC (Multi-Agency Risk Assessment Conferences) and MAPPA (Multi-Agency Public Protection Arrangements) or PPANI (Public Protection Arrangements Northern Ireland).
Safeguarding information coming into and out of the practice/organisation can include:
- Information held within letters between healthcare professionals, e.g. within an outpatient paediatric or mental health team letter.
- Invitations to strategy meetings, child Protection conferences, adult safeguarding conferences.
- Strategy meeting minutes.
- Child protection conference reports.
- Adult safeguarding conference reports.
- Child protection medical reports.
- Safeguarding child or adult referrals made by general practice staff.
- Safeguarding information held within records of patients who are new to the practice, which is identified by administrative staff when summarising these records.
- MARAC reports and minutes.
- MAPPA minutes.
- Channel Panel reports and minutes.
- Domestic abuse reports from the police.
It is important to note that these all may contain information about more than one person and should be flagged as containing third party information, as well as redacting from patient online access.
Recording family groups/relationships
Where possible family/household members should be linked on the records. This aids practitioners to ‘Think family’, be able to see ‘the child behind the adult’ and ‘the adult behind the child’ as well as understanding the wider context of an adult’s life when there are safeguarding issues.
Where possible, and if known, details of key individuals should be added to the record. This is particularly important with children – details of parents/carers, who has parental responsibility, and foster carers are all important. Where there are complex family situations, it is important to highlight who has legal parental responsibility.
For adults, details of those with Lasting Power of Attorney can be helpful or people mentioned in advance directives.
Documenting who attends with a patient is also really important.
Domestic abuse
Refer to 'RCGP guidance on recording domestic abuse in the electronic medical record' for information on coding of domestic abuse and MARAC information.
Recording adult drug and alcohol problems, mental health problems and learning disabilities
If you are aware that a parent/carer/household member has a drug/alcohol problem, a learning disability or significant mental health problem it needs to be considered whether that information should be recorded in their children’s records or in the records of any adult with care and support needs within the household to ensure a holistic approach to the needs of the whole family.
This information should always be redacted from patient online access and clearly indicated that it contains third party information.
‘Was not brought'
- Children and many adults with care and support needs need to be brought to health appointments by their caregivers (there are exceptions to this such as teenagers who have made the appointment themselves). Health appointments includes face-to-face, phone and virtual appointments.
- If not brought to an appointment, this should be recorded as ‘not brought’ rather than ‘did not attend/DNA’.
- Not being brought to an appointment can be a sign that the family/carers are struggling in some way or can be an indicator of abuse/neglect.
- Every practice should have a policy in place for how these missed appointments are acted on as well as missed reviews. For example when an adult with a learning disability has had repeated invitations for their annual review but no appointment has been made.
Management of Child Protection conference invitations, reports (including those provided by general practice and those received) and minutes
- These should be added onto ALL the records of the family/household members – there will be some exceptions to this which need to be judged on a case by case basis.
- These should be marked not for online access and that they contain third party information.
- Relevant codes should be added (see table below).
Management of Adult safeguarding conference invitations, reports(including those provided by general practice and those received) and minutes
- These should be added onto the patient record and consideration given as to whether they should be added onto any other patient’s records e.g. family members, children, partners or whether a short summary should be added.
- These should be marked not for online access and that they contain third party information.
- Relevant codes should be added (see tables below).
Contextual Safeguarding situations
Contextual safeguarding recognises that as young people grow and develop, they are influenced by a whole range of environments and people outside of their family. For example in school or college, in the local community, in their peer groups or online. Examples of this includes child sexual exploitation, child criminal exploitation and harmful sexual behaviour. There is often a different multi-agency safeguarding response to these young people when the risk is extra-familial (i.e. outside the family/household) which is not always through a child protection process. The information practices receive about these young people may be significantly less than what is contained within a child protection conference report.
This information should always be redacted from patient online access and marked as containing third party information.
Where there is extra-familial harm to a child, it will not always be appropriate to put all the safeguarding documents and information related to this in the entire family record (if there is no known risk within the family). In these circumstances, it is appropriate to use the code ‘child in family is cause for safeguarding concern’ in all relevant family records with brief free-text about situation.
Information about perpetrators of abuse
This is one of the most complex and challenging areas of recording safeguarding information: should information be recorded in an alleged perpetrator’s medical record?
The RCGP already has guidance on recording and managing information about perpetrators (alleged or confirmed) of domestic abuse.
When considering whether to record information in a perpetrator record (alleged or confirmed), there are a number of issues to balance:
- If perpetrators of abuse become aware that their victim has spoken about the abuse, this could put the victim at increased risk of significant harm.
- ‘Allegations’ are simply that and the alleged perpetrator has no ability to refute the allegations within their own medical record if they are not aware this information has been documented.
- Knowledge about possible perpetrators of abuse may prompt earlier identification of safeguarding issues.
- Knowledge that a patient is displaying abusive or harmful behaviour towards others can help with risk assessments in general practice to ensure everyone’s safety in the practice including staff and other patients’ safety.
- Patient online access brings additional challenges such as the perpetrator becoming aware of information if it had not been redacted from the online record.
When is it appropriate to record information about a perpetrator of abuse in their own medical record?
- If the individual themselves has provided the information about any abusive behaviour or allegations they have faced/are facing.
- When it is clear that the perpetrator is aware of the allegations. For example, information shared from child protection processes such as child protection conferences where the concerns are about abuse within the family by parents/carers who are fully aware of the allegations and concerns of professionals.
- When there are agreed local multi-agency information sharing arrangements in place which take into account:
- the unique challenges general practice face in managing information such as data controllership and patient online access
- the risks and benefits to sharing information about perpetrators when the perpetrator is not aware that information is being requested, or shared, about them.
What if an agency such as MAPPA/PPANI, wishes to share information with general practice about an individual who is a violent or sexual offender and who is a patient at the practice, but the individual is not going to be told that the information is being shared?
- There needs to be absolute clarity in this situation about why the agency wishes to share the information, and why it is without the individual’s knowledge. Questions and factors to consider are:
- Does the individual pose a significant risk to staff in general practice? If so, can the individual be safely managed in a routine general practice setting or does there need to be consideration of the special allocation scheme which is a service for managing violent and abusive patients in general practice ? This could not be done without the individual’s knowledge.
- Does the patient pose a significant risk to others such as the wider public, partners or children? If so, what are the expectations of general practice having this information, e.g. what are they going to do with this information and how are they to use it without the individual’s knowledge?
- Should this information be shared when, for example, a referral is being made to a mental health team or secondary healthcare provider?
- Information shared with general practice stays on a patient’s medical record for life.
- Patient online access.
The RCGP
would like to thank the NNNGP (National Network of Named GPs), Dr
Imran Khan, Dr Ralph Sullivan and Dr Tom Nichols in particular for
their input into this section.
Managing safeguarding information in the context of patient online access
There is already extensive guidance on this in the RCGP GP online services toolkit and practitioners working in areas where there is patient online access should be familiar with all aspects of this toolkit. This toolkit provides specific safeguarding guidance on:
- Coercion – guidance on the impact of coercion to share record access with a third person or failure to maintain the privacy of online record access.
- Safeguarding and automatic record access – guidance on managing safeguarding risks and online record access.
- Safeguarding and vulnerable groups – guidance on how specific groups of vulnerable groups of patients may not be able to manage online record access safely.
In addition, the GP online services toolkit also provides extensive guidance on all the aspects of patient online access including managing potential harmful information, redaction and data quality for online access.
Safeguarding codes
There are now multiple codes that can be utilised for recording safeguarding concerns and information in the electronic medical record, with new codes frequently being developed. There are different clinical IT systems used in general practice across the four UK nations which use different coding systems.
The table below provides a list of essential safeguarding codes. Regular and consistent use of these codes will ensure a common safeguarding language and understanding across general practice.
The relevant code should be recorded in the child’s records as well as relevant family member records.
The relevant code should be recorded in the child’s records as well as relevant family member records.
The relevant code should be recorded in the child’s records as well as relevant family member records.
The relevant code should be recorded in the child’s records. In relevant family record’s a code such as ‘Child in family is safeguarding concern’ should be recorded.
The relevant code should be recorded in the child’s records.
The relevant code should be recorded in the adult’s records. Consideration should also be given as to whether any information needs to be recorded in any other records, such as relevant family members.
(PLEASE ALSO REFER TO THE SEPARATE GUIDANCE ON RECORDING DOMESTIC ABUSE)
This code should be recorded in the patient record and linked to the document.
This code does not have to be placed in the Major/Active Significant Problems.
This code should be recorded in the patient record.
This code should be recorded in the patient record.
Part 5: Information Sharing and multiagency working
This guide to information sharing for the purposes of safeguarding is applicable to all UK nations.
“Good multi-agency work involves taking joint responsibility for finding effective ways of working together, making joint decisions where possible and seeking and providing information.”
—Multi-agency working and information sharing: learning from case reviews NSPCC Learning.
General practice is a vital member of both the child and adult multi-agency safeguarding partnerships. We therefore have a responsibility to ensure that we understand the necessity of information sharing to safeguard children and adults and how we do this effectively.
Issues around information sharing in a safeguarding context, such as lack of information sharing or missed opportunities, are longstanding and come up repeatedly in case reviews which happen when children or adults die, or are seriously harmed, due to abuse or neglect.
This part of the RCGP safeguarding toolkit aims to provide GPs and everyone working in general practice with the knowledge they need to be confident in sharing information for the purposes of safeguarding.
The RCGP would particularly like to thank the Information Commissioner’s Office and the GMC Standards and Ethics team for their input and advice into this part of the toolkit.
Part 3 of this toolkit has detailed guidance on assessing mental capacity in adult safeguarding situations.
Guidance on information sharing
The GMC (General Medical Council), the ICO (Information Commissioner’s Office) and other organisations all provide detailed guidance on information sharing which is set out in Appendix 1. Appendix 1 also contains devolved nation specific guidance.
All doctors should be aware of the relevant GMC guidance in full.
Useful additional tools:
- The GMC have a confidentiality decision tool in their guidance, ‘Confidentiality: good practice in handling patient information’.
- The ICO also have a guidance tool: Lawful basis interactive guidance tool.
What does ‘information sharing’ in a safeguarding context mean?
Sharing information in a safeguarding context means sharing relevant personal information about children and adults that multi-disciplinary and multi-agency professionals and agencies hold. The information is shared in order to safeguard children and adults from abuse and neglect.
Information can be shared in a variety of ways such as: safeguarding referrals, safeguarding reports, letters, emails, clinical IT systems, verbal discussions and multi-agency processes such as multi-agency risk assessment conferences (MARAC), muti-agency public protection arrangements (MAPPA) or public protection arrangements Northern Ireland (PPANI).
Information sharing can range from documenting safeguarding concerns in a patient record, to seeking advice from a practice safeguarding lead, to providing a detailed report for the purposes of a safeguarding conference.
The information that general practice can provide can be very wide-ranging. Further detail on relevant information that general practice can provide can be found in Part 3 of the RCGP safeguarding toolkit in the sections: ‘Top tips for making a child safeguarding referral and writing safeguarding reports’ and ‘Top tips for making an adult safeguarding referral and writing safeguarding reports’.
The challenges of information sharing in general practice
Information sharing in a safeguarding context can give rise to a number of challenges in general practice – some of these are listed in the table below. We have to balance the need for a confidential health service with the responsibilities we have to share information when appropriate to keep children, and adults at risk of harm, safe from abuse and neglect.
These challenges must not prevent appropriate sharing of personal information for the purposes of safeguarding. One of the key ways to overcome many of these challenges is to be confident in your knowledge about safeguarding and information sharing processes. You can be assured that sharing personal information for the purposes of safeguarding is allowed in both the common law and data protection law.
Why do we need to share information?
Organisations need to share information with the right people at the right time for safeguarding purposes to:
- prevent abuse and neglect including serious harm and death
- co-ordinate effective and efficient responses to stop abuse and neglect
- enable early interventions to prevent the escalation of risk
- reveal patterns of abuse that were previously unrecognised and that could identify others at risk of abuse
- identify low-level concerns that may reveal people at risk of abuse
- help people to access the right kind of support to reduce risk and promote wellbeing
- help identify people who may pose a risk to others and, where possible, work to reduce offending behaviour
- reduce organisational risk and protect reputation.
When should we share information?
There are two broad safeguarding-specific scenarios in general practice which will prompt consideration of sharing information:
-
When we in general practice have a concern that a child or adult, has experienced, or is at risk of experiencing, abuse or neglect e.g. seeking advice from a safeguarding professional or making a safeguarding referral.
-
When other professionals or agencies, such as a health visitor or social care, have a safeguarding concern about an adult or child, they share that concern with general practice, and request information from general practice as part of the safeguarding process, e.g. social care request a report for a child protection conference.
There are other scenarios where information sharing is also needed within the broad scope of safeguarding, for example:
- court orders, such as requests for medical records as part of a family court process
- requests for completion of medicals and forms for prospective foster carers/adoptive parents
- requests for information as part of the health assessments for Looked After Children.
What information should we share?
Information shared for the purposes of safeguarding should be:
- clearly identified as either fact or professional opinion
- respectful, remembering that information provided may be seen by the person about whom it is shared
- necessary, relevant, and proportionate. This will vary depending on the situation, what information is being requested and which professional/agency is making the request and why. Part 3 of the toolkit (child, adult) provides further information on information most likely to be relevant to share for the purposes of safeguarding. Entire health records should not be shared (there may be exceptions to this, such as a court order).
Who should we share information with, and how?
- Documenting safeguarding concerns clearly within the medical record. Part 4 of the RCGP Safeguarding toolkit provides further guidance on recording safeguarding concerns in the patient medical record.
- Sharing safeguarding concerns in practice safeguarding meetings.
- Seeking advice from the practice safeguarding lead and/or Caldicott Guardian regarding safeguarding information management issues.
- Sharing safeguarding concerns as relevant in referral letters/communication with other health professionals.
- Proactive sharing of safeguarding concerns as they arise with:
- other health professionals/teams involved in the care of the patient such as midwives, health visitors, mental health teams
- other professionals such as social workers, if they are already involved with the patient.
- Sharing safeguarding concerns with our multi-agency safeguarding partners, e.g. via safeguarding referrals. This is most likely to be with the local authority/social care in England, Scotland and Wales, and with Health and Social Care Trusts in Northern Ireland. Local agreed multi-agency processes should be followed.
- Sharing relevant information as part of multi-agency safeguarding assessments.
- There are other agencies with whom information sharing will be necessary at times. These include education, drug and alcohol teams, care homes, care agencies, domestic abuse agencies and providers of services to those experiencing homelessness.
- These are specific multi-agency processes set up to protect victims of high-risk domestic abuse (MARAC) and to manage the risks posed by those convicted of violent, sexual and terrorism offences who are living in the community, in order to protect the public (MAPPA, PPANI).
- Information sharing with, and from, general practice into these processes varies across different parts of the UK and practitioners should be aware of how these work in their locality.
- Any decisions to disclose personal or confidential patient information to the police must be taken on a case-by-case basis.
- Be aware of, and abide by, the advice on public interest disclosures provided by your professional regulator (GMC: Confidentiality: good practice in handling patient information. Paragraphs 22, 23).
- Know who deals with requests from the police in your organisation, who you can ask for advice, and who should authorise the disclosure of information to the police. Know what to do if these people are unavailable (for example, you are working out of hours). If a decision really cannot wait because someone is at imminent risk of serious harm, use your professional judgement.
- Seek advice from your practice safeguarding lead/Caldicott guardian/information governance lead/data protection officer/medical defence organisations if you are unsure how to proceed.
- Understand that there may be times when it is appropriate to challenge an information sharing request from the police.
- Additional guidance on sharing information with the police: Sharing information with the police. Doctors should also refer to the GMC guidance: Confidentiality: good practice in handling patient information.
- The ICO has a useful toolkit: Can I share personal data with a law enforcement authority, such as the police?
General principles for consideration of information sharing requests from other professionals or agencies for the purposes of safeguarding
- Has the request come from a verified source?
- Has the process for the request followed any locally agreed multi-agency information sharing processes including for requesting personal information from general practice?
- Has sufficient information been provided about the current situation, what the safeguarding concerns are and the current level of risk/harm?
- Has information been provided about consent (under the common law) from the patient/parents/carers/lasting power of attorney (depending on the situation, the patient’s age, competence and capacity) to share their personal information?
- If this consent has not been sought, have the reasons for this been given?
- If this consent has been sought and given, are you confident the patient (or relevant person who has given consent) is aware of what information is contained in the medical record, i.e. what information they have consented to sharing?
- If this consent has been sought but not given, have any of the other conditions for the disclosure of confidential information under the common law been met, i.e. it is required by law, or in response to a court order, or it is justified in the public interest?
Information sharing about perpetrators
This is an area of particular complexity, in particular when the individual is not aware of the allegations being made against them or that they are not aware that other agencies are sharing information about them.
The RCGP has guidance on recording and managing information about perpetrators (alleged or confirmed) of domestic abuse.
There is also additional guidance on this issue in Part 4 of the toolkit: Documenting safeguarding concerns and information.
Information sharing and the law
There are a number of laws and principles that govern information sharing across the four UK nations which include the common law, data protection law (UK GDPR and the Data Protection Act 2018 (DPA 2018)), human rights legislation, and mental capacity legislation. As health and social care laws are devolved to Wales, Scotland and Northern Ireland, practitioners should consider how legislation impacts them in relation to their relevant part of the UK.
Consent
Consent can be a complex issue and there can be a lot of misunderstanding amongst all agencies about how it is used. In health, consent needs to be considered under the common law duty of confidentiality. Consent is used in a different way in the common law and in data protection law and it is important to understand the differences and how each should be used. Consent is generally not relied upon as the legal basis for information sharing under data protection law.
Under the common law duty of confidentiality, consent may be explicit or implied.
- Explicit consent is given when a patient actively agrees, either orally or in writing, to the use or disclosure of information.
- Implied consent refers to circumstances in which it would be reasonable to infer that the patient agrees to the use of the information, even though this has not been directly expressed.
Under data protection law, consent has a different meaning and standard than under the common law duty of confidentiality.
Consent is defined in the UK GDPR as:
-
Any freely given, specific, informed, and unambiguous indication of the data subject’s wishes by which he or she, by a statement or by a clear affirmative action, signifies agreement to the processing of personal data relating to him or her.
Additional ‘conditions’ for consent include the right to withdraw consent easily and at any time.
‘Consent’, as defined in data protection law, is therefore unlikely to be appropriate to use when sharing information for safeguarding purposes and it is not required under data protection law for sharing information in a safeguarding context.
Under the UK GDPR, consent is only one of the legally defined ‘lawful bases’ for handling personal information. A ‘lawful basis’ is a valid reason in data protection law for processing personal information.
In most safeguarding scenarios you will be able to find a more appropriate lawful basis than consent. There are six available, and the most appropriate ones for safeguarding purposes are likely to be public task, legitimate interests, legal obligation and vital interests. Using the right lawful basis means you can share all the information you need to, with an appropriate organisation or individual.
You can be confident that the two differing concepts of consent mean that you may lawfully share information for the purposes of safeguarding without consent as defined under data protection law, while still obtaining consent as defined and prescribed by common law.
It is also important to be aware that consent under the common law is not always necessary to share information for the purposes of safeguarding. As outlined below, there are other legal bases allowed by the common law to share information. These are particularly important in a safeguarding context.
Legal considerations for sharing personal information
Both are equally important and necessary, but need to be considered separately; by doing so you can confidently share personal information that is necessary, proportionate, and relevant, for the purposes of safeguarding.
You can also be assured in the knowledge that you are complying with the common law and data protection law.
Information acquired by doctors in their professional capacity will generally be confidential under the common law. It is generally accepted that the common law allows disclosure of confidential information if:
- the patient consents
- it is required by law, or in response to a court order
- it is justified in the public interest.
“Confidentiality is an important ethical and legal duty, but it is not absolute. You may disclose personal information without breaching duties of confidentiality when any of the following circumstances applies:
- The patient consents, whether implicitly or explicitly for the sake of their own care or for local clinical audit, or explicitly for other purposes.
- The patient has given their explicit consent to disclosure for other purposes.
- The disclosure is of overall benefit to a patient who lacks the capacity to consent.
- The disclosure is required by law, or the disclosure is permitted or has been approved under a statutory process that sets aside the common law duty of confidentiality.
- The disclosure can be justified in the public interest.”
GMC guidance ‘Confidentiality: good practice in handling patient information’ (paragraphs 63 – 70) sets out guidance on disclosing information in the public interest and the principles to follow.
Under UK GDPR, there are six lawful bases for sharing personal information. The most appropriate ones for safeguarding purposes are likely to be public task, legitimate interests, legal obligation, and vital interests.
APPENDIX 1: Information sharing advice and guidance
There is a wealth of information sharing guidance relevant to general practice.
The General Medical Council (GMC) provides detailed guidance on confidentiality and information sharing. All GPs should be fully aware of the relevant guidance in its entirety, in particular:
- GMC. Confidentiality: good practice in handling patient information.
- GMC. Protecting children and young people: the responsibilities of all doctors.
- GMC. 0–18 years: guidance for all doctors.
- GMC. Ethical Hub: Adult safeguarding. Reviewed January 2024. This hub provides resources exploring how to apply the existing guidance in practice - it does not set out new professional standards.
The Information Commissioner’s Office (ICO) provides detailed guidance on UK GDPR (General Data Protection Regulation). In particular:
- ICO. A 10 step guide to sharing information to safeguard children.September 2023.
- ICO. A guide to lawful basis. October 2022.
- ICO. Data sharing: a code of practice. May 2021.
The British Medical Association (BMA) provides guidance also:
- BMA. Adults at risk, confidentiality, and disclosure of information. Updated June 2024.
- BMA. Children and young people toolkit. January 2024.
The UK Caldicott Guardian Council (UKCGC) also provides useful guidance on information sharing and disclosure:
- UKCGC. Information sharing and disclosure.
- UKCGC. Information Sharing in Cases of Domestic Violence and Abuse. Guidance for health and care professionals and other agencies.
- UKCGC. Information/Data Sharing Decision template.
Northern Ireland-specific guidance
- Safeguarding Board for Northern Ireland. Procedures Manual. Updated December 2023.
Scotland-specific guidance
- Scottish Government. NHS Scotland Caldicott Guardians: Principles into Practice. February 2011.
- Scottish Government. Getting it right for every child (GIRFEC) Practice Guidance 4 – Information Sharing.September 2022.
- Scottish Government. Adult Support and Protection (Scotland) Act 2007: Code of Practice. July 2022.
- Scottish Government. Adult Support and Protection (Scotland) Act 2007: guidance for General Practice. July 2022.
- NHS Scotland. Protecting Patients Confidentiality. The Common Law Duty of Confidentiality in practice. July 2023.
Wales-specific guidance
Welsh Government. Wales Accord on the Sharing of Personal Information (WASPI).
References
- GMC. Protecting children and young people: the responsibilities of all doctors.
- GMC. Ethical Hub: Adult safeguarding. Reviewed January 2024.
- BMA. Adults at risk, confidentiality and disclosure of information. Updated June 2024.
- BMA. Children and young people toolkit. Updated June 2024.
- GMC. What to expect if your doctor is worried about your child’s safety. September 2012.
- ICO (Information Commissioner’s Office). A 10 step guide to sharing information to safeguard children. September 2023.
- Department of Education. Working Together to Safeguard Children 2023. February 2024.
- Social Care Institute of Excellence. Safeguarding adults: sharing information. Updated January 2019.
- National Data Guardian for health and social care. The Eight Caldicott Principles. December 2020.
- UKCGC (The United Kingdom Caldicott Guardian Council). Information/Data Sharing Decision template.
- UKCGC. Information sharing and disclosure.
- UKCGC. Information Sharing in Cases of Domestic Violence and Abuse. Guidance for health and care professionals and other agencies.
- NHS England Transformation Directorate. Sharing information with the police. May 2022.
- GMC. Confidentiality: good practice in handling patient information.
- GMC. 0–18 years: guidance for all doctors.
- GMC. Confidentiality: key legislation factsheet.
- Department for Education. Information Sharing. Advice for practitioners providing safeguarding services for children, young people, parents and carers. May 2024.
- Information Commissioner’s Office. A guide to the data protection principles. Updated May 2019.
- NSPCC. Multi-agency working and information sharing: learning from case reviews. April 2024.
Acknowledgements
The RCGP would like to thank the numerous individuals and organisations who have been involved in the development of the RCGP Safeguarding Standards and toolkit including:- Academy of Medical Royal Colleges: Academy Professional Development Committee
- Appraisal teams, 4 UK nations
- Centre of expertise on child sexual abuse
- Child Protection Unit & Adult Protection and Support, Scottish Government
- CQC
- GMC
- GPC
- ICO
- NHSE
- NNNGP
- RCN
- RCPCH
- RCGP Northern Ireland
- RCGP Scotland
- RCGP Wales
- RCGP Clinical Policy team
- RCGP CPD Events team
- RCGP eLearning team
- RCGP Professional Standards team
Date of publication: 3 October 2024