Acute Kidney Injury toolkit
| Site: | Royal College of General Practitioners - Online Learning Environment |
| Course: | Clinical toolkits |
| Book: | Acute Kidney Injury toolkit |
| Printed by: | Guest user |
| Date: | Saturday, 26 April 2025, 5:56 AM |
Description
We have developed this toolkit to disseminate learning highlighted from AKI case notes reviews, part of the RCGP AKI Quality Improvement project.
Table of contents
- Introduction
- Kidney Health and AKI: Information for patients, carers, and healthcare staff
- AKI: Recognition and response
- Post-AKI Care: Primary care management after an episode of AKI
- Embedding holistic post-AKI care planning into routine practice
- AKI and Quality Improvement
- Further resources and references
Introduction
Targeting Acute Kidney Injury (AKI) is a global priority for improving patient safety and health outcomes. AKI is a sudden reduction in a person’s kidney function that often complicates episodes of acute illness.
We have developed this toolkit to disseminate learning highlighted from AKI case notes reviews, part of the RCGP AKI Quality Improvement project. Working with GP practices, we have put together resources, alongside national Think Kidneys guidance, to support the implementation of quality improvement methods into routine clinical practice. The toolkit aims to support improvements in both the recognition and response to AKI for adults in primary care as well as improve the delivery of post-AKI care.
As a clinical syndrome (not a condition or primary diagnosis), AKI offers a shift away from a single disease framework. It provides a lens to learn about generic factors affecting patient safety during and after episodes of acute illness. Lessons learnt can be applied to improving the delivery of care for people with a range of conditions, particularly those taking multiple medicines and living with complex health and social care needs.
This toolkit has been developed in partnership between:
- the RCGP Clinical Innovation and Research Centre
- the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC), Greater Manchester
- Think Kidneys
- Kent Surrey Sussex Academic Health Science Network (KSS AHSN)
- North East and North Cumbria AHSN (AHSN NENC).
NHS Education for Scotland, Healthcare Improvement Scotland and the NIHR Greater Manchester Patient Safety Translational Research Centre ( NIHR GM PSTRC) have also contributed to development of the toolkit and since April 2018 have also joined the RCGP AKI Quality Improvement Project.
Please send any feedback or suggestions to clinicalquality@rcgp.org.uk.
Kidney Health and AKI: Information for patients, carers, and healthcare staff
Kidney Health: Clinical importance and understanding
Although kidney health is paramount to overall health, healthcare staff and patients often lack understanding about kidney function in health and illness (eg. only 1 in 2 people are aware that kidneys make urine). The NHS Think Kidneys campaign has developed resources to support patient, public and professional awareness of kidney health and disease. The following resources may assist conversations with patients and carers about why and how to keep their kidneys healthy:
Think Kidneys: Almost everything you need to know about your kidneys
Acute Kidney Injury (AKI)
AKI is a sudden drop in kidney function occurring over hours or days. It is a marker of illness severity. There are many causes for AKI though in most cases it occurs as part of an episode of acute illness, such as flu or gastroenteritis. It is often the combined result of infection, being short of salt and water (i.e. low circulatory blood volume), low blood pressure (i.e. hypotension) and medication effects. It is not caused as a result of a physical blow to the body. It is associated with very poor patient outcomes so patients at risk of AKI should be informed about how to reduce their AKI risk especially if they become unwell.
- How to keep your kidneys safe: Information for patients at risk of AKI - How to keep your kidneys safe print version (223 KB PDF)
- Understanding Acute Kidney Injury: Information for patients who have had AKI - Acute Kidney injury print version (229 KB PDF)
AKI risk reduction strategies should incorporate assessment of fluid status and prompt medication review during acute illness episodes. The National Institutes of Health in the US have developed resources to support understanding and advice about drug management to help keep kidneys safe:
AKI e-Learning modules
- AKI in primary care: RCGP Learning (free for members to access). This module will help you to recognise patients who are at increased risk, detect AKI and initiate appropriate management. It will also help you to respond to the automated AKI Warning Stage which appear on kidney function test results.
- AKI: diagnosis and management in primary care: BMJ Learning (membership required). This interactive case based module covers the recognition, assessment, and management of AKI in the community. It contains practical advice for GPs, including when to refer and how to follow patients up after an episode of AKI.
AKI: Recognition and response
The NCEPOD report Adding Insult to Injury identified failings in recognition, investigation and management of patients with AKI. There is evidence that illness complicated by AKI is associated with:
- High mortality - over 20% of patients with AKI in hospital die during admission
- Increased length of hospital stay and utilisation of NHS resources
- Incomplete recovery of kidney function with many patients developing new or worsening chronic kidney disease (CKD)
Recognising and responding to AKI warning stage test results for adults in primary care
The presence of AKI is determined using internationally recognised criteria that are based on individualised changes in serum creatinine concentration with respect to that person’s usual (or baseline) value, and/or reduction in urine volume (see Think Kidneys guidance for primary care).
Primary care teams should prioritise early AKI detection because:
- In approximately two thirds of cases AKI begins in the community
- AKI is associated with poor outcomes, even for patients who are not admitted to hospital.
Strategies to expedite AKI recognition and response should include:
- Prompting AKI awareness and risk reduction strategies among patients and healthcare staff, because AKI often begins without symptoms specific to AKI
- Maintaining a low threshold to perform blood tests to check kidney function if “at risk” patients become unwell
- Timely review of patients whose blood results trigger AKI warning stage alerts* in order to interpret the test result in clinical context.
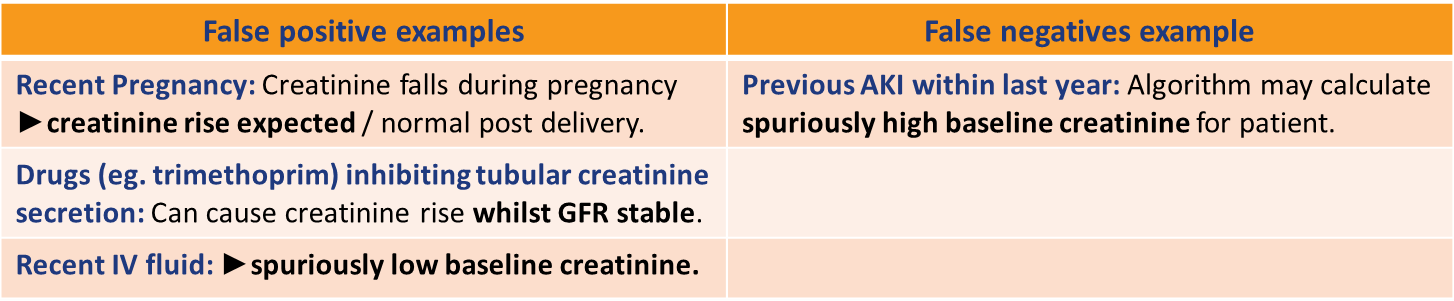
* NHS England has mandated that UK laboratories present AKI Warning Stage alerts alongside renal blood results, when potentially significant creatinine changes are identified. This system aims to highlight potential AKI cases promptly. The national AKI algorithm employs computer-based comparison of serial blood results and is unable to incorporate clinical context into assignment of AKI Warning Stage Test results. It is therefore imperative that clinical teams do not “rely” upon this system to accurately identify all AKI cases, as false positives and false negatives can occur if blood results are interpreted without clinical correlation. Although AKI Warning Stage alerts will help highlight most AKI cases, an overarching principal should be to “treat the patient not the test result”. Think Kidneys has published resources to support such timely validation and response to AKI warning alerts, tailored to primary care teams.
Table 1: Recommended response times to AKI Warning Stage Test Results for adults in primary care
Key questions when responding to an AKI Warning Stage Test Result:
Why was the blood test taken?
Clinical context at time of venesection influences the pre-test probability of the AKI Warning Stage Test Result:
- Routine chronic disease monitoring or drug monitoring? (Yes = AKI less likely)
- Assessment of acute illness? (Yes = AKI more likely)
It is good practice for primary care teams to implement processes to enable the person reviewing blood results to know “why” the test was taken, especially if 1) AKI was suspected; or 2) the blood results are likely to be sent to “Out of Hours” services. Enriching Summary Care Records can help better information exchange. Auditing response to AKI Warning Stage Test Results as well as conducting AKI case note reviews may support the development of a protocol for ensuring a safe and reliable system for managing tests.
Is this a true case of AKI?
AKI Warning Stage Test Results reflect changes in creatinine over time. Review of the clinical context and comparison with the patient’s baseline creatinine is necessary to decide if the patient with a warning stage test result does indeed have AKI. Consider:
- Is the patient acutely unwell? (If yes = AKI is more likely)
- Is the patient known to have chronic kidney disease (CKD) and is the change in creatinine due to progression of CKD rather than an acute change? (Particularly consider this if the baseline creatinine values are ≥ 12 months old; look at the serum creatinine values over a longer period of time to ascertain better the patients' baseline)
- Are there any other issues that might underlie a false positive result (table below)?
If still in doubt (and the patient is well) consider repeating the creatinine within 48-72hrs which will help determine whether the changes are dynamic/progressive or are stable (i.e. more consistent with CKD).
Any there any risk factors prompting early review / admission?
- Poor oral intake /urine output
- Hyperkalaemia, especially if moderate (K+ 6.0-6.4 mmol/L) or severe (K+ ≥ 6.5 mmol/L)
- Physiological evidence of deterioration (see NEWS2)
- Known CKD stages 4 or 5, or kidney transplant recipient
- Vulnerability to infection (therapeutic immunosuppression or immunodeficiency)
- Frailty with co-morbidities (CKD, diabetes, heart failure, liver disease, neurological or cognitive impairment)
- Past episodes of AKI
- Suspected intrinsic kidney disease (e.g. few pre/post renal features +/- abnormal urinalysis)
- Suspected urinary tract obstruction
Resources to guide response to AKI in primary care
The Think Kidneys Best Practice Guidance provides more detail on factors that require consideration when responding to AKI Warning Stage Test Results.
Table 2: Recognising and Responding to Acute Kidney Injury for Adults in Primary Care
Post-AKI Care: Primary care management after an episode of AKI
Informed by RAND/UCLA methodology, Table 3 provides consensus guidance to support tailored and timely care following a hospital admission complicated by acute kidney injury.
Aligned with NHS England Discharge Standards, Table 4 highlights top tips to support safer transitions of care for people who have had a hospital admission complicated by AKI.
Clinical implications and rationale
Adverse patient outcomes associated with AKI are not limited to episodes of acute illness with many patients remaining at risk of poor outcomes following AKI. These include:
- Increased risk of unplanned 90-day hospital readmission highlighting a need to coordinate timely post-AKI care across the secondary-primary care interface
- Increased risk of new or worsening chronic kidney disease (CKD) Increased risk of cardiovascular disease (especially if CKD 3B, 4 or 5 are present)
- Increased short and longer-term mortality
Key elements of Post-AKI care
Post-AKI care should be personalised to consider existing co-morbidities as AKI is a clinical syndrome with various causes and variable adverse outcomes, affecting a heterogeneous patient population. Factors determining the urgency of review include the cause(s) of the AKI, its severity, and the degree of kidney recovery following AKI. Key elements of post-AKI care include:
- Ensuring accurate diagnostic coding of AKI
- Optimising medicines management
- Coordinating monitoring of kidney function
- Communicating kidney health and AKI risk with patients and carers
- Ensuring accurate diagnostic coding of AKI
NICE has recommended that primary care teams establish AKI patient registers to facilitate systematic care for this high risk patient population. These aim to help:
- Identify patients that require timely post-AKI care planning
- Highlight vulnerable patients that require prompt review when acutely unwell
- Support quality assurance and future QI interventions
- Optimising medicines management
Optimising medicines management underpins safe post-AKI care. Key questions to consider include:
- Have medicines been stopped during the episode of acute illness?
- What were the original indications for these medications?
- Are there strong prognostic indications to restart medications?
- If, when, and how should medications be restarted?
- What is the patient’s blood pressure?
- Should any medications (e.g. NSAIDs) be discontinued?
- Is there an opportunity to rationalise medications and avoid unnecessary polypharmacy?
It is really important to restart drugs with prognostic benefit following AKI, as a failure to do so can result in avoidable patient harm. Timely reconciliation of medications post-AKI, tailored to a patient’s acute and chronic co-morbidities, will mitigate such adverse outcomes - patients with chronic heart failure represent a common exemplar patient group. While it is sometimes appropriate to "withhold" ACE-inhibitors and diuretic drugs during AKI episodes, patients with chronic heart failure are at high risk of decompensated heart failure, hospital readmission and death if these drugs are not reviewed post-AKI.
Think Kidneys have developed resources to support such medicines reconciliation post AKI and (in collaboration with The UK Renal Association and The British Heart Failure Society) to support interpretation of renal function changes when these drugs are used in clinically stable contexts post AKI.
Medication review post-AKI may also provide opportunities to:
- Minimise polypharmacy - Polypharmacy guidance (NHS Scotland) provides a stepwise approach to support decision making with patients living with complex health and social care needs (e.g. patients living with dementia; end of life care)
- Stop (or restrict) the use of NSAIDS unless there is a ‘compelling need.’
- Coordinating monitoring of kidney function
Why: Patients who have sustained AKI are at increased risk of developing new or worsening chronic kidney disease (CKD), even when they have recovered from AKI. Residual CKD following AKI represents a significant adverse outcome, and is a risk factor for cardiovascular, end-stage kidney disease and further AKI. Risk of developing new or worsening CKD is higher if:
- Kidney function remains below pre-AKI baseline
- AKI is severe or there are repeated AKI episodes
- There are orisk factors for CKD (eg. diabetes mellitus)
When: International consensus guidance recommends evaluating a patient’s kidney function 3 months after an episode of AKI to check for new onset, worsening or pre-existing CKD. Earlier monitoring should be prioritised if serum creatinine has not returned to a patient’s pre-AKI baseline, or if stipulated at point of hospital discharge. Non-recovery of kidney function 3 months post-AKI usually indicates new or worsening CKD and frequency of onward monitoring should follow NICE CKD guidance.
What: Where appropriate, assessment of a patient’s kidney health should include blood tests (electrolytes, serum creatinine and eGFR) to check for kidney function and a urine test (I.e. urinary albumin:creatinine ratio, ACR) to assess for evidence of proteinuria.
Context: In the context of providing person-centred care, kidney function monitoring needs to be tailored to a patient's individual health and social care needs. Key questions to consider include:
- What is the overall clinical context? Do not treat the test result in isolation; trade-offs may be required in the management of patients with heart failure, for example.
- Are there co-morbidities strongly associated with adverse outcomes (CKD, heart failure, diabetes)? Follow-up should be prioritised regardless of the degree of renal recovery.
- Has the episode of AKI been coded and communicated with the patient?
- Has the CKD been coded and communicated with the patient? Can follow-up prioritise person-centred care? Aligning kidney monitoring with pre-existing routine long-term condition review appointments may reduce patient burden.
- Communicating kidney health and AKI risk with patients and carers
Generating an agreed action plan with patients may help ensure timely review of medicines and kidney monitoring as well as support management of future episodes of acute illness. Resources to support communication include:
How to keep your kidneys safe: Information for patients at risk of AKI - How to keep your kidneys safe print version (223 KB PDF): developed by Think Kidneys in partnership with the RCGP and Kidney Care UK:
‘If you are unwell and unable to drink properly, particularly if you are losing excess fluid through vomiting or diarrhoea, or you have a high temperature and sweats, then it is important that you discuss your condition with a medical professional. This may be your GP or a specialist nurse, e.g. a heart failure or kidney nurse if you have one. You may be advised to discontinue taking medications which lower your blood pressure for a short time and a blood test will be arranged to check your kidney function. If you are admitted to hospital for a specialist x-ray or operation, you should make your health care team aware if you have Chronic Kidney Disease. If you are only passing small amounts of urine you may need admission to hospital and you should alert your GP to this.’
RCGP safety netting - The RCGP slide set aims to embed safety netting into routine care through:
- Advising patients ‘when to worry’
- Advising patients when to return for a review
- Providing verbal and/or written information
- Fixing follow-up before the patient leaves the consultation (when necessary)
- Read coding and clear documentation
Sick day guidance: Advising selected patients about cessation of medicines during specific acute illnesses (“Sick Day Guidance”) may form part of proactive care planning post-AKI. This should be decided upon an individual basis - such policies have not been formally evaluated and may risk inappropriate / unsafe self-medication changes if loosely applied to all patients. A Sick Day Guidance Position Statement (Think Kidneys Programme Board) includes:
‘In terms of medicines management, advice from the Think Kidneys Programme Board is that it is reasonable for clinicians to provide sick day guidance on temporary cessation of medicines to patients deemed at high risk of AKI based on an individual risk assessment. However, we consider that investment in a systematic approach to increase uptake of sick day rules guidance by patients should only be undertaken in the context of a formal evaluation.’
Embedding holistic post-AKI care planning into routine practice
Embedding key elements of post-AKI care planning into routine practice
Why: Arranging timely review for all patients who have experienced AKI is recommended in international consensus guidance, and embedding this into routine practice can help ensure that all patients receive the individualised care that they need.
When: Determine the urgency of post-AKI care review. All patients warrant planned follow-up post-AKI, as many will remain at increased risk of poor health outcomes. It may be possible to redirect workflow to assist in timely delivery of this aspiration. To determine the urgency of review acknowledging the burden of general practice workload, consider:
- Patient factors that should expedite review:
- Frailty or multi-morbidity. Kidney related care may be less urgent than other issues in such circumstances, for example anticipatory care planning may be prioritised when AKI episodes herald that frail, multi-morbid patients are failing.
- Pre-existing vascular disease or risk (CKD, diabetes, hypertension, heart failure)
- Polypharmacy
- Cognitive impairment
- Dependence upon a formal or informal carer
- Complex social needs
- Severe AKI (Stage 3 > Stage 2 > Stage 1)
- Renal function remains worse than patient’s pre-AKI baseline
- Significant illness caused AKI
- Patient required admission to critical care during admission complicated by AKI
How
- Establish a practice protocol for post-AKI care.
- Establish a proactive plan to support management of future episodes of acute illness
- Consider utilising generic resources to support patient and carer involvement in care planning, to help embed post-AKI care planning into routine practice
- Enrich Summary Care Records to support information exchange
A practice protocol may support care planning, including promotion of proactive holistic management and advanced care planning, in this high risk patient population.
- Does the patient have an existing care plan?
- If yes, does this need reviewing in light of recent episode of illness?
- If no, will the patient benefit from a care plan?
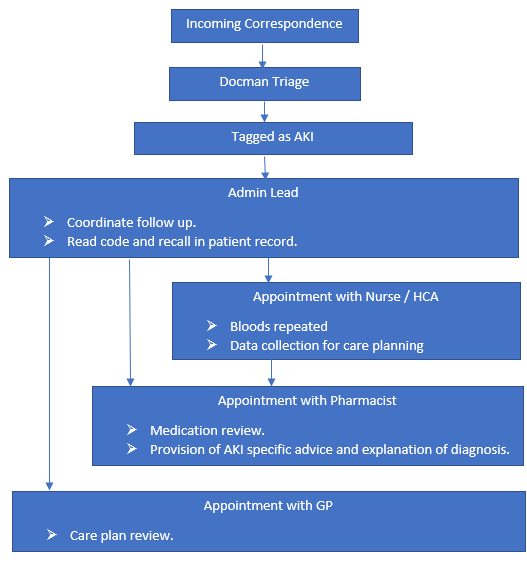
Members of the practice team to consider when embedding a protocol for identifying, coding, monitoring and managing this patient population include:
- GP lead
- Administration lead
- Practice pharmacist
- Community matron
- IT support - to help embed elements of AKI care into existing care plan documentation
Example of practice protocol developed by a practice based in Bury CCG:
Proactive follow-up for this high-risk patient population provides an opportunity to ensure involvement of patients and carers in decision making. Person-centred care planning includes supporting people to co-create individualised plans, visible to patients, carers and all sectors of healthcare. This will support better co-ordinated, safer healthcare and includes a need for:
- Shared understanding of the relevance of kidney health and AKI risk, in the context of chronic disease monitoring and medicines optimisation
- Plans for escalation of treatment in the event of acute illness
- Plans for modification of medication in the event of an acute illness
These priorities will vary according to individual need, incorporating: pre-existing co-morbidities; characteristics of the AKI associated illness; and the degree of kidney recovery
- Patient Capacity Assessment - This instrument aims to shift 'the focus from the medical condition of the person to their situation in life, identifies what the person values doing and being, explores how healthcare and other resources serve or limit this person, and recognises and cultivates opportunities to advance the person and their situation.'
- Social Prescribing – Taking into account individual’s health and social needs, consider the potential benefits of referring people to local, non-clinical services in the community
- Person Centred Care - RCGP resources to support the delivery of person-centred care
- NHS England toolkit for general practice supporting older people living with frailty
- Updated guidance on supporting routine frailty identification and frailty care through the GP Contract 2017/2018
- The House of Care – a framework for managing of long-term conditions
- Anticipatory Care Planning Toolkit
- RCGP Bright Idea - practice based development of questions to support anticipatory care planning
This section includes information on summary care records for each of the devolved nations:
Key Information Summary – Scotland
Best Practice Statement for Key Information summary (KIS) from the Scottish Government
Electronic Care Record - Northern Ireland
NI direct - resources to support understanding and use of Northern Ireland Electronic Care Record
Enriched Summary Care Records - England and Wales
- NHS Digital resources to support understanding and use of the Enriched Summary Care record in England and Wales
- Your Health and Care Records - NHS Choices resource to support understanding about health and care records
AKI and Quality Improvement
There is evidence that current mechanisms for improving safety and quality do not realise their full potential, for example, Audit and significant event analysis as part of Annual NHS appraisals.
There is a recognised need for quality improvement activities to help:
- Address system factors impacting on patient safety
- Aggregate data to encourage learning and improvement within and across organisations
- Involve patients and carers
By focusing on AKI as a lens through which we can shift away from a single disease framework and improve patient safety for patients, the opportunity arises to drive quality improvements in:
- medical safety
- safer transitions of care
- safety for vulnerable patients.
Within its Patient Safety Domain, NHS England established the Think Kidneys Programme through which a number of national levers have been introduced to improve the prevention, detection and management of AKI.
Principles underpinning AKI Quality Improvement
Addressing a major NHS priority, the RCGP Quality Improvement Project aims to be an exemplar of how to embed improvement methods in routine practice and provide a platform to realise the Triple Aim. The project aims to provide an example of how to improve patient safety in primary care and across the interfaces of care. In doing so, it hopes to mitigate safety risks that are common to multiple problems beyond AKI. Key principles underpinning AKI Improvement work are:
- Develop evidence based interventions grounded in an in-depth understanding of routine clinical practice
- Navigate the challenge of overdiagnosis: Maximise clinical utility of AKI as a driver of quality and safety whilst minimise treatment burden for patients (and corresponding unnecessary clinician workload)
- Support system resilience through person-centred collaborative working across the interfaces of care
Approaches to Quality Improvement
This section outlines two complementary approaches to supporting improvement in everyday clinical practice:
The QI Wheel for Primary Care
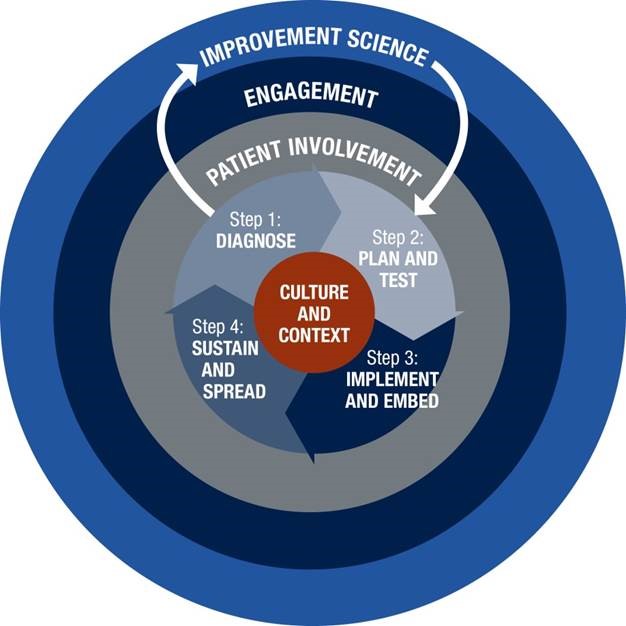
Informed by Institute for Healthcare Improvement methodology, the RCGP has developed the Quality Improvement Guide for General Practice. Key resources include:
- Process Mapping - creates a visual representation of a process enabling waste and areas for improvement to be identified
- Fishbone diagram - used to identify the root causes of a problem (also called a cause and effect diagram)
- Model for Improvement and PDSA (Plan Do Study Act) - proposes three questions to ask prior to testing a change using a PDSA cycle
Systems Thinking for Everyday Work (STEW)
The ‘Systems Thinking for Everyday Work (STEW)’ approach embraces a Safety-II perspective and is informed by the principles laid out in the white paper written by the European Organisation for the Safety of Air Navigation. A Safety-II perspective emphasises that healthcare organisations ‘might improve their ability to learn from past experience by studying not only what goes wrong (i.e. represented by incidents), but also by considering what goes right (i.e. by learning from everyday clinical work).'
The STEW principles act as a framework for teams to explore everyday work by obtaining multiple perspectives to understand how and why people adapt their ways of working to cope with the system conditions they face (such as competing goals or availability of information).
Access slides from the ‘Adopting a ‘systems approach’ to QI and safety work in frontline general practice’ session at the RCGP Annual Conference 2018.
Strategies for AKI improvement - AKI Case Note Review Templates
As part of the AKI Quality Improvement project, GP practices undertook case note reviews for patients who have generated an AKI alert and are now being looked after by in primary care.
24 general practices across England and Scotland conducted and reflected on case note reviews, conducting 148 in total.
Resonating with a Safety-II perspective, the AKI case note review templates are structured to identify patient safety issues, highlighting learning opportunities across care interfaces (Primary/Secondary; In/Out of Hours). The questions aim to promote learning from real-life AKI cases, rather than audit or criticise current practice.
RCGP AKI case note templates (800 KB DOCX)
- AKI Safety Template 1 is designed to support case note review of patients who have generated an AKI Warning Stage Test Result in primary care
- AKI Safety Template 2 is designed to support case note review of patients who have had a hospital admission complicated by AKI
- AKI Safety Template 3 is designed to aid reflection and learning through a summary of cases in order to create action plans for practice-level improvements in future care.
AKI Shared Learning from case note reviews – a summary of the key learning points and suggested actions for improvement
Strategies for AKI improvement - Further resources
The following resources may aid understanding of factors that underpin incorporation of AKI-related work into routine care. They may support practice-based discussions and generate discussion and learning across the interfaces of care:
- Practice Based Learning using STEW Framework: Learning generated from across the 24 participating practices and an example from a practice in Scotland: the Systems Thinking for Everyday Work (STEW) framework can generate learning on how to improve the management of AKI.
- Shared learning through Process Mapping and Fishbone diagrams - At the national RCGP Shared Learning Event in 2018, delegates worked in small multidisciplinary groups, undertaking process mapping to generate learning about the delivery of post-AKI care and fishbone diagrams to understand failures to respond to an AKI Warning Stage Test Result.
- Illustrated summary of presentations and exercises at the RCGP Shared Learning Event by medical artist, Dr Morium Howlader, GP.
Systems Thinking for Everyday Work: A Safety and Improvement Model for Healthcare
Resonating with a Safety-II perspective, the STEW Safety and Improvement Model offers a framework to integrate learning based on data generated through case note reviews (Work-as-done) as well as audit data (Work-as-imagined). Using the STEW principles framework can help identify key areas for improvement. These can inform discussions with relevant stakeholders to identify joint improvement targets and agreed actions (Work-as-designed). Through a participatory approach (i.e.co-development), the STEW framework aims to support a sustainable ongoing cycle of improvement grounded in an in-depth understanding of routine care.
The following links provide suggestions on how to use QI methods to:
Further resources and references
AKI Guidance, Quality Standard and Patient Safety Drivers
NICE AKI Guideline
Updated in 2019, the NICE AKI guideline is primarily intended to support the delivery of care by non-specialist clinicians working in a range of settings.
The guideline highlights a need for early intervention and emphasises ‘the importance of risk assessment and prevention, early recognition and treatment’
NICE AKI Quality Standard
Through a shared learning database, NICE have published links to Think Kidneys resources to support implementation of the the AKI Quality Standard.
National Patient Safety Drivers
A number of national levers were used to support improvement in the detection, treatment, management and prevention of AKI. These levers have included two patient safety alerts, published by NHS England and subsequently by NHS Improvement and a CQUIN.
NICE AKI Indicators for General Practice
NICE recommend that general practices establish and maintain a register of all patients who have had an episode of AKI.
In keeping with NICE recommendations for general practices to maintain an AKI register, the Bury CCG report presents results from an audit on the management of patients who have had an episode of care complicated by AKI.
Think Kidneys Resources
Care Homes
Think Kidneys has developed practical resources to raise awareness and help with the prevention, detection and management of AKI in care homes. The work was done by a cross-professional group comprising health care assistants, nurses, dietitians, care
home managers, commissioners, hydration specialists and academics.
Clinical Biochemists
Resources to assist laboratory teams in the implementation of the algorithm for reporting AKI warning stage test results, transmitting data to the UK Renal Registry with examples of best practice and top tips.
Commissioners
CCGs have in some areas been working across the whole health community, to improve safety and incidence rates of AKI.
Community Services
Publications and resources for clinical and support staff working in the community to help prevent, detect, treat and manage patients at risk of, or with, acute kidney injury.
Junior Doctors
Resources for use in secondary care including the minimum care bundle, who’s at risk of AKI and medicines optimisation and the Think Kidneys AKI App.
Mental Health
Information and resources for clinicians working in mental health to help prevent, detect and know how to manage patients at risk of, or with, acute kidney injury.
Nurses
Nurses, wherever they work, have a vital role to play in the prevention, detection and treatment of AKI. These resources are for all nurses, and have been added to the website following Think Kidneys discussions with AKI Nurses at their network meeting.
The resources are relevant and useful for nurses working at all levels and in all sectors of the NHS, and include work developed by AKI nurses.
Pharmacists
Think Kidneys have provided a range of resources for pharmacists.
Primary care
Think Kidneys has developed a range of resources specifically for primary care. The links provide members of the multidisciplinary team caring for people with, or at risk of AKI with information and guidance on how to respond. The aim is to improve safety
and outcomes for patients.
Secondary Care
Publications and tools for clinicians working at all levels and in all specialties across secondary care.
References and Further Reading
The Renal Association and British Society for Heart Failure have published national guidance to understand changes in renal function associated with drug treatment in heart failure.
GP and medical artist, Dr Morium Howlader presents 'The Journey of the Kidney' outlining the policy timeline and the emergence of AKI as a national priority.
This work was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Greater Manchester. The views expressed in this toolkit are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
To the best of our knowledge, the contents of this publication are in line with National Institute for Health and Care Excellence guidance relating to the management and treatment of acute kidney injury. Professional advice should be sought before taking, or refraining from taking, any action on the basis of the content of this publication. We cannot be held responsible for any errors or omissions therein, nor for the consequences of these or for any loss or damage suffered by readers or any third party informed of its contents. The AKI Quality Improvement Project Steering Group disclaims all liability and responsibility arising from any reliance placed on the information contained in this publication by you or any third party who may be informed of its contents.
Acknowledgements
A number of organisations, working groups and individuals contributed to the development of the AKI post-discharge guidance.
AKI RAND Consensus Panel
- Simon Sawhney
- Sarah Worboys
- James Larcombe
- Ben Carrigan
- Clare Allinson
- Nigel Taylor
- Zahra Iqbal
- Alistair Bateman
- Nick Jones
British Society for Heart Failure
- Paul Kalra
- Ahmet Fuat
- Teik Goh
NHS Education for Scotland
- Duncan McNab
- Royal Pharmaceutical Society
- Liz Butterfield
RCGP Overdiagnosis Group
- Margaret McCartney
- Jane Wilcock
- Doug McKechnie
Others
- Dr Krishnadas Thulasidoss
- Jeffrey C Fink
- Rebecca Doerfler
- Darren Green
- Jeffrey Schryer
- Leonard Ebah
- Prasanna Hanumapura
- Ally Moonie
- Claire Oates
- Owen David
- David Jewell