Syncope toolkit
Syncope is very common and will affect 42% of people during their lifetime
Definitions and causes of syncope and blackouts
Syncope and blackouts are both symptoms, and not a diagnosis in their own right. It is therefore important to establish the underlying causes. Syncope does not have the same meaning as blackouts.
In this section:
Definitions
Blackout is also known as Transient Loss of Consciousness (TLoC).
TLoC is defined as a state of real or apparent loss of consciousness with loss of awareness, characterised by abnormal motor control, loss of responsiveness, and a short duration.
Syncope is a subset of blackouts and is defined as TLOC due to cerebral hypoperfusion, characterised by a rapid onset, short duration, and spontaneous complete recovery. Syncope occurs when cerebral blood flow ceases for 6-8 seconds or there is a drop in systolic blood pressure below 60mmHg, and typically lasts for under one minute.
Presyncope describes the symptoms and signs that occur before losing consciousness. From studies in A&E, presyncope should be managed as for syncope as the prognosis is the same.
Orthostatic intolerance is a heterogeneous condition in which the standing position provokes a variety of symptoms such as dizziness, discomfort, nausea, and palpitations.
Causes of blackouts
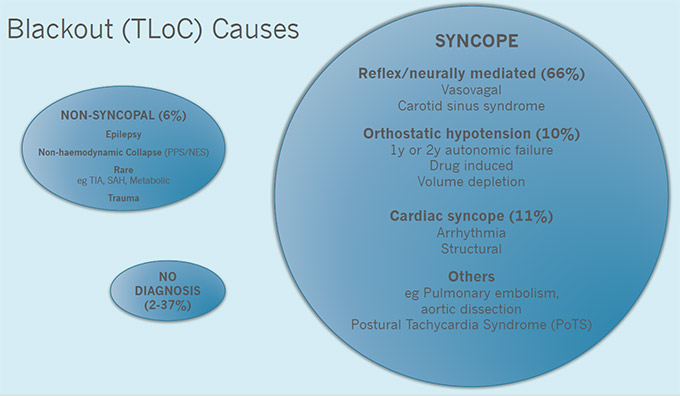
Diagram key:
- PPS - ‘psychogenic’ pseudo-syncope
- NES - non-epileptic seizures
- TIA - transient ischaemic attack
- SAH - subarachnoid haemorrhage
- 1y - primary
- 2y - secondary
Download causes of blackout diagram (89 KB PPT)
Mechanisms of syncope
Syncope is caused by a reduction in cerebral blood flow due to a drop in blood pressure. A fall in systolic blood pressure to below 60mmHg with or without a pause in heart rate of 6-8 seconds will usually cause syncope.
Blood pressure is the product of cardiac output and peripheral resistance, and a reduction in either can cause syncope.
Reduced cardiac output may be due to arrhythmia (bradycardia or tachycardia), structural disease, reduced cardiac contractility or reduced venous return to the heart and volume depletion.
Reduced peripheral resistance can result from failure to vasoconstrict or inappropriate vasodilatation.
Often more than one mechanism is present when syncope occurs.