Adult safeguarding toolkit
The Safeguarding Adults at Risk of Harm toolkit provides info sheets, templates, and handy guides for all the primary care team.
We are awaiting a review before updating this resource. Please use with caution.
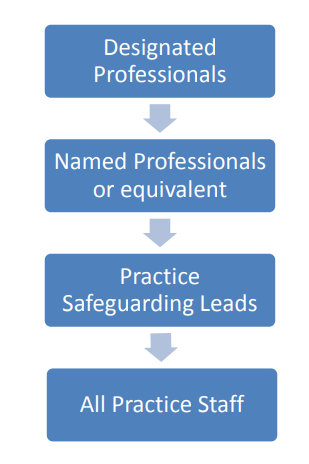
Below is a simplified outline of the safeguarding structure within primary care in England and Wales (this doesn’t include key agencies outside of health including adult social care who are the key partner and who lead adult safeguarding investigations):
Safeguarding is part of the holistic care that General practice offers to patients. Practices should therefore consider how they are going to embed safeguarding practice into their everyday routine.
Practice Safeguarding Leads
Each practice should have a GP Safeguarding Lead. This is vital to the embedding of Safeguarding practices within the practice. Effective safeguarding requires effective leadership and the Practice Safeguarding Lead should be supported by practices to take on this role.
Some practices may decide that one GP will take on the role of Adult and Child Safeguarding Lead, other practices may have a different GP for the Adult and Child Safeguarding Lead role; if this is the case, the two Safeguarding Leads should work very closely together as there is much crossover between adult and child safeguarding. Larger practices may decide to have a Safeguarding Deputy Lead also.
The role of the Practice Safeguarding Lead
It is important that practices recognise the importance to patient care of having a Practice Safeguarding Lead.
Practices should also recognise that as awareness of, and education around, safeguarding increases, there will be increased recognition of safeguarding issues and therefore time needed to manage these.
In order to lead safeguarding within their practices, the practice lead needs additional training over and above the usual Safeguarding training required for a GP.
The role of a Practice Safeguarding Lead may include:
- regular chairing of safeguarding team meetings within the practice which may include other community healthcare team members such as district nurses, midwives, palliative care nurses, health visitors and school nurses;
- being available to offer advice and guidance to GP colleagues on safeguarding cases;
- being available to listen to any safeguarding concerns raised by any member of the practice team;
- supporting staff who have been involved in safeguarding cases as these can be very challenging;
- meeting regularly with the key safeguarding administrator in the practice regarding coding, summarising and other issues;
- regularly attending Practice Safeguarding Lead Forums hosted by the CCG Named GPs (Named GPs exist only in England);
- being available to attend Adult and Child Safeguarding Conferences or facilitating a practice ethos that allows the most appropriate clinician to attend these;
- facilitating in-house staff safeguarding training such as updates;
- working closely with the practice manager;
- working closely with the practice Caldicott Guardian.
This list is not exhaustive but can be used as a starting point for practices to consider how they support the role of their Practice Safeguarding Lead to support safeguarding practices within their team.
Good practice idea – Consider implementing a regular ‘coffee time’ slot into your daily rota to enable discussions between clinicians about challenging cases and so that your Practice Safeguarding Lead can be available for advice.
Clinical Staff
All GPs and nursing staff should be fully aware of their safeguarding roles and responsibilities as defined by the GMC and NMC.
This short video, created by the service user sub-group of the Cheshire East Safeguarding Adults Board, is also an excellent resource for all practice staff to watch and generate discussion around adult safeguarding.
Administrative staff
- Each practice will have their own unique way of how they handle information coming into the practice. However, it is good practice to have a small team of staff who deal with all the safeguarding information to ensure consistency.
- It is ideal to have one administrative person within the practice who is responsible for the coding and summarising of new notes coming into the practice and who codes all the incoming safeguarding information. In practices where this is impractical, there should be a senior administrator who oversees the team coding and summarising and who is available for advice and direction in this area. This staff member will work closely with the Practice Safeguarding Lead.
- It is also imperative that each practice has a robust mechanism for ensuring the flow of safeguarding information in and out of the practice. For example, ensuring that Adult Safeguarding or Child Protection Conference reports are not included in notes copied for the purpose of an insurance report.
Reception staff
Reception staff also play a key role in safeguarding. They are the frontline of general practice and can help a vulnerable adult navigate their way through, what can sometimes be, a complex health system. They are also ideally placed to raise concerns. Examples of this could be by:
- enabling those who are vulnerable, such as an adult with learning difficulties, to make an appointment to see a GP;
- noticing that an elderly lady with dementia seems more confused than normal and keeps turning up for her appointments on the wrong day so highlights this to her usual GP;
- noticing that an adult seems to be struggling to read the registration form and discreetly taking that patient to a more private area to provide assistance;
- being aware that a young man with schizophrenia who attends the practice frequently for his injections is brought by a much older man who appears very controlling and abusive towards the young man in the waiting room and raises this concern with the nurse who regularly sees the patient and also his usual GP.
Practice managers
The role of practice managers in safeguarding should not be underestimated. The Practice Safeguarding Lead should work closely with the manager to embed a safeguarding ethos and culture in the practice and to ensure robust safe recruiting and management of any safeguarding concerns raised about staff members.
There should be a culture within the practice of empowering all staff members to raise any safeguarding concerns they have about either patients or staff.