Liver disease toolkit
The aims of the BLT/RCGP Liver Priority Project are to raise awareness of liver disease as an increasingly important cause of morbidity and mortality in the UK and to provide resources to support its optimal management in primary care.
Recommendations for commissioning bodies to improve the early detection of chronic liver disease in UK primary care
3) Develop an agreed local pathway for assessing the risk of liver disease, finding patients at risk, testing, following up and referring to secondary care
Look at whether there is an existing pathway that GPs are aware of and using in your area. Assess whether this meets the steps below. in different regions of the country, it is important that any pathway is agreed with secondary care, particularly around agreed methods of fibrosis testing and referral criteria. Examples of pathways working in parts of the UK are given below. They can be adapted according to your local needs and resources and all groups are happy to be contacted to discuss their pathways in more detail.
It is very important that the agreed pathway does not rely solely on liver blood tests or LFTs(liver enzymes) but adequately assesses liver fibrosis. The exemplar pathways showcase potential approaches for doing this.
The locally agreed pathway should include the following:
(i) Assessing the risk of liver disease for individuals – how to find patients at risk
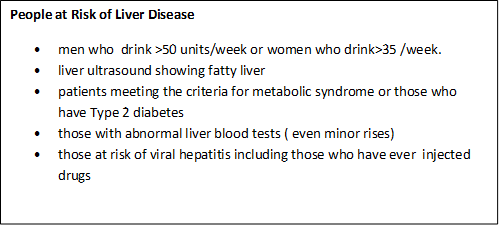
The main drivers of chronic liver disease in the UK are alcohol and the combined effects of obesity and type 2 diabetes. We recommend that services are commissioned so that liver disease is considered regularly in people with these risk factors as well as those with risk factors for viral hepatitis.
Alcohol related liver disease:
Recommendation 1: Assess and code alcohol risk (both dependence and non-dependent excessive drinking) using NICE/BSG guidelines and recognised tools
- At new patient registration
- During annual hypertension reviews
- As part of any NHS/other routine ‘health check’
- Opportunistically during consultations
- Aim for all registered adults to have their alcohol risk assessed at least every 5 years
Those at risk of alcohol related liver disease are defined by NICE as men who regularly drink over 50 units of alcohol or women who drink over 35 units of alcohol weekly.
Rationale for recommendation: Information on drinking behaviour is unlikely to be volunteered or coded unless people are routinely and regularly asked about their alcohol consumption. Alcohol-related liver disease contributes the biggest morbidity and mortality burden of all liver disease.
Non-alcohol related fatty liver disease:
Recommendation 2: Assess metabolic risk (obesity, Type 2 diabetes, other metabolic risk factors) leading to non-alcohol related fatty liver disease (NAFLD)
- Keep a register of all patients coded as having NAFLD
- Assess for NAFLD every 3-5 years in all registered patients with Type 2 diabetes (set up recall as for other chronic disease management)
- Code people with a liver ultrasound showing fatty liver
- Consider keeping a register of all patients meeting criteria for the metabolic syndrome and assessing for NAFLD in these patients as for people with Type 2 diabetes
Rationale for recommendation: Most patients at risk of NAFLD are likely to be under review for other reasons due to common metabolic and cardiovascular risk profiles. Only minor systems changes are needed to ensure liver disease is also routinely considered and coded in these patients.
Recommendation 3: Investigate incidental abnormal liver enzyme blood tests (LFTs)
These individuals are at risk of liver disease and should be investigated regardless of level of abnormality (use BSG guidelines to triage these patients and identify those at risk of common chronic liver disease as well as ruling out and referring on for rarer causes)
Rationale for recommendation: Patients with even minor abnormalities in their liver enzymes can have significant liver disease and a diagnosis should be sought /ruled out in all cases rather than re-testing/not acting on results. This is a cost effective approach and nationally recommended.
Viral Hepatitis:
Recommendation 4: Offer tests to those who inject drugs or have other risk factors for viral hepatitis
- People who inject drugs (PWID) should be offered testing for Hepatitis C routinely. 90% of HCV is acquired through injecting drugs
- Follow NICE guidelines to ensure testing for Hepatitis B and C is being carried out in high risk patients
- All patients testing positive for Hepatitis B and C should be offered referral to consider treatment options
Rationale for recommendation: Untreated hepatitis C infection causes cirrhosis and liver cancer. Very effective, well tolerated oral therapies are now available on the NHS. There are national and international targets to eliminate Hepatitis C within the next 15 years. There are also effective treatments to control Hepatitis B.
Recommendation 5: Diagnostic testing in patients at risk of chronic liver disease (Alcohol related and NAFLD) should focus on diagnosing/ruling out liver fibrosis
- Assessing fibrosis can be done using blood-based algorithms, serum fibrosis markers, transient elastography (fibroscan) or these methods in combination. The choice of tests depends on local availability.
- Do not use a set of normal routine liver enzymes (LFTs or liver blood tests) to rule out fibrosis in those identified as individuals at risk (including those with alcohol risk, NAFLD risk or viral hepatitis risk)
- Fibrosis assessment should run in parallel with brief interventions/lifestyle advice
- All patients where an initial liver screen, based on risk factors, has identified a cause other than alcohol or NAFLD should be referred to gastroenterology/hepatology
Rationale for recommendation: Liver fibrosis is the best predictor of progression to cirrhosis and poor clinical outcomes in patients with chronic liver disease. There are now several methods of assessing for fibrosis in the community. There is a lack of consensus around which is the best initial test of fibrosis to use, but it is important that ONE of the assessment methods is employed consistently according to local resources. All patients with liver disease aetiology other than alcohol or NAFLD require further investigation and management, which is not currently available in the community for most.
- Direct to fibroscan if available
- If not available then direct to ELF testing
- If neither available then referral to gastroenterology/hepatology
- Direct to ELF test if available (see NICE guidance)
- Or serum based algorithm test (Fib 4, NAFLD fibrosis score, AST:ALT ratio) followed by fibroscan if available
- If neither ELF or direct access fibroscan are available to request from primary care then referral on the basis of an indeterminate Fib 4, NAFLD fibrosis score or high AST:ALT ratio to gastroenterology/hepatology
Rationale for recommendation: There is a lack of consensus around which is the best initial test of fibrosis to use, but it is important that ONE of the assessment methods is employed consistently according to local resources. See example pathways later in this document.
Recommendation 7: Develop robust systems for follow up
- Individuals identified as being at low risk of liver fibrosis should be coded and re-assessed for fibrosis in the community using routine recall facilities every 3-5 years
- It is essential that follow up should include targeted brief interventions and lifestyle advice which should be coded and repeated if risk factors remain
- Alcohol support services and weight loss services should be used as available and considered to be commissioned or expanded to meet demand
- High risk individuals* should be referred for specialist follow up. Local referral pathways should be determined by local resource availability and capacity, in discussion with primary care, secondary care and commissioners.
Rationale for recommendation: If risk factors remain, patients at low risk of fibrosis may become high risk over time and it is crucial that these people are coded and followed up. To reduce this risk, brief interventions (both alcohol and weight loss) have been shown to be clinically and cost effective
*Note : There is some dispute around which ELF values and fibroscan scores should warrant referral/ cirrhosis assessment - commissioners should review the evidence and make locally agreed decisions in conjunction with the clinicians who will be receiving referrals
Recommendation 8: Audit any new pathway introduced to drive quality improvement making use of RCGP QI resources
Quality Improvement (QI) is an evidence-based approach that helps primary care free up time to deliver and evaluate initiatives, and embed new approaches more effectively and efficiently into practice. QI helps us to make the most of our systems, organisations, talents and expertise to deliver better outcomes for patients. Read more.
QI Ready is a free resource for all practices and has been developed to support GPs and practice teams with QI activities in practices. It is the starting place for all QI tools, guidance and case studies. Read more about the this RCGP programme here.