Liver disease toolkit
The aims of the BLT/RCGP Liver Priority Project are to raise awareness of liver disease as an increasingly important cause of morbidity and mortality in the UK and to provide resources to support its optimal management in primary care.
Recommendations for commissioning bodies to improve the early detection of chronic liver disease in UK primary care
4) Exemplar pathways to adapt for your local needs
The Scarred Liver Project, Greater Nottingham
The Scarred Liver Project is risk factor focussed and uses Fibroscan to stratify patients at risk of liver disease. Developed out of pilot project in 2014 a fully integrated CCG commissioned pathway is now in place across Greater Nottingham.
The scarred liver project has implemented an integrated pathway within the community to identify patients with risk factors for liver disease. GPs opportunistically identifying patients with risk factors for alcohol related liver disease, NAFLD or with unexplained abnormal liver enzymes are able to refer directly to liver fibrosis assessment using Fibroscan. All patients who attend for a Fibroscan® receive brief lifestyle intervention about their liver health. Patients stratified to have significant liver disease or cirrhosis are referred to a hepatologist for further review.
The pathway has been demonstrated to be cost effective (ICER per QALY £2138 for NAFLD and £6537 for ALD) and has seen over 3000 patients in its first 18months since full implementation in September 2016
Full details of the pathway, its evaluation, associated publications and contact details for the clinicians involved are available on the website.
The Gwent AST project
All blood tests sent from primary care where ALT is raised have a ‘reflex’ AST measured in the laboratory. If the AST:ALT ratio is >1 and no other diagnosed reason, advice to refer directly for transient elastography (fibroscan).All fibroscan >15 Kpa (likely cirrhosis) referred to hepatologist
Results so far (19 months of pathway in action):
- 13 % of abnormal ALT results revealed an AST:ALT ratio over 1 (1826 from 13929 ALTs requested in Gwent area)
- 648 were referred for fibroscan (some had other clear cause requiring alternative action, others not referred ?reason)
- 271 have had a fibroscan to date. 120 Fibroscan <8kPa = 44% (low risk of significant liver fibrosis; 73 Fibroscan 8-15 kPa = 27% (possible fibrosis/early cirrhosis); 76 Fibroscan >15 kPa = 28% (probably cirrhosis or advanced fibrosis)
Take home message: up to 30% of patients investigated along this pathway had likely cirrhosis of the liver. Simple pathway requiring minimal additional tests/GP time which picks up significant numbers of previously undiagnosed cirrhosis of the liver
For more information about this project please contact Dr. Andrew Yeoman, clinical lead for Welsh Liver Plan: andrew.yeoman@wales.nhs.uk
A Scottish Government supported, research funded, development of an automated investigation algorithm which maximises diagnosis and management.
1. GP requests LFTs via electronic system, entering data about patients’ alcohol consumption, BMI and features of metabolic syndrome.
2. In the laboratory, the finding of abnormal LFT results triggers an automated cascade of additional tests on the same sample to find an cause (viral serology, liver immunology, iron studies, alpha 1 anti-trypsin, and caeruloplasmin) and stage fibrosis (Fib 4 and NAFLD fibrosis score) This information automatically populates diagnostic algorithms and management plans.
3. The report is made available to the GP in real time for them to action. Access to the management plans is delivered electronically as web hyperlinks.
Results: In a trial of iLFT, the diagnosis rate was increased by 43% and it was cost-effective, with a saving to the NHS of £3,216 over a patient lifetime. It is now being rolled out in other sites across Scotland.
For more information about this project please contact Professor John Dillon, lead clinician on iLFT project at j.f.dillon@Dundee.ac.uk
Southampton
St Marys (a large, inner city practice) worked in partnership with secondary care to develop a pathway for the management of patients at risk of liver disease/ with abnormal LFTS. This was integrated in to the clinical system and liver health was promoted to patients through work with the British Liver trust (2016). The pathway was shared city wide in December 2017 and led to the commissioning of direct access fibroscan in October 2018.
Outcomes:
Within St Marys surgery population steep rise in coded / diagnosed liver disease:
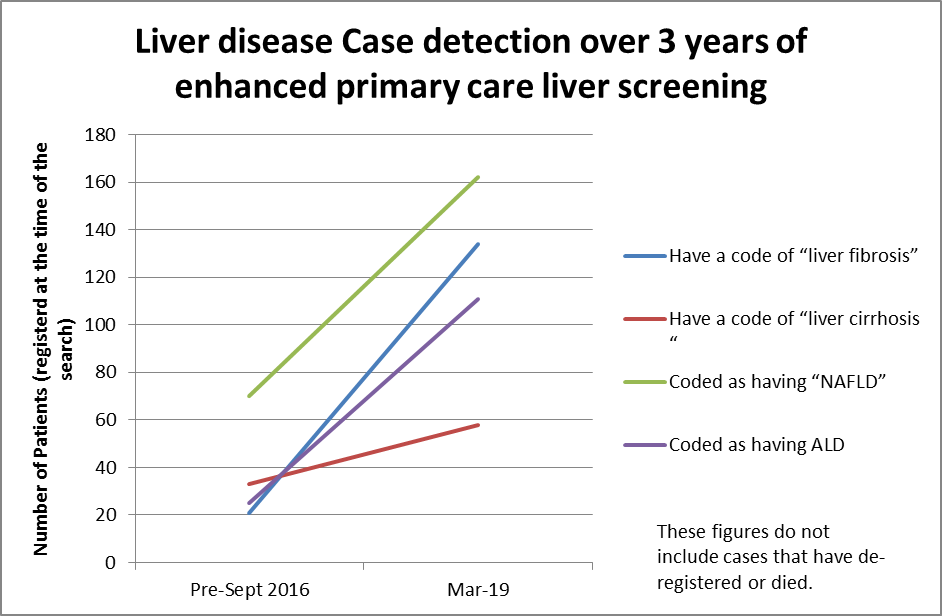
City wide data will be available shortly.
For more information about this project please contact Dr Mead Mathews, lead clinician and RCGP/British Liver Trust Liver Disease Clinical Priority Clinical Fellow, on meadmathews@nhs.net