RCGP Safeguarding toolkit
The aim of this toolkit is to enhance the safeguarding knowledge and skills that GPs already have to enable them to continue to effectively safeguard children and young people, as well as adults at risk of harm.
Key questions in safeguarding
These key questions link summary information from the toolkit to provide easily accessible information.
Presentations of child and adult abuse and neglect in general practice are seldom clear-cut and well-defined. Both children and adults can experience different types of abuse at the same time. There are many similarities to the presentations of different types of abuse, such as change in behaviour, mental health difficulties including self-harm, drug and alcohol use, disturbed sleep, and physical symptoms and signs.
Identifying abuse and neglect is not always easy. Knowing the signs of the different types of child and adult abuse helps to be able to identify possible concerns about abuse and neglect, as well as giving a voice to children and adults who are experiencing abuse.
Part 2 of the toolkit outlines the different types of abuse that children and adults can experience and how these might present in general practice. There are many signs that are common indicators of many different types of abuse such as behaviour changes and mental health concerns. Identification of any signs of abuse should prompt further exploration using professional curiosity.
Always keep abuse and neglect in mind as a potential cause for any reason a patient may present in general practice.
Responding to concerns about child abuse.
There are five steps to take. These are summarised here with further information and guidance in Part 3 of the toolkit.
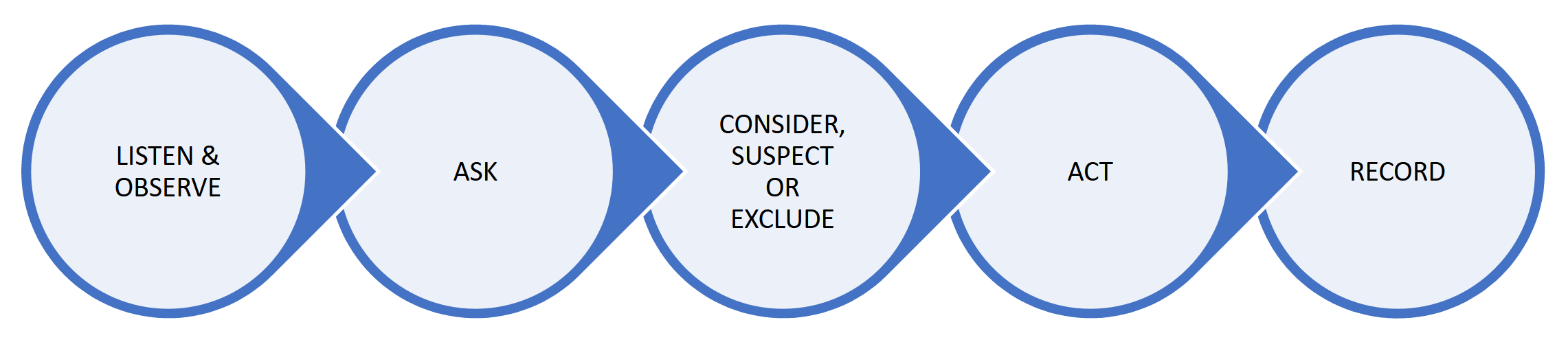
- Step 1. Listen and observe. Piece together any information you already have about that child and family.
- Step 2. Ask. Seek an explanation for any injury, presentation or concern from both the parent or carer and the child/young person (if possible, dependent on age, communication needs, disabilities).
-
Step 3. Consider, suspect or exclude abuse or neglect:
- Consider – child abuse is one possible explanation for the concerns and is included in your differential diagnosis.
- Suspect – you have a serious level of concern about the possibility of child abuse (you do not need to have proof).
- Exclude – a suitable explanation is found for your concern.
-
Step 4. Act.
- If you suspect child abuse, you should follow your local multi-agency safeguarding processes and make a safeguarding referral to children’s social care/Health and Social Care Trust (Northern Ireland).
- If you are considering child abuse, you should decide on what further action needs to be taken, such as gathering further information, discussing your concerns and arranging review of the child.
- If you have excluded child abuse at this time, you should continue to exercise professional curiosity and be prepared to once again consider or suspect child abuse should the situation change, or new information come to light.
- Step 5. Record. Ensure clear documentation in the child’s record (and that of any other family member as appropriate). Mark entries ‘not for online access’.
Responding to concerns about adult abuse.
There are five steps to take. These are summarised here with further information and guidance in Part 3 of the toolkit.
- If you are unsure, seek further advice from a colleague, your organisational safeguarding lead or local safeguarding professionals.
- Ensure the patient is safe and deal with any immediate medical needs.
Is the adult an 'adult at risk/adult at risk of harm'?
YES: consider an adult safeguarding referral and follow steps 4 & 5 below.
NO: consider:- other sources of support for the adult
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation if new relevant information comes to light
- Continue to monitor the situation as risk and the ability to safeguard themselves may change over time.
Does the adult at risk of harm have capacity to make a decision about a safeguarding referral?
NO: proceed with an adult safeguarding referral.
YES and they consent to a referral: proceed with an adult safeguarding referral.
YES but they do not consent to a referral: consider:- whether they need more information on the safeguarding adult process, which might address any concerns they have
- what other sources of support are available
- whether any others are at risk of harm and for whom a safeguarding referral needs to be considered, such as any children or other adults who are adults at risk of harm
- whether the level of harm is potentially so serious that a different type of referral is required such as a MARAC referral in the cases of high-risk domestic abuse
- reassess the situation at appropriate intervals as risk can change as can an adult’s ability to protect themselves.
- reassess the situation if new relevant information comes to light
UNCERTAIN: discuss with a colleague, your organisational safeguarding lead or local safeguarding professionals.
NOTE FOR PRACTITIONERS WORKING IN WALES – all practitioners working in Wales should be aware of the statutory ‘duty to report’.
- The practice/organisation safeguarding lead.
- A more experienced colleague.
- The Caldicott Guardian or Data Protection Officer if you need advice about information sharing.
- Local safeguarding professionals such as Named GPs/Nurses for Safeguarding, Designated Health Professionals, safeguarding leads within health boards.
- Social worker – you can contact your local authority/Health and Social Care Trust by phone and ask to speak to the duty social worker if you have an urgent safeguarding concern. You can find these numbers on the safeguarding section on the website of your local authority, or in Northern Ireland, your local Health and Social Care Trust.
- The phone numbers for your local safeguarding professionals, local authority, Health and Social Care Trust (Northern Ireland), should be clearly displayed and easily accessible within your organisation.
- For practitioners in England, the NHS Safeguarding App is an easy way to find your local authority details. It can be accessed by visiting your device’s appropriate app store and searching for ‘NHS Safeguarding’.
Information sharing is essential to safeguarding children and adults.
Sharing information in a safeguarding context means sharing relevant personal information about children and adults that multi-disciplinary and multi-agency professionals and agencies hold. The information is shared in order to safeguard children and adults from abuse and neglect.
Below are the key principles of information sharing and a summary of the ‘Why, When, Who, What and How’ of information sharing. Further guidance, including on issues around consent, can be found in Part 5 of the toolkit.
You can also find more guidance on making child and adult safeguarding referrals in Part 3 of the toolkit (if needed).
Summary of the ‘Why, When, Who, What and How’ of information sharing for the purposes of safeguarding:
When there is a concern that a child is at risk of, or is experiencing, abuse or neglect.
When there is a concern that an adult is at risk of, or is experiencing, abuse or neglect and one of the following:- It is required by law.
- The adult provides consent for the information to be shared.
- The adult does not have the capacity to provide consent for the information to be shared.
- It is in the public interest, i.e. there are others at risk of serious harm, or it is necessary to share information to prevent a serious crime or there is an imminent risk of serious harm to the individual.
Information can also be shared when safeguarding advice is being sought – this can often be done without sharing the names or other identifying features of the patient involved.
- General practice multi-disciplinary team.
- Wider health multi-disciplinary team.
- Multi-agency safeguarding partners.
- Other relevant agencies as appropriate.
- High quality documentation of safeguarding information is fundamental to safeguarding children and adults in order to:
- ensure victims and survivors of abuse have the healthcare and support they need
- allow a picture to be built over time of emerging concerns
- manage and share information about risk appropriately
- allow for effective information sharing when required
- allow for discussions with patients about online access where there are safeguarding concerns.
- Experiencing abuse and/or neglect as a child or adult has significant implications on health and wellbeing so therefore needs to be documented.
- All safeguarding information should be stored within the medical record, not separate to it.
- Any documents containing third party information should be flagged as such with the appropriate code.
- It is not necessary to black out information within safeguarding documents before putting into the patient record.
- The use of coding to record key safeguarding information is important to be able to easily find the relevant information when needed in the future or for audit purposes.
- Safeguarding information should be managed safely to reduce the risk of perpetrators using any disclosures of abuse from victims (or any information in the medical record) to further abuse them.
- If any member of staff is unsure how to manage safeguarding information, they should always seek advice from the practice safeguarding lead/Caldicott Guardian/Information Governance lead/Data Protection Officer.
- All safeguarding information should be redacted from patient online access and clearly marked ‘not for online access’.
Further information and guidance on documenting and coding safeguarding information.
Having knowledge of local safeguarding policies and procedures is essential to effective safeguarding. This table outlines the knowledge you need so that you can take prompt safeguarding action when necessary. Please access the downloadable version of the table (DOCX).
How do I contact them?
How do I contact them?
Safeguarding learning is a continual process and enables us to have the knowledge and capabilities to safeguard our patients.
The RCGP Safeguarding Standards set out the professional safeguarding standards and safeguarding training requirements for GPs and anyone working in any general practice setting in the UK. This includes, but is not limited to, NHS GP practices, independent and online providers of general practice services, Primary Care Networks (PCNs), GP out of hours and extended access services. The standards combine and include both safeguarding children and adults and are a whole life course document. These standards form part of the wider intercollegiate documents on safeguarding knowledge and competencies for all healthcare staff.
It is important to note that both adult and child safeguarding knowledge and capabilities are equally necessary and expected for all staff in general practice, even if the staff member only works with adults.
The RCGP Safeguarding Standards set out five key areas of safeguarding knowledge and capabilities, shown here.
- Understanding statutory, legal, professional and employment safeguarding responsibilities and duties, including the obligation to act when there is a safeguarding concern.
- Preventing abuse and neglect as far as possible through timely action and intervention.
- Accounting for the influence of personal beliefs, experience and attitudes.
- Maintaining individual wellbeing.
- Supporting colleague wellbeing.
- Recognising indicators and signs of all types of abuse and neglect in children and adults.
- Identifying children and adults who may be more vulnerable to abuse and neglect.
- Applying principles of consent, confidentiality and capacity in relation to safeguarding.
- Mitigating barriers to healthcare faced by victims and survivors of abuse.
- Understanding the lifelong impact of abuse.
- Learning from those with lived experience of abuse.
- Practising in a trauma-informed way.
- Applying relevant legislation.
- Being vigilant and addressing organisational/institutional abuse/neglect.
- Acting when there is a safeguarding concern.
- Talking to children, adults, families, parents and carers about abuse.
- Following local referral processes for child and adult safeguarding.
- Contributing to the lifelong holistic care needed by victims and survivors of abuse.
- Seeking advice and guidance and escalating concerns when necessary.
- Promptly acting on, and responding appropriately to, any concerns or allegations about persons in a position of trust.
- Documenting safeguarding concerns accurately and safely in the patient record.
- Managing safeguarding documents in line with best practice in information governance and data protection.
- Proactively addressing safeguarding challenges of patient online access including coercion to access records.
- Participating in multi-agency and multi-disciplinary working.
- Sharing information appropriately and proactively in a safeguarding context.
- Contributing to safeguarding reviews.
- Learning from safeguarding serious case reviews (local and national).
This table gives a summary of the safeguarding training requirements as set out in the RCGP Safeguarding Standards for GPs and anyone working in a general practice setting in the UK. Also see ‘RCGP safeguarding standards for general practice’.
- Receptionists, administrative and secretarial staff (with the exception of manager/lead roles of these groups who will need level 2).
- Volunteer staff.
- Safeguarding included in practice/organisation induction AND completion of relevant safeguarding level 1 eLearning updates.
- Level 1 safeguarding update.
- Practice managers (including deputy managers) and equivalent leadership roles. [ALSO SEE ADDITIONAL REQUIREMENTS FOR THIS GROUP]
- Care navigators.
- Reception managers.
- Safeguarding administrators.
- Managers/leads of administrative/secretarial teams.
- Health care assistants, pharmacy technicians.
- Safeguarding included in practice/organisation induction AND completion of relevant safeguarding level 2 eLearning updates.
- Complete relevant safeguarding level 2 eLearning modules.
- Have a safeguarding induction with an appropriate senior leader e.g. practice manager/practice safeguarding lead depending on nature of role. This induction should include:
- discussion about the safeguarding structure, policies and procedures within the practice/organisation
- identification of any areas of professional development related to safeguarding.
- Level 2 safeguarding update
- GPs, practice nurses, physician associates, nursing associates, pharmacists, paramedics, Advanced Care Practitioners, Advanced Nurse Practitioners, social prescribers, mental health workers, physiotherapists, podiatrists, dieticians and any similar ARRS (Additional Roles Reimbursement Scheme) roles.
- Primary care network (PCN) safeguarding roles in England such as PCN safeguarding co-ordinators.
- GP speciality trainees [who should refer to the specific safeguarding training requirements for the workplace based assessment (WBPA) part of the MRCGP exams]
- Safeguarding included in practice/organisation induction.
- Completion of relevant safeguarding level 3 eLearning updates (or provide evidence of prior completion) e.g. RCGP modules.
- Meet with the practice/organisational safeguarding lead, their deputy, or other relevant senior leader within one month of starting their new role to:
- discuss the safeguarding structure, policies and procedures within the practice/organisation
- identify any areas of professional development need related to safeguarding.
- Level 3 safeguarding update.
- Completion of the Safeguarding Structured Reflective Template to demonstrate reflection and learning across the breadth of all the five areas of safeguarding knowledge and capabilities. This must include both child and adult safeguarding issues, even if a practitioner only works with adults.
Annually:
- Safeguarding update.
- Demonstrate regular attendance at the local practice safeguarding lead forums (if available in the locality).
- Demonstrate an example of reflection/learning aligned with the practice/organisational role specific knowledge and capabilities.
- The practice/organisation safeguarding lead.
- A more experienced colleague.
- Caldicott Guardian or Data Protection Officer, if you need advice about information sharing.
- Local safeguarding professionals such as Named GPs/Nurses for Safeguarding, Designated Health Professionals, or safeguarding leads within health boards.
- Social worker – you can contact your local authority (Health and Social Care Trust in Northern Ireland) by phone and ask to speak to the duty social worker if you have an urgent safeguarding concern.
For those who are new to general practice, or general practice in the UK, we recommend first completing the RCGP eLearning course - Core Safeguarding in General Practice (Level 3). These modules provide an overview of safeguarding in general practice in the UK and will also be useful to any practitioner as a safeguarding update or refresher. Completing the modules, along with the essential reading list, will provide a solid background in safeguarding.
When you have completed the eLearning modules and the essential reading list, you will have a great foundation in safeguarding that you can build throughout your career in UK general practice. See ‘What safeguarding training do I need?’ above for further information on training requirements.
- A resource for busy GPs and general practice staff to refer to when they need safeguarding support or are unsure of what steps to take when they have a safeguarding concern about an adult or child.
- An educational resource to support the building and development of safeguarding knowledge and capabilities. Some practitioners might dip in and out of the toolkit when they need to, others may read through it systematically over time to support their safeguarding learning.
- A resource for practice safeguarding leads to use to support safeguarding learning and reflection in their organisation.
There are five parts to the toolkit – these match the five different key areas of safeguarding knowledge and capabilities set out in the RCGP Safeguarding Standards. Contents of the toolkit are summarised below:
- Essential reading list.
- Safeguarding roles and responsibilities in general practice.
- Safeguarding and personal wellbeing.
- Summary of relevant safeguarding legislation and guidance in each UK nation.
- Identifying child abuse and neglect:
- the rights of children
- adverse childhood experiences (ACEs)
- safeguarding young people aged 16 and 17 years old
- age of consent, Fraser guidelines and Gillick competence
- how does child abuse/neglect present in general practice?
- obstacles to recognising and responding to child abuse and neglect
- where do children experience abuse and neglect
- contextual safeguarding
- children at greater risk of abuse and neglect
- children who may be invisible to services
- looked after children
- caring for refugee and asylum seeking children
- perinatal safeguarding
- unseen men
- disguised compliance
- types of abuse and neglect (including Was Not Brought).
- Radicalisation (covers child and adults).
- Domestic abuse (covers child and adults) including ‘honour’ based abuse and forced marriage.
- Transitional safeguarding.
- Identifying adult abuse and neglect:
- human rights based approach
- principles of safeguarding
- types of abuse and neglect
- organisational abuse including safeguarding in care homes
- adults at greater risk of abuse and neglect
- how does adult abuse/neglect present in general practice
- safeguarding those who are homeless
- Was not brought.
- How should we respond when we have concerns that a child or adult is experiencing abuse or neglect?
- Responding appropriately and effectively in general practice to concerns about abuse.
- Talking to children, adults, families and carers about abuse.
- Trauma-informed practice.
- Responding to concerns about child abuse:
- the child’s voice
- five-step process to responding to concerns about child abuse and neglect:
- listen and observe
- ask
- consider, suspect or exclude
- act
- document
- early Help
- making a child safeguarding referral
- top tips for making a child safeguarding referral and writing safeguarding reports– The 5 Cs
- working with parents and carers when there are safeguarding concerns about their children/the children they care for
- child protection system in the UK.
- Responding to concerns about adult abuse:
- five-step process to responding to concerns about adult abuse and neglect:
- concern about abuse
- the views of the adult
- is the adult an ‘adult at risk of harm’?
- assessing mental capacity (includes mental capacity principles, decisional and executive capacity, ‘unwilling’ or ‘unable’ to safeguard, assessing capacity in complex situations and in self-neglect, giving medication covertly
- is a safeguarding referral needed?
- what should happen if an adult at risk of harm has capacity but does not want any safeguarding procedures and is unwilling to take steps to safeguard themselves
- making safeguarding personal
- making an adult safeguarding referral
- top tips for making an adult safeguarding referral and writing safeguarding reports – the 5 Cs
- adult safeguarding processes.
- five-step process to responding to concerns about adult abuse and neglect:
- Contributing to the lifelong holistic care of victims and survivors of abuse.
- Responding to allegations of abuse regarding staff or persons in a position of trust (PiPoT).
- Documenting and coding safeguarding information in the electronic medical record.
- Key principles of documenting safeguarding concerns and information in the patient electronic medical record.
- Who is responsible for managing safeguarding information in the practice/organisation?
- What is ‘safeguarding information’?
- Sources of safeguarding information.
- Recording family groups/relationships.
- Domestic abuse – specific guiding of domestic abuse and MARAC information.
- Recording adult drug and alcohol problems, mental health problems and learning disabilities.
- ‘Was not brought’.
- Management of child protection conference invitations, reports (including those provided by general practice and those received) and minutes.
- Management of adult safeguarding conference invitations, reports(including those provided by general practice and those received) and minutes.
- Contextual safeguarding situations.
- Information about perpetrators of abuse.
- Codes to use.
- Managing safeguarding information in the context of patient online access.
- Key principles of information sharing.
- The challenges of information sharing.
- The why, when, who, what and how of information sharing.
- Information sharing and the law.
- Consent.
These two templates have been developed to support safeguarding learning and reflection. They can be used to support annual appraisal as well as revalidation.