Royal College of General Practitioners - Online Learning Environment
Search results: 41

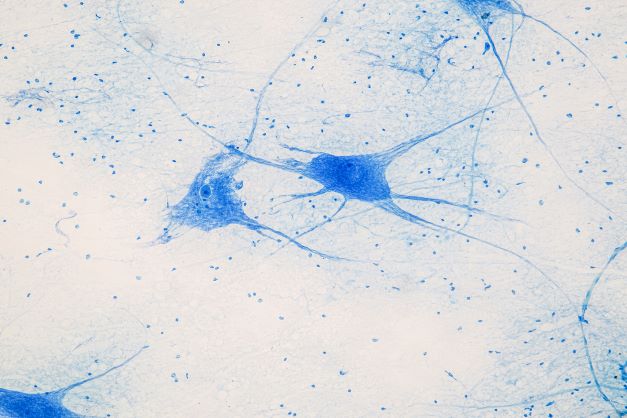
Allergies are a major public health concern in the UK, with rates of allergy increasing and a shortage of consultants who specialise in this area. Asthma and food allergy can be life-threatening; conditions such as allergic rhinitis and eczema, whilst not obviously as severe, can have medical consequences and a significant effect on quality of life and educational achievement. This course aims to educate GPs about the various presentations of allergic disease, how to assess an atopic patient and when to investigate in primary care or refer to secondary care. Find out more about the course by watching the video.
Editorial and content decisions were made solely by the RCGP.

Atopic conditions such as asthma, eczema, allergic rhinitis (hay fever) and food allergy commonly present in primary care. In the last few years we have seen tragic deaths from food allergies make the headlines, and we know that over 2% of children in the UK are affected by peanut allergy, with estimates of lifetime prevalence for any food allergy reaching around 20%. Allergic rhinitis is even more common, affecting up to 50% of the population worldwide; it is often seen as a mere summer inconvenience but is more significant than this, being associated with poorly controlled asthma and impaired performance in school exams and at work. The National Review of Asthma Deaths serves as a timely reminder that allergy is a key consideration in severe asthma, with trigger factors being recorded for under half of those featured in the report. Eczema also has a significant effect on quality of life; children with eczema are more likely to be bullied, to miss school, and to have poor school performance than their peers and are at a higher risk of depression than the general population.
The RCGP allergy hub provides a variety of resources to help learners to improve their knowledge on allergy. The eLearning course on allergy has four modules which between them cover all of the atopic conditions already discussed. A pre and post course MCQ allows users to test the improvement in their knowledge after doing the course.
There are also a variety of podcasts which cover different
aspects of the diagnosis and management of allergy in primary care,
particularly the difference between IgE mediated and non-IgE mediated allergy.
Non-IgE mediated allergy can be more difficult to diagnose, because symptoms
may present some time after the allergen was ingested, and may not be initially
recognised as being allergic in origin. The connection between asthma and
allergic rhinitis is discussed, using the concept of the one-airway theory.
Pollen food syndrome, otherwise known as oral allergy syndrome, is also the
subject of a podcast; whilst this allergy is usually mild and short lived, it
can cause anxiety if oral symptoms are incorrectly interpreted as the start of
a more sever reaction. In many of our courses and podcasts we attempt to do
some myth busting, so that patients can access accurate information from their
GPs, and any incorrect assumptions can be challenged. Finally, there are four
short screencasts which provide bite-sized updates for the time-pressed GP who
wants to know more about eczema, peanut allergy, asthma or allergic rhinitis.
References:
- https://cks.nice.org.uk/topics/food-allergy/
- https://cks.nice.org.uk/topics/allergic-rhinitis/
- https://cks.nice.org.uk/topics/eczema-atopic/
- Walker S, Khan-Wasti S, Fletcher M et al. Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study. J Allergy Clin Immunol. 2007 Aug;120(2):381-7.
- de la Hoz Caballer B, Rodríguez M, Fraj J, Cerecedo I, Antolín-Amérigo D, Colás C. Allergic rhinitis and its impact on work productivity in primary care practice and a comparison with other common diseases: the Cross-sectional study to evAluate work Productivity in allergic Rhinitis compared with other common dIseases (CAPRI) study. Am J Rhinol Allergy. 2012 Sep-Oct;26(5):390-4
- Royal College of Physicians. Why asthma still kills. May 2014. https://www.rcplondon.ac.uk/projects/outputs/why-asthma-still-kills


Within the five years following an injury to their anus and pelvic floor during childbirth, over one in five women cannot reach a toilet in time, losing control of flatus or faeces. For many anal incontinence (AI) symptoms occur soon after childbirth, but others find it starts or worsens during or after the menopause. The physical, emotional and social impact of AI can be profound and long lasting. Women suffering AI have reported anger, feeling unclean, relationship breakdown, isolation and loss of self-esteem. Women may feel embarrassed by symptoms and unaware that help is available. It takes, on average, seven years before women with AI are seen by a professional with the training and experience to treat their symptoms. Encouraging practitioners to opportunistically enquire about possible symptoms, and empowering women to disclose their concerns, can enable access to timely advice and treatment thus improving women’s physical, emotional and social wellbeing.
An educational grant was received by University of Warwick for the production of the course. The research that informed the materials and the costs of course production were funded by the National Institute for Health Research (NIHR) Research for Patient Benefit (NIHR202172).The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Editorial and content decisions were made solely by the RCGP.

Available until Thursday 30 October 2025.
This One Day Essentials Cancer care conference is a learning event to inform primary care of knowledge and innovations in improving cancer care – for GPs in their everyday clinical practice. The conference will cover a range of topics including the evidence base for urgent referrals and RDCs, safety netting tips and tools, latest advances in cancer testing/detection (including multi-cancer early detection tests), the evolving role of primary care networks and wider primary care teams. Supporting patients living with and beyond cancer and when to think about cancer recurrence. Finally we will look to the latest hot topics and future of cancer care. The conference will provide GPs with knowledge to impact and improve care of cancer patients in their own practices, as well as inform GPs of changes and innovations that will impact the role of early cancer diagnosis in primary care.
Topics include:
- Use of urgent suspected cancer referrals and in non-specific presentations rapid diagnostic centres (RDC)
- Safety netting tips and tools
- Latest advances in cancer testing and detection including multi-cancer early detection (MCED) tests
- Primary Care Networks and wider primary care teams - Improving Early Diagnosis of Cancer
- Supporting patients living with and beyond cancer
- Latest Cancer Hot Topics for GPs
Learning objectives:
- Up to date on the latest evidence for early cancer detection in primary care
- Current primary care tests and how they can help in cancer risk assessment
- Novel approaches to cancer detection including multi-cancer early detection (MCED) tests
- Embedding safety netting in your clinical practice
- Understand non-specific symptom (NSS) presentations and use of rapid diagnostic centres (RDCs)
- Supporting cancer patients once diagnosed and living with and beyond their cancer
Conference Chair:
Dr Thomas Round, General Practitioner and Academic Clinical Research Fellow


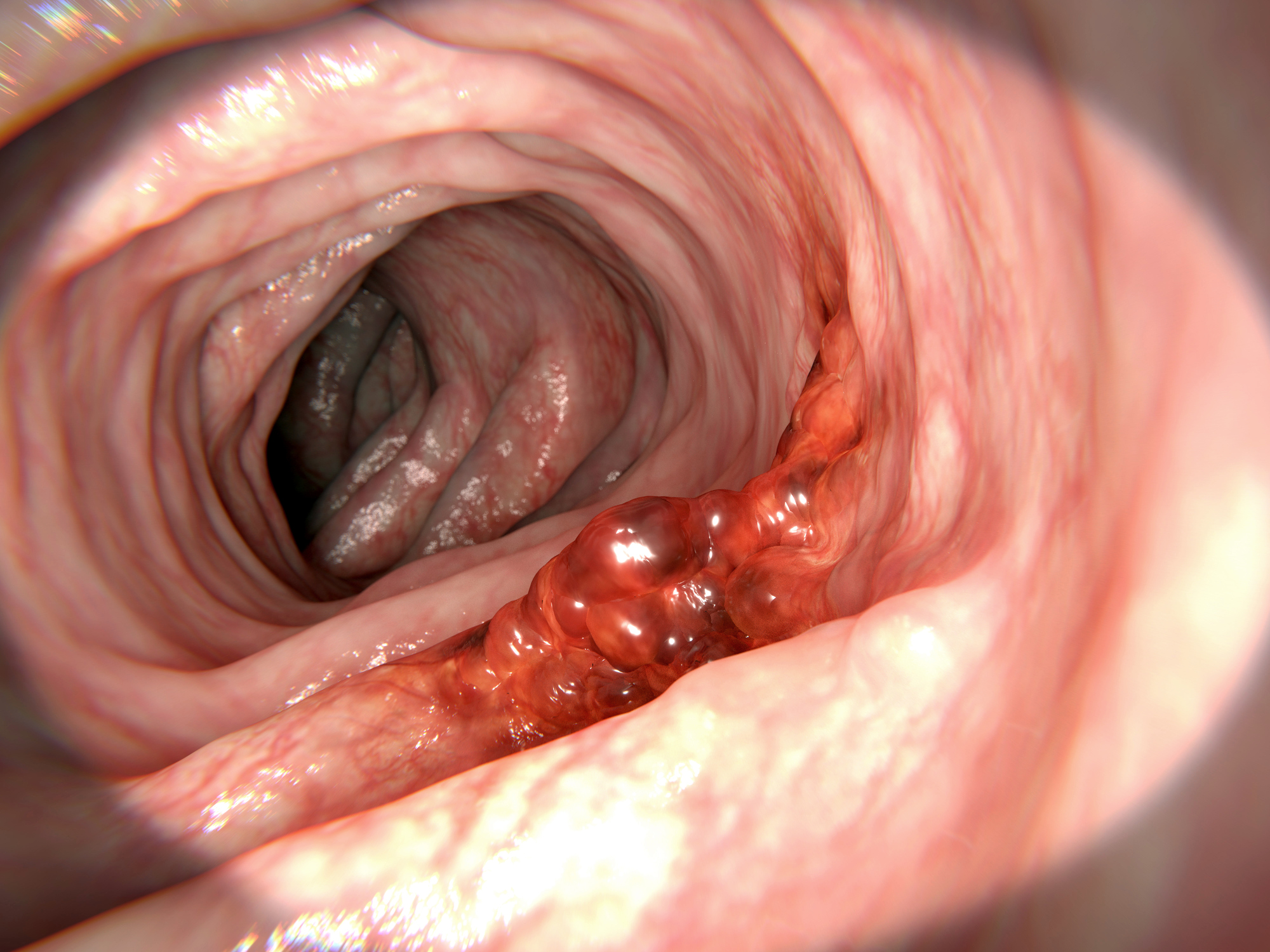
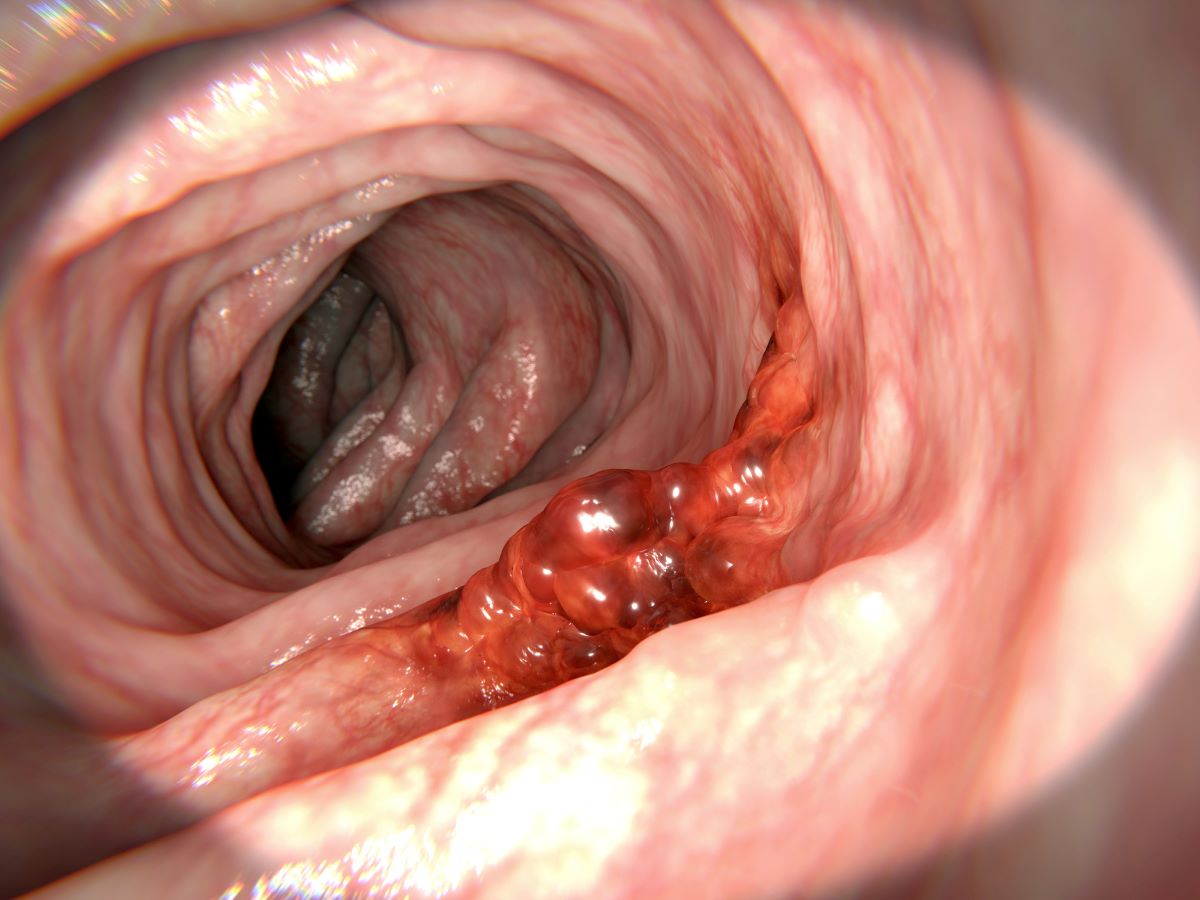
This 30 minute session will provide you with information on the presentation of colorectal cancer, particularly looking at the reasons behind late presentation and the implications of this. Diagnostic and screening investigations are explored, and next steps following referral to the cancer pathway are discussed.
This course was developed in partnership with UCLH Cancer Collaborative.


Editorial and content decisions were made solely by the RCGP.

Developed in collaboration with the Intensive Care Society, this webinar allows you to hear from the multi-professional team in Intensive Care to understand some of the rehabilitation needs of patients post-COVID-19 critical illness. The webinar covers:
- The challenges around recovery of communication and swallowing post ICU.
- The psychological impact of COVID-19 recovery and what to look out for.
- The breathless ICU survivor post coronavirus infection - heart, lungs or muscle as the problem?

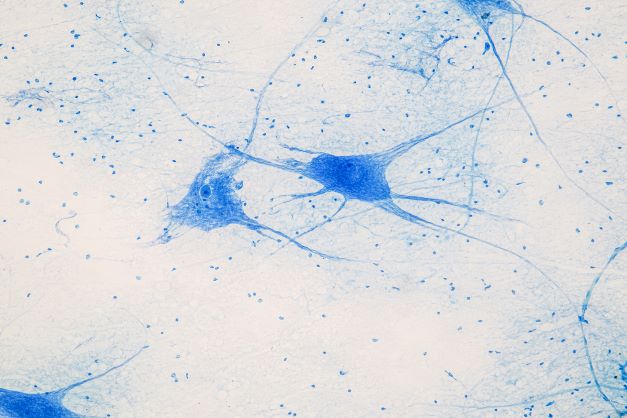
Dr Sally Higginbottom talks to Dr Morounkeji Ogunrinde, a GP in north central London and a Medical Education Fellow at UCL who is leading on a project which aims to diversify teaching in dermatology so that students, clinicians, nurses can recognise normal skin as well as common and complex skin conditions in darker skin tones where there has been a gap in the availability of learning resources within this population of people.
Within the podcast, the need to understand darker skin tones to offer the kind of care needed, to avoid delay in diagnosis and provide the most suitable treatments is discussed along with a range of different skin conditions including eczema, psoriasis, alopecia, and skin cancer, how they appear within more pigmented skin and how they should be treated. Useful resources for further learning and signposting to helpful organisations are also highlighted.


The crux of the diabetes hub revolves around the 2022 updates to the National Institute for Health and Care Excellence (NICE) guidelines on the management of people with type 2 diabetes. Courses of 15-30 minutes explain the change in emphasis from a target-driven and glucocentric approach towards a greater focus on cardio-renal risk reduction. This shift in focus places the assessment of current and future cardiovascular risk at the centre of treatment. There are courses on the challenges of polypharmacy in diabetes, lifestyle modification, the low GI diet in the context of diabetes and the NHS Diabetes Prevention Programme.


This course explores the range of eating disorders and how patients affected by them may present to their GP. It offers practical advice to enable clinicians to assess, manage and monitor such patients and know when to refer and when to be concerned.
This course is FREE to RCGP members and can be purchased by non-members.


This Update consists of five modules covering new and changing knowledge on:


This Update consists of five modules covering new and changing knowledge on:


This Update consists of five modules covering new and changing knowledge on:


This Update consists of five modules covering new and changing knowledge on:

This free 'taster' contains some examples of the Essential Knowledge Update (EKU) modules and Essential Knowledge Challenge (EKC) questions currently available in the full Essential Knowledge Update Programme as well as a number of EKU Hot Topics, Podcasts and Screencasts. All of the EKU Programme resources cover new and changing knowledge relevant to daily general practice, wherever you work in the UK.
The Essential Knowledge Updates and Challenges are FREE to all RCGP members, Associates, and GP registrars as part of the RCGP Membership benefit package. Non RCGP members can purchase an Annual Essential Knowledge Update Programme subscription (this includes access to the two most recently released Updates and Challenges) for £149 or an individual Update for £75 or Challenge for £55. To do so, please visit the ‘Courses and Events’ section of the RCGP website and follow the online instructions to complete your registration and booking for these courses. Access to the Hot Topics, Podcasts and Screencasts is free for ALL users.
Access to this course is Unrestricted.
For more information, contact us at eku@rcgp.org.uk.


Fetal Alcohol Disorders are a common group of neurodevelopmental abnormalities caused by prenatal alcohol exposure. A diagnosis remains challenging due to a lack of access to neurodevelopmental pathways and training in how to obtain accurate alcohol histories in pregnancy. Use of biomarkers and other definitive means of ascertaining exposure is at a research stage only. Up to one in twenty schoolchildren in the UK may be affected. Early recognition and treatment can lead to significant improved outcomes.

Why does primary care need to know about women’s health?
The 2022 women’s health strategy showed that women spend a significantly greater proportion of their lives in ill health and disability compared to men; a majority of women who responded to the survey felt that there had been times when their voices were not listened to when accessing healthcare. Specific concerns were that symptoms were not taken seriously, that significant self-advocacy was needed to reach a diagnosis, and that there were limited opportunities to discuss the possible treatments. There are a variety of medical needs and life stages which are specific to women, including cervical and breast screening, dysfunctional menstruation, the need for contraception, care during pregnancy and the postnatal period, and management of the menopause. Breast cancer, which is vastly more common in women than in men, is the commonest UK cancer, with two other female specific cancers (uterus and ovary) listed in the 20 most common UK cancers. Cancers of the cervix and vulva are less common (with cancer of the cervix reducing in incidence due to HPV vaccination), but it remains important that we maintain a high index of suspicion for symptoms which could represent a malignancy of any part of the female tract.
This hub concerns illnesses and life stages which are relevant to those of the female sex, and so the words woman/women/female and the pronouns she/her are used throughout the resources. Some of our patients for whom these illnesses and life stages are relevant will have a gender identity which is not female. Their chosen pronouns should be respected and used.
Women’s health eLearning
This hub contains courses which cover the main female cancers – endometrial, cervical, vulval and ovarian, as well as information about prevention of, and screening for, breast cancer. The course on endometriosis discusses the presentation and initial decision making process around whether to treat empirically in primary care or refer for a diagnosis. The decision on whether a formal diagnosis, only available via laparoscopy, is necessary at first presentation, needs to be made by the woman and her GP and will depend on a variety of factors including severity of symptoms and whether there is a current wish to conceive. There is also a course on heavy menstrual bleeding (HMB) which starts from the assessment of a patient with HMB and discusses the current guidelines and how to assess the risk of endometrial pathology and use this to make decisions about whether to treat empirically, investigate in primary care, or refer at first presentation.
The course on contraception covers all currently available methods and uses an interactive approach, case studies and videos to provide education about the mode of action and efficacy of each method, the common myths and how to refute them, and broader issues which women seeking contraception may want to consider. Concepts such as quick-start and bridging contraception are also discussed. The menopause and hormone replacement therapy (HRT) is covered in a module aimed at generalists which discusses the identification and management of the menopause and perimenopause, what women need to know about HRT and how to start it, as well as the specific features that apply to women with premature ovarian insufficiency (POI), many of whom will need referral to secondary care.
The hub also contains a variety of podcasts. Some of these cover the same subjects as the courses – a podcast sometimes allows more in depth discussion of an aspect of care where management may not be clear-cut; where there is a podcast and a course, they usually cover different facets of the condition and so it is worth accessing both resources. There are also podcasts on subjects which do not have a course on the hub, such as influenza (flu) vaccination in pregnant women, and women’s health and migraine.
References:


This course aims to educate GPs about how we can improve asthma outcomes whilst reducing the carbon footprint of inhaler prescribing. It will outline opportunities to improve patient disease control and optimise inhaler device prescribing and will signpost to step-by-step quality improvement tools to implement this work in practice. For GPs based in England, completing this course will support achievement of the Investment and Impact Fund criteria on respiratory care and sustainability from April 2022 - April 2024. Much of the information about greener inhaler choices also applies to patients who use inhalers for other reasons, e.g. COPD.
An educational grant was received from NHS England for the production of the course. Editorial and content decisions were made solely by the RCGP.





This course covers the investigation of patients who present with lower gastrointestinal symptoms that are likely to be Irritable Bowel Syndrome, the red flags to look out for, how to make a confident diagnosis in primary care, and how to manage patients in line with NICE CG61.
Editorial and content decisions were made solely by the RCGP.


Inflammatory Bowel Disease (IBD) is a life-long relapsing-remitting condition affecting the bowels and many other parts of the body. Symptoms can develop at any age, and can mimic those of many other conditions. This newly designed toolkit allows users to learn about IBD through different formats including three bite-sized NUBs - New Useful Bits, a 30 minute module and a recorded podcast. The toolkit provides tips to help those working in Primary Care suspect, investigate, and refer patients for appropriate investigations. It also summarises key information to consider when supporting patients living with IBD

Available until 12 February 2026.
Lifestyle medicine is a global medical discipline, teaching clinicians behavioural techniques to support patients with some of the root causes of ill health. These include assessing and addressing financial stress, poor mental wellbeing, social isolation, inactivity, poor quality food, poor sleep/shift work and harmful substances or behaviours such as smoking, alcohol and harmful tech use. Lifestyle medicine provides one-to-one assessment and support but requires wider public health population level interventions. The aim of these interventions is to prevent, treat and potentially reverse ill health whilst minimising the need for long-term medications.
This One Day Essentials lifestyle medicine conference will describe lifestyle medicine practice and how it is applied in everyday clinical practice for GPs. The conference will cover the RCGP GP with extended role in lifestyle medicine pathway, the evidence for lifestyle medicine and where it sits with population and public health, how this practice can be used to reduce health inequity, avoid over-diagnosis and over-prescribing. Speakers will also address how lifestyle medicine practice can be more sustainable medicine, can deliver person-centered care and recognises the wider aspects of wellbeing such as art and nature.
Learning objectives
- Define lifestyle medicine
- Describe how public health and population health interventions can be complemented by lifestyle medicine’s one-to-one support
- List the evidence for lifestyle medicine interventions
- Define over-diagnosis and over-prescribing and how lifestyle medicine can address these challenges
- Describe how lifestyle medicine can be used to address inequity
- List how lifestyle medicine can improve sustainable practice
- Describe how art and time in nature can improve health outcomes
Topics
- What is lifestyle medicine and introduction to RCGP GP with extended role in lifestyle medicine
- The evidence for lifestyle medicine and how it works with public and population health
- Lifestyle medicine is sustainable medicine and can improve planetary health
- Social prescribing, physical activity, green spaces
- Lifestyle medicine and health inequalities
- The challenge of over-diagnosis and over-prescribing; can lifestyle medicine help?
- How art and music can improve health
Conference chair
Dr Ellen Fallows - GP and expert in obesity and lifestyle medicine

Bronze sponsor
Symprove sponsored this conference. Editorial and content decisions were made solely by the RCGP.

Lipoedema is an adipose tissue disorder. It causes bilateral symmetrical enlargement of the lower extremities, which can lead to significant distortion of the hip to waist ratio. Lipoedema can also affect the upper extremities, but this is less common. Lipoedema is often diagnosed late (or not at all) and may be confused with obesity or lymphoedema. This course describes the presentation, pathophysiology, diagnosis and management of lipoedema in primary care.
This course was developed in partnership with Lipoedema UK and has been endorsed by the Royal College of Nursing.

The primary prevention of cardiovascular disease (CVD) is one of the most important aspects of primary care and is particularly important for those patients with familial hypercholesterolemia (FH). As the prevalence of heterozygous FH in the UK population is approximately 1 in 250, a typical practice with 10,000 patients might have up to 40 patients with a significantly increased risk of premature heart disease. The condition is significantly underdiagnosed, and the 2017 NICE FH guideline has recommended case finding in primary care using electronic records as an acceptable and highly cost effective method for individual practices to identify patients who so far have not had the benefit of treatment. The NHS 2019 long-term plan has set an ambition to identify 25% of the predicted FH patients, and achieving this will depend heavily on GP input.
The course consists of two modules. Module 1 provides GPs and other Health Care Professionals with information about the causes and consequences of FH, how they can identify those in their practice most likely to have FH, and how these patients and their relatives should be managed. Module 2 covers the genetic causes of FH in more detail, the ongoing study into identifying FH in infants, and describes novel lipid-lowering agents.
A grant was received from Health Education England by the North Thames Genomic Laboratory Hub (based at GOSH) and South East Genomic Medicine Service Alliance for the production of this resource. Editorial and content decisions were made solely by the RCGP.
![]()
![]()
![]()
![]()
Available until 20 November 2025.
The 29th Managing addictions in primary care conference took place on Thursday 16 and Friday 17 January 2025 in Manchester.
This conference is the largest event in the UK for GPs, shared care workers, nurses and other primary care staff, specialists, commissioners and researchers interested in and involved with the Management of people with Addictions in Primary Care (MAPC). It is now in its 29th year with a loyal following but always attracts new faces from primary care. As usual, we will be covering important issues for the field including drug and alcohol problems including both a beginners guides as well as more specialist issues, managing harms from behavioural addictions such as pornography.
With alcohol and drug related deaths still at an all time high, a harm reduction approach is paramount along with tackling stigma (so people don’t shy away from help).
We are really excited to go back on tour – yes we will be at an excellent iconic venue, The Lowry in the Quays area of Manchester, with plenty of room to make the best of workshops, interaction, networking and learning from each other. This includes showcasing great organisations such as Camerados, Fallen Angels Dance Theatre and The Spider Project, which have been ongoing for many years providing exceptional services for people in recovery from addiction.
Learning objectives:
• Increase understanding of current interventions for the prevention, assessment and treatment of alcohol and other drug problems
• Increase understanding of what interventions are possible to deliver in Primary Care and what require specialist help
• Increase knowledge of drug and alcohol policies in the UK and how they are implemented in primary care
• Increase knowledge of links between multiple needs, health inequalities and drug and alcohol use


Available until 20 November 2025.
The 29th Managing addictions in primary care conference took place on Thursday 16 and Friday 17 January 2025 in Manchester.
This conference is the largest event in the UK for GPs, shared care workers, nurses and other primary care staff, specialists, commissioners and researchers interested in and involved with the Management of people with Addictions in Primary Care (MAPC). It is now in its 29th year with a loyal following but always attracts new faces from primary care. As usual, we will be covering important issues for the field including drug and alcohol problems including both a beginners guides as well as more specialist issues, managing harms from behavioural addictions such as pornography.
With alcohol and drug related deaths still at an all time high, a harm reduction approach is paramount along with tackling stigma (so people don’t shy away from help).
We are really excited to go back on tour – yes we will be at an excellent iconic venue, The Lowry in the Quays area of Manchester, with plenty of room to make the best of workshops, interaction, networking and learning from each other. This includes showcasing great organisations such as Camerados, Fallen Angels Dance Theatre and The Spider Project, which have been ongoing for many years providing exceptional services for people in recovery from addiction.
Learning objectives:
• Increase understanding of current interventions for the prevention, assessment and treatment of alcohol and other drug problems
• Increase understanding of what interventions are possible to deliver in Primary Care and what require specialist help
• Increase knowledge of drug and alcohol policies in the UK and how they are implemented in primary care
• Increase knowledge of links between multiple needs, health inequalities and drug and alcohol use


Available until 20 November 2025.
The 29th Managing addictions in primary care conference took place on Thursday 16 and Friday 17 January 2025 in Manchester.
This conference is the largest event in the UK for GPs, shared care workers, nurses and other primary care staff, specialists, commissioners and researchers interested in and involved with the Management of people with Addictions in Primary Care (MAPC). It is now in its 29th year with a loyal following but always attracts new faces from primary care. As usual, we will be covering important issues for the field including drug and alcohol problems including both a beginners guides as well as more specialist issues, managing harms from behavioural addictions such as pornography.
With alcohol and drug related deaths still at an all time high, a harm reduction approach is paramount along with tackling stigma (so people don’t shy away from help).
We are really excited to go back on tour – yes we will be at an excellent iconic venue, The Lowry in the Quays area of Manchester, with plenty of room to make the best of workshops, interaction, networking and learning from each other. This includes showcasing great organisations such as Camerados, Fallen Angels Dance Theatre and The Spider Project, which have been ongoing for many years providing exceptional services for people in recovery from addiction.
Learning objectives:
• Increase understanding of current interventions for the prevention, assessment and treatment of alcohol and other drug problems
• Increase understanding of what interventions are possible to deliver in Primary Care and what require specialist help
• Increase knowledge of drug and alcohol policies in the UK and how they are implemented in primary care
• Increase knowledge of links between multiple needs, health inequalities and drug and alcohol use


Available until 1 April 2026.
Long COVID-19 presents a significant challenge in general practice, with patients experiencing a broad and often debilitating range of symptoms. GPs are at the frontline of care, yet the evolving nature of research, varied presentations, and complexities of management can make it difficult to navigate. This webinar aims to empower and upskill GPs with the latest evidence-based understanding of Long COVID-19, its pathophysiology, and practical approaches to patient care. The session will feature expert-led talks, followed by interactive Q&A discussions.
Learning Objectives:
- Recognise the key presentations and symptomatology of Long COVID-19 encountered in general practice.
- Understand the current research and evidence-based insights into the pathophysiology of Long COVID-19.
- Manage common Long COVID-19 symptoms, including fatigue, brain fog, and breathlessness, using practical, patient-centred approaches.
- Address more complex Long COVID-19 manifestations such as mast cell activation syndrome, POTS, and pleuritic chest pain.
- Explore emerging and debated topics in Long COVID-19 management, including microclots, vagal nerve dysfunction, hyperbaric oxygen therapy, supplements, and Low Dose Naltrexone.
- Discuss prognosis and expected outcomes to better support and counsel patients on their recovery journey.


Available until 14 April 2026.
Approximately 20% of men will not live to see retirement in the UK, often due to a reluctance to seek medical help, particularly for sexual or mental health concerns. Delaying care can lead to more serious and challenging health issues. As GPs, we are often the first point of contact and have a vital role in improving men's health outcomes.
The RCGP One Day Essentials Men’s health conference offers valuable insights tailored for GPs, providing practical advice and resources to enhance patient care. Expert speakers will address key topics and share strategies to help you confidently manage common men’s health concerns in your practice. Based on feedback from previous years, the event is designed to be as relevant and beneficial as possible. While staple topics such as prostate cancer and LUTS remain, this year introduces new discussions on male fertility and testicular conditions.
Topics include:
- Male fertility in primary care
- Erectile dysfunction
- Male pattern hair loss
- Testicular abnormalities
- Lower urinary tract symptoms (LUTS)
- Genital dermatology in men
- Prostate cancer
Conference Chair:
- Dr Anand Patel, GP Partner, Secretary to the Primary Care Testosterone Group and a trustee of the Sexual Advice Association
Platinum Sponsor:
We are the leading prostate cancer charity in the UK and the largest funder of research into prostate cancer. Our ambition is to save and improve the lives of men affected. 1 in 8 men will get prostate cancer. We offer free education and professional development for healthcare professionals. Whether it’s online learning, resources, courses or events, we’re here to help you meet your educational and professional development needs
Gold Sponsor:
testhim is a pioneering platform dedicated to addressing the often-overlooked issue of male fertility. Founded by Ian Stones, Michael Close, and Toby Trice—leaders in the field with over four decades of combined experience—testhim aims to bridge the gap in fertility education and support for men. By offering a free questionnaire, men can quickly discover how their lifestyle and health history may be affecting their fertility, with instant recommendations for health, lifestyle changes, and advanced fertility tests. In collaboration with LogixX Fertility and leading clinics, testhim provides innovative diagnostics such as oxidative stress testing and sperm DNA fragmentation, while also offering high-quality fertility supplements and services. The platform empowers men to take control of their reproductive health, making advanced fertility care more accessible and transforming the male fertility landscape.


This collection of resources is specifically designed to support the mental health and wellbeing of the GP workforce and the healthcare community at large. The resources aim to help with the mental and physical state of the workforce, address current and future challenges, allow healthcare professionals to feel supported and therefore provide better care to colleagues and patients. By giving the members of the primary care team the tools to recognise signs of burnout, PTSD and low mood, and subsequently introduce them to techniques to manage these, these resources aim to prevent further reduction of the workforce due to ill health.
A grant was received by CHSA (COVID-19 Healthcare Support Appeal) for the production of this hub. Editorial and content decisions were made solely by the RCGP.

The climate emergency is a health emergency. Primary care accounts for approximately 23% of NHS England’s emissions footprint; this hub contains courses to help GPs who want to advocate for climate change mitigation and adaptation.
Most primary care emissions are associated with prescribing; the first course ‘Introduction to sustainable healthcare’ gives an overview of the links between planetary health and our patients’ health and introduces “Delivering a net zero National Health Service”, the report which sets emissions targets for the NHS. It discusses how we can promote initiatives such as active travel and social prescribing, ways to reduce overprescribing and overdiagnosis, and the contributions that diet, exercise and patient empowerment can make to good clinical care and reduction of emissions.
Inhalers make up a large percentage of clinical emissions and the second course, ‘High quality and low carbon respiratory care’ discusses changes that we can make. Moving from metered dose inhalers (MDIs) to dry powder inhalers (DPIs) reduces emissions and often benefits patients, who may find DPIs easier to use, improving adherence. For patients who cannot move from an MDI, changing the brand or dose per puff can also reduce greenhouse gases from their inhaler. The importance of good asthma control is also discussed, with reference to the National Review of Asthma Deaths (NRAD). References such as Greener Practice can help practices to improve asthma care whilst reducing emissions and meeting the requirements of the Investment and Impact Fund (IIF).
The final eLearning course, ‘Understanding non-clinical carbon and general practice’ considers the four key areas in which change can be made – energy, travel, business services and medical and office goods and equipment. Understanding the energy hierarchy and the circular economy, reducing waste and making environmentally responsible choices may also improve the health of primary care staff and save money for the practice. The NHS Net Zero Supplier Road Map is explained, as is how to draw up a practice green action plan and make better procurement choices.
The hub also links to the population and planetary health topic guide in the RCGP curriculum, and has a webinar presented by the RCGP’s faculty climate and sustainability group, which shares practical ideas that could help GPs to get started in sustainable healthcare.


In an average practice of 10,000 patients, approximately 5 patients will be living with and beyond a diagnosis of neuroendocrine neoplasm (NEN). This course aims to increase the primary care clinician’s knowledge of neuroendocrine neoplasms, and thereby improve the time to diagnosis and management of patients with NENs. Over the course of these two modules we will discuss the types of NENs, common presenting symptoms, the challenge their diagnosis presents, and the importance of primary care input following diagnosis.
An educational grant was received from Neuroendocrine Cancer UK for the production of this resource. Educational content was supported by NCUK but final editorial and content decisions were made by the RCGP.


Nocturia is a common symptom, especially in older adults. It is commonly framed as a lower urinary tract symptom and we frequently think of a limited range of aetiologies (usually benign prostatic hypertrophy and overactive bladder). However, for many patients, nocturia is due to one or more other conditions including endocrine causes, drug side effects and nocturnal polyuria.
An educational grant was received from Ferring Pharmaceuticals for the production of the course. Editorial and content decisions were made solely by the RCGP.

Patients frequently present to general practice with a range of undifferentiated symptoms that may or may not signify serious disease.
This course helps GPs to make sense of the early symptoms that could be explained by pancreatic cancer. Using video-based scenarios, it reviews the patterns of symptoms that emerge over time, which can suggest a serious underlying diagnosis, and sets out an approach that GPs can take to ensure appropriate and timely investigation and follow-up in cases of diagnostic uncertainty.
Pancreatic cancer is more prevalent than is often recognised and earlier detection of symptoms will improve outcomes for patients.
This course has been developed in partnership with Pancreatic Cancer Action.

The aim of this course is to raise awareness of post-polio syndrome, with a particular focus on its presentation and recognition by health professionals. The physiology behind the symptoms is explored, and guidance is given on management strategies.
This course was developed in partnership with British Polio Fellowship. The course is FREE to RCGP members and available for purchase by non-members on the RCGP website.

This toolkit contains five NUBs, designed to cover the key areas related to cancer in primary care. The majority of patients who are diagnosed with cancer present with non-specific symptoms, rather than clear red flags; the early diagnosis NUB covers the factors which slow down diagnosis for these patients, and how to address them on an individual and systems level. Two NUBs will discuss pre-cancer issues (screening and smoking/vaping), and the final two cover the patient journey after diagnosis. With more patients than ever surviving cancer, the survivorship NUB gives some ideas for holistic primary care for this cohort, and the end of life NUB talks about the principles of providing good end of life care. An extensive resources list signposts to other eLearning on this subject and to more detailed information on symptom control, commissioning, and how services can vary by country of the UK.

Motor neurone disease, with its most common form amyotrophic lateral sclerosis, is a group of progressive and fatal degenerative conditions of both upper and lower motor neurons. Incidence is 1.5 per 100,000 people per year, with a prevalence worldwide of 6 per 100,000. This screencast reminds all members of the primary care team of the most common symptoms and red flags to aid early diagnosis and referral.
An educational grant was received from Motor Neurone Disease Association for the production of this screencast. Editorial and content decisions were made solely by the RCGP.


This module will look at the issues in screening for the LGBTQ+ population. This group consistently has a lower attendance for cancer screening. Having discussions about screening and how non-attendance can be followed up is covered, along with best practice for the cervical smear process in trans men and non-binary people with a cervix. Information is provided on who needs to be screened, to ensure appropriate cancer screening is achieved in the trans population. The need for STI screening is also highlighted.
An educational grant was received from the Government Equalities Office for the production of the course. Editorial and content decisions were made solely by the RCGP.


This eLearning screencast discusses the DeSTRESS project, which was set up to understand the challenges facing GPs who see patients with mental distress relating to poverty. The screencast explains some of the evidence linking poverty to poor mental health and discusses some of the difficulties that GPs may face when dealing with such patients. It then goes on to give some consultation tips that we can use and ways to make a small difference from one consultation to the next. Finally it reminds us that we are human too and that we need to look after ourselves in order to be able to help our patients.
An educational grant was received from the University of Exeter for the production of the screencast. Editorial and content decisions were made solely by the RCGP.



Type 2 diabetes is an increasingly common and progressive disease, the progression of which can sometimes be paused or even reversed using a low glycaemic-index (GI diet). Many patients with type 2 diabetes are on multiple drugs, yet are still not well controlled. This module describes the use of a low GI diet as an adjunct treatment for diabetes, using a case study of a real patient registered at the author's practice. The physiology and evidence behind a low glycaemic-index diet are described, as well as how to implement it in real life.
An educational grant was received by Diabetes.co.uk for the production of the course. Editorial and content decisions were made solely by the RCGP. The course is free to RCGP members.


Available until 17 December 2025.
GPs are the first port of call for women’s health issues. We manage the majority of them without recourse to secondary care, even though the amount of time that medical school and vocational training devotes to subjects such as contraception and the menopause can be variable. When we do refer, our patients wait for many months or years, during which we manage symptoms and answer our patients’ questions.
In this One Day Essentials conference, Dr Toni Hazell and a group of leading speakers will focus on essential information, latest evidence, practical tips and take-home messages to help improve practice and patient outcomes. The primary care perspective will be foremost in all of the talks, with consideration of the real-life decisions that we make every day whilst working in an under-resourced system. There will be ample opportunity for questions.
Learning Objectives:
- To gain confidence in the management of women’s health issues in primary care, and knowledge of when referral is appropriate.
- To understand the updated NICE guideline on menopause and how to explain complex issues of risks and benefits to women contemplating HRT, as well as being aware of the British Menopause Society guidance on unscheduled bleeding on HRT and how this might affect your referral decisions.
- To understand how to manage suspected endometriosis in primary care and how decisions on referral should be individualised depending on factors such as symptom severity and desire to conceive.
- To be updated on contraception and the latest thinking in PCOS.
- To be aware of the NICE guidelines on familial cancer risk and know how to manage a patient who presents with concerns about genetic risks of cancer.
- To be able to talk to women holistically throughout their life and give sensible advice when asked about lifestyle and complementary medicine.
Topics include:
- Menopause update: What NICE did and did not say in 2024?
- Bleeding on HRT
- Contraception cluedo: Update your contraceptive knowledge for 2025
- Endometriosis
- Familial cancer
- PCOS
- Holistic women's health throughout the life cycle
Conference chair
Dr Toni Hazell, GP and RCGP eLearning fellow