Acute Kidney Injury toolkit
We have developed this toolkit to disseminate learning highlighted from AKI case notes reviews, part of the RCGP AKI Quality Improvement project.
AKI and Quality Improvement
There is evidence that current mechanisms for improving safety and quality do not realise their full potential, for example, Audit and significant event analysis as part of Annual NHS appraisals.
There is a recognised need for quality improvement activities to help:
- Address system factors impacting on patient safety
- Aggregate data to encourage learning and improvement within and across organisations
- Involve patients and carers
By focusing on AKI as a lens through which we can shift away from a single disease framework and improve patient safety for patients, the opportunity arises to drive quality improvements in:
- medical safety
- safer transitions of care
- safety for vulnerable patients.
Within its Patient Safety Domain, NHS England established the Think Kidneys Programme through which a number of national levers have been introduced to improve the prevention, detection and management of AKI.
Principles underpinning AKI Quality Improvement
Addressing a major NHS priority, the RCGP Quality Improvement Project aims to be an exemplar of how to embed improvement methods in routine practice and provide a platform to realise the Triple Aim. The project aims to provide an example of how to improve patient safety in primary care and across the interfaces of care. In doing so, it hopes to mitigate safety risks that are common to multiple problems beyond AKI. Key principles underpinning AKI Improvement work are:
- Develop evidence based interventions grounded in an in-depth understanding of routine clinical practice
- Navigate the challenge of overdiagnosis: Maximise clinical utility of AKI as a driver of quality and safety whilst minimise treatment burden for patients (and corresponding unnecessary clinician workload)
- Support system resilience through person-centred collaborative working across the interfaces of care
Approaches to Quality Improvement
This section outlines two complementary approaches to supporting improvement in everyday clinical practice:
The QI Wheel for Primary Care
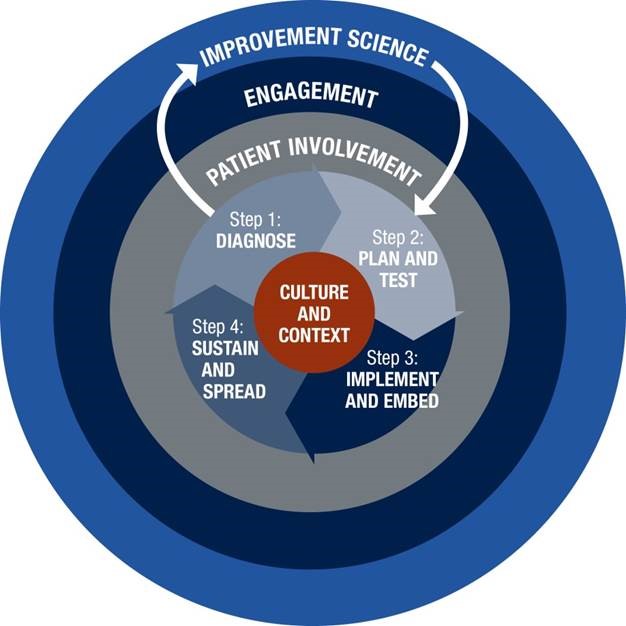
Informed by Institute for Healthcare Improvement methodology, the RCGP has developed the Quality Improvement Guide for General Practice. Key resources include:
- Process Mapping - creates a visual representation of a process enabling waste and areas for improvement to be identified
- Fishbone diagram - used to identify the root causes of a problem (also called a cause and effect diagram)
- Model for Improvement and PDSA (Plan Do Study Act) - proposes three questions to ask prior to testing a change using a PDSA cycle
Systems Thinking for Everyday Work (STEW)
The ‘Systems Thinking for Everyday Work (STEW)’ approach embraces a Safety-II perspective and is informed by the principles laid out in the white paper written by the European Organisation for the Safety of Air Navigation. A Safety-II perspective emphasises that healthcare organisations ‘might improve their ability to learn from past experience by studying not only what goes wrong (i.e. represented by incidents), but also by considering what goes right (i.e. by learning from everyday clinical work).'
The STEW principles act as a framework for teams to explore everyday work by obtaining multiple perspectives to understand how and why people adapt their ways of working to cope with the system conditions they face (such as competing goals or availability of information).
Access slides from the ‘Adopting a ‘systems approach’ to QI and safety work in frontline general practice’ session at the RCGP Annual Conference 2018.
Strategies for AKI improvement - AKI Case Note Review Templates
As part of the AKI Quality Improvement project, GP practices undertook case note reviews for patients who have generated an AKI alert and are now being looked after by in primary care.
24 general practices across England and Scotland conducted and reflected on case note reviews, conducting 148 in total.
Resonating with a Safety-II perspective, the AKI case note review templates are structured to identify patient safety issues, highlighting learning opportunities across care interfaces (Primary/Secondary; In/Out of Hours). The questions aim to promote learning from real-life AKI cases, rather than audit or criticise current practice.
RCGP AKI case note templates (800 KB DOCX)
- AKI Safety Template 1 is designed to support case note review of patients who have generated an AKI Warning Stage Test Result in primary care
- AKI Safety Template 2 is designed to support case note review of patients who have had a hospital admission complicated by AKI
- AKI Safety Template 3 is designed to aid reflection and learning through a summary of cases in order to create action plans for practice-level improvements in future care.
AKI Shared Learning from case note reviews – a summary of the key learning points and suggested actions for improvement
Strategies for AKI improvement - Further resources
The following resources may aid understanding of factors that underpin incorporation of AKI-related work into routine care. They may support practice-based discussions and generate discussion and learning across the interfaces of care:
- Practice Based Learning using STEW Framework: Learning generated from across the 24 participating practices and an example from a practice in Scotland: the Systems Thinking for Everyday Work (STEW) framework can generate learning on how to improve the management of AKI.
- Shared learning through Process Mapping and Fishbone diagrams - At the national RCGP Shared Learning Event in 2018, delegates worked in small multidisciplinary groups, undertaking process mapping to generate learning about the delivery of post-AKI care and fishbone diagrams to understand failures to respond to an AKI Warning Stage Test Result.
- Illustrated summary of presentations and exercises at the RCGP Shared Learning Event by medical artist, Dr Morium Howlader, GP.
Systems Thinking for Everyday Work: A Safety and Improvement Model for Healthcare
Resonating with a Safety-II perspective, the STEW Safety and Improvement Model offers a framework to integrate learning based on data generated through case note reviews (Work-as-done) as well as audit data (Work-as-imagined). Using the STEW principles framework can help identify key areas for improvement. These can inform discussions with relevant stakeholders to identify joint improvement targets and agreed actions (Work-as-designed). Through a participatory approach (i.e.co-development), the STEW framework aims to support a sustainable ongoing cycle of improvement grounded in an in-depth understanding of routine care.
The following links provide suggestions on how to use QI methods to: