_ RCGP Learning
Blog entry by _ RCGP Learning
Dr Dirk Pilat
Rabies (from latin ‘to rage’) is a zoonotic, mostly fatal disease caused by a neurotropic virus of the lyssavirus genus.
The disease was first described in Egypt around 2300 BCE and is currently endemic in over 150 countries, with the highest risk of exposure in Africa and Asia. Dogs are the principal host in Africa, Asia and America, but the virus can be present in other wild animals, such as bats, cats, skunks or racoons. The most common way of transmission is the bite of an infected dog or cat, though handling of infected carcasses can cause infection too.
Figure 1. 3D still
showing rabies virus by www.scientificanimations.com/is
licenced under CC
BY-SA 4.0 DEED
Worldwide, around 59,000 people die of rabies each year, mainly in Africa and Asia. In the UK there have been reportedly 26 fatalities since 1946, with the most recent in 2018. There is recent qualitative and quantitative evidence that the perceived risk of exposure to rabies for travellers is low, with vaccination often avoided due to cost implications.
Before the SARS-CoV-2 pandemic, circa 2000 people required post-exposure treatment in England per year, of which 12% were potentially exposed to the two bat species in the UK who harbour the virus. The disease remains prevalent in some countries in Eastern Europe.
After an incubation time of typically three to 12 weeks, infection with the virus can cause a slow but progressive encephalitis with early symptoms being headache, fever, and malaise. The patient may then develop the characteristic symptoms of hydrophobia, hallucinations, and features of mania before progressing to paralysis and coma. Rabies is almost always fatal, and there is currently no specific treatment other than symptom control.
Pre-exposure prophylaxis via vaccination before travelling (or for those with occupational hazards) into endemic areas is a safe and effective method of protecting people from rabies, with the Green Book recommending an individual risk assessment of potential exposure prior to travelling.
Post-exposure management should consist of wound treatment (running tap water over the wound for several minutes, washing with soap or detergent and application of a dressing with disinfectants (such as 40 to 70% alcohol, tincture, or aqueous solution of povidone-iodine) and treatment with either an accelerated course of rabies vaccine or administration of human rabies immunoglobulin. The decision about which course of post-exposure treatment to administer depends on the categories of exposure, which animal was involved and in which country the incident occurred. Advice on who to contact in a suspected case of rabies can be obtained in this table from the Green Book.
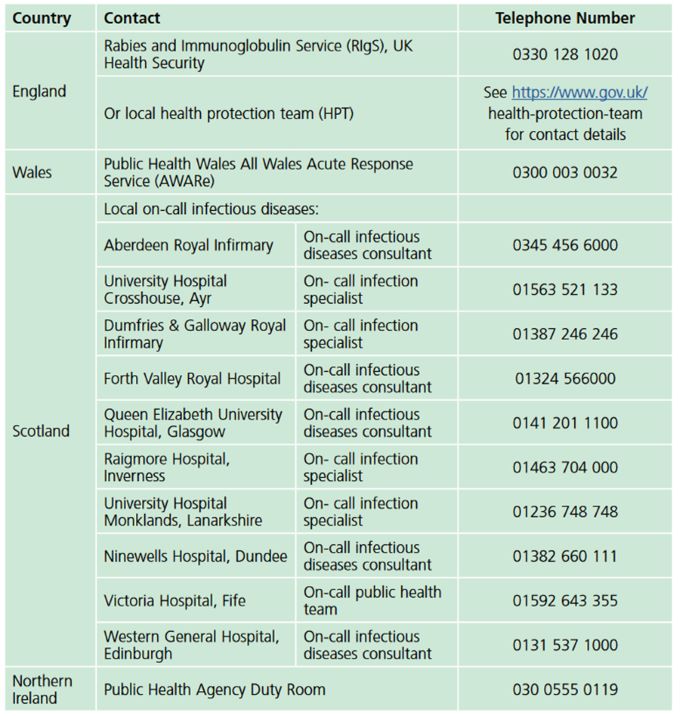
Guidance Rabies: the green book, chapter 27, p11. Contains public sector information licensed under the Open Government Licence v3.0.
 Tetanus is a disease caused by the neurotoxin produced by the bacterium Clostridium tetani. The spores of the bacterium are ubiquitous in soil throughout the world and enter contaminated wounds or minor abrasions. In low- and middle-income countries, both maternal (tetanus during pregnancy or within 6 weeks of the end of pregnancy via birth, miscarriage, or abortion) and neonatal tetanus (infection occurs via the umbilical stump) are likely significantly under-reported, but it is estimated that in 2015 about 35,000 deaths were due to neonatal tetanus and 57,000 adults were reported to have died. In high income countries, older people and people who inject drugs are the most likely to contract the disease. Migrants from countries with poor vaccination programmes can be particularly susceptible. Between 2001 and 2022, 147 cases of tetanus were reported to the UK Health Security Agency.
Tetanus is a disease caused by the neurotoxin produced by the bacterium Clostridium tetani. The spores of the bacterium are ubiquitous in soil throughout the world and enter contaminated wounds or minor abrasions. In low- and middle-income countries, both maternal (tetanus during pregnancy or within 6 weeks of the end of pregnancy via birth, miscarriage, or abortion) and neonatal tetanus (infection occurs via the umbilical stump) are likely significantly under-reported, but it is estimated that in 2015 about 35,000 deaths were due to neonatal tetanus and 57,000 adults were reported to have died. In high income countries, older people and people who inject drugs are the most likely to contract the disease. Migrants from countries with poor vaccination programmes can be particularly susceptible. Between 2001 and 2022, 147 cases of tetanus were reported to the UK Health Security Agency.Figure 2.Opisthotonus in a patient suffering from tetanus - Painting by Sir Charles Bell - 1809. In public domain.
Under anaerobic conditions the spores germinate, and the newly formed bacteria produce a highly toxic neurotoxin that is transported retrogradely along the axonal pathways, reducing motor nerve inhibition. After an incubation time of up to 21 days, localised or general spasms (such as back arching, known as opisthotonos) can occur, with trismus and ‘risus sardonicus’ being early signs. This can be associated with dysphagia due to laryngeal and pharyngeal spasms. Testing is available via wound samples or serology but should not delay treatment. The UK Health Security Agency defines a probable case as “In the absence of a more likely diagnosis, an acute illness with muscle spasms or hypertonia, and diagnosis of tetanus by a health care provider”.
Treatment requires thorough cleaning and debridement of the wound, antibiotics and in severe cases mechanical ventilation under neuromuscular blocking agents.
Fortunately, a safe and efficient vaccine exists and has been in regular use since 1961. By the 1970s the disease had almost disappeared in children under 15. These days, it is part of the United Kingdom’s routine immunisation schedule.
 Patients with tetanus prone wounds might, depending on their
vaccination status, receive a reinforcing dose of tetanus vaccine and – if
indicated – a dose of human tetanus immunoglobulin after their wound has been
thoroughly cleaned. The Green Book categorises tetanus prone wounds as:
Patients with tetanus prone wounds might, depending on their
vaccination status, receive a reinforcing dose of tetanus vaccine and – if
indicated – a dose of human tetanus immunoglobulin after their wound has been
thoroughly cleaned. The Green Book categorises tetanus prone wounds as:
- puncture-type injuries acquired in a contaminated environment and likely therefore to contain tetanus spores e.g. gardening injuries and wounds containing foreign bodies
- compound fractures
- wounds or burns with systemic sepsis
- certain animal bites and scratches - although smaller bites from domestic pets are generally puncture injuries, animal saliva should not contain tetanus spores unless the animal has been routing in soil or lives in an agricultural setting.
High-risk tetanus wounds include any of the above with either:
- heavy contamination with material likely to contain tetanus spores e.g. soil, manure
- wounds or burns that show extensive devitalised tissue
- wounds or burns that require surgical intervention that is delayed for more than six hours are high risk even if the contamination was not initially heavy.
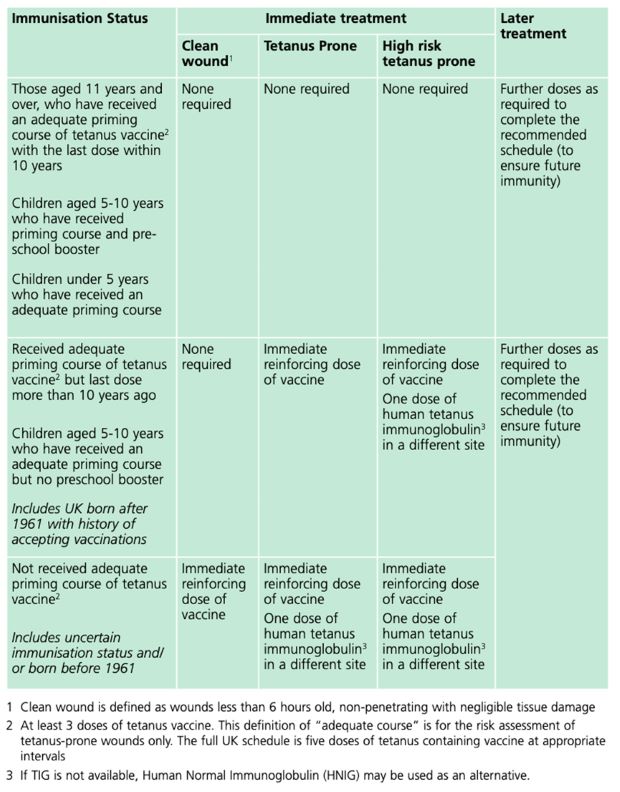
Guidance Tetanus: the green book, chapter 30, Table 30.1, p.10. Contains public sector information licensed under the Open Government Licence v3.0.
References
Marano, C et al. (2019). Perceptions of rabies risk: a survey of travellers and travel clinics from Canada, Germany, Sweden and the UK. Journal of Travel Medicine, Vol 26, Suppl 1, S3–S9, DOI: 10.1093/jtm/tay062
Singh,R et al.(2017). Rabies – epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review, Veterinary Quarterly, 37:1, 212-251, DOI: 10.1080/01652176.2017.1343516
United Kingdom Health Security Agency (2023). Guidance on the management of suspected tetanus cases and the assessment and management of tetanus-prone wounds. https://www.gov.uk/government/publications/tetanus-advice-for-health-professionals/guidance-on-the-management-of-suspected-tetanus-cases-and-the-assessment-and-management-of-tetanus-prone-wounds (Accessed 14.11.2023)
United Kingdom Health Security Agency (2023). Rabies: the green book, chapter 27. https://www.gov.uk/government/publications/rabies-the-green-book-chapter-27 (Accessed 13.11.2023)
United Kingdom Health Security Agency (2022). Tetanus: the green book, chapter 30. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1080599/Green_Book_on_immunisation_chapter_30_tetanus.pdf (Accessed 14.11.2023)
Yen, LM; Thwaites, CL (2019). Tetanus. Lancet 2019; 393: 1657–68 http://dx.doi.org/10.1016/S0140-6736(18)33131-3