_ RCGP Learning
Blog entry by _ RCGP Learning
Written by Dr Toni Hazell
Public health authorities have noted a recent rise in both measles and pertussis cases. The first three months of 2024 saw 2,793 laboratory-confirmed cases of pertussis in England (compared to 858 in the whole of 2023), with so far five known deaths, all in infants1. There have been fewer cases of measles (826 over the same time frame2), but again this is a significant increase when compared to the 212 cases seen in the last quarter of 20232.
Prior to the introduction of vaccination, both of these infections were endemic. There were 800,000 cases of measles per year in the UK3, with 120,000 cases of pertussis per year in England and Wales4. Infections and deaths fell when vaccination was introduced, but the success of vaccinations for both infections has been hindered by reduced uptake5, with pertussis also affected by immunity that wanes over time. This was illustrated by an increase in cases in 2011/12, despite sustained levels of vaccine coverage over 95%6.
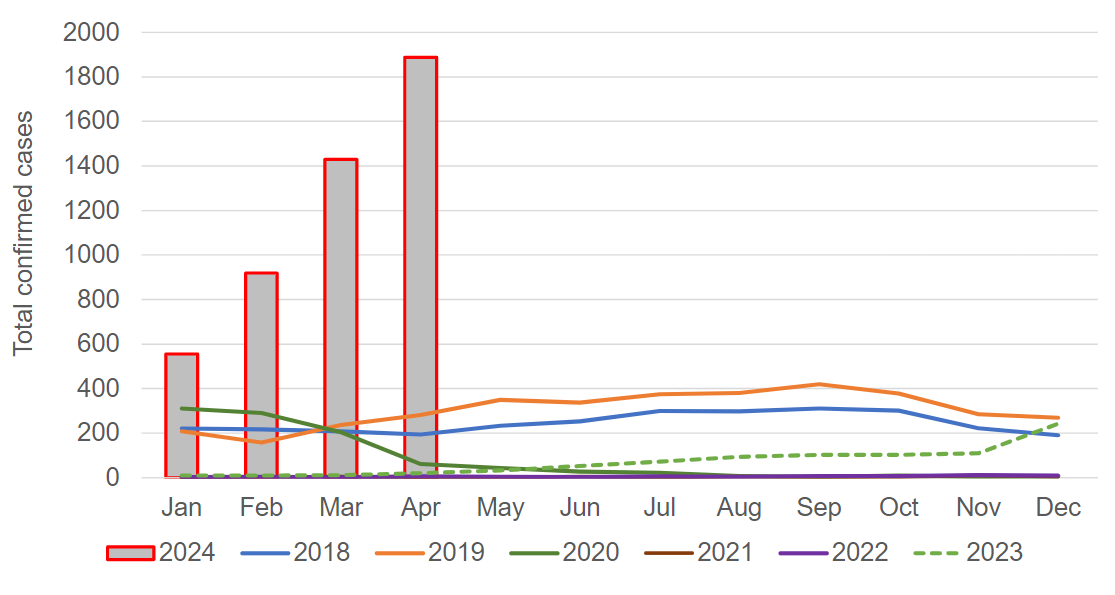
Laboratory confirmed cases of pertussis in England in 2024, compared to previous years1.
Image used under the Open Government v3.0 licence.
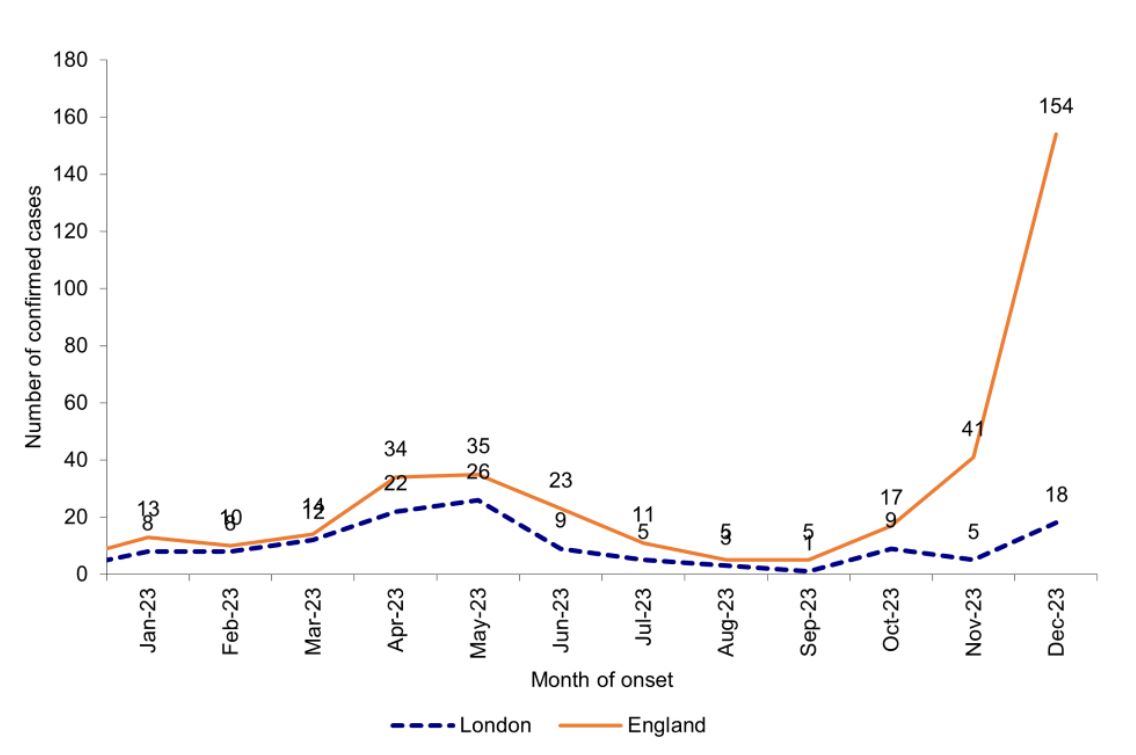
Laboratory confirmed cases of measles by month of onset of rash or symptoms reported7.
Image used under the Open Government v3.0 licence.
GPs working at the moment will not have been in clinical
practice when these infections were endemic, and so may need a reminder of how
to spot them – clinical features are outlined below. Both infections
present with a prodrome which is similar to a usual viral upper respiratory
infection; diagnosis at this point is probably less likely than when specific
features develop later on in the evolution of the illness.
Both illnesses have the potential for unpleasant complications. Patients who have had measles are more susceptible to opportunistic infection for around three years after their recovery, because the measles virus suppresses the immune response. Common complications include otitis media, diarrhoea and pneumonia. Rarer, but potentially more severe, are convulsions, encephalitis and subacute sclerosing panencephalitis. This last condition occurs on average seven years after the measles infection (but has been known up to 30 years later) – it presents with neurological symptoms and is always fatal3. Complications of pertussis include pneumonia, apnoea, seizures and encephalopathy. The strength of the cough can cause pneumothorax, abdominal hernia, rib fracture and subconjunctival haemorrhage. It is particularly risky in newborns – anyone aged under six months with suspected pertussis should be referred to paediatrics and is likely to be admitted4.
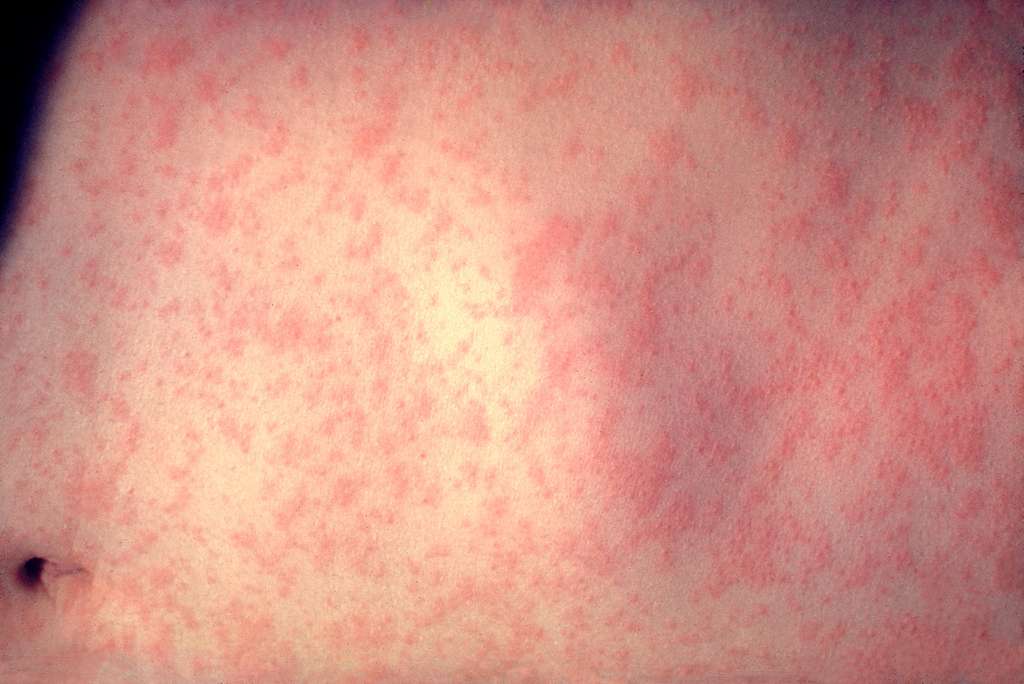
- Prodrome of upper respiratory tract symptoms and conjunctivitis, which starts 10-12 days after contracting the infection and lasts for 2-4 days, at which point a rash appears.
- Children generally feel unwell, with many references describing them as ‘miserable’.
- Fever, which peaks at around 39°C, coinciding with appearance of the rash.
- Rash with the following features:
- Starts on the face and behind the ears, before spreading down the body and finally to the extremities.
- Becomes confluent as it spreads.
- Erythematous and maculopapular.
- Lasts in total around one week, fading in any given area around five days after first appearance.
- May be less prominent (or not appear at all) in those who are immunosuppressed.
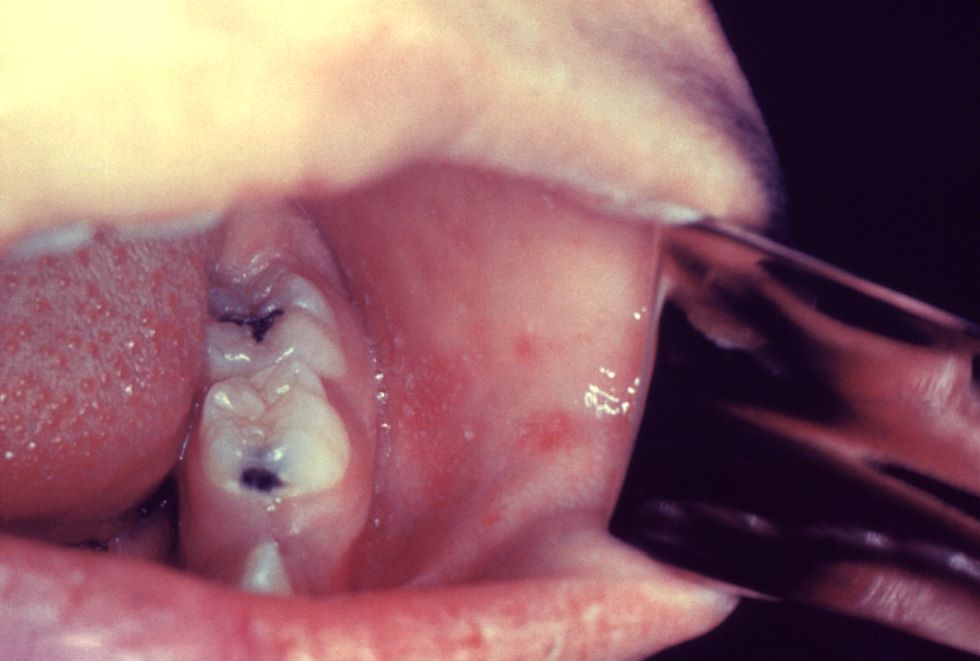
- Koplik spots on the buccal mucosa:
- 2-3mm across.
- Red, with white centres.
- Pathognomic for measles, but their absence does not exclude the condition.
- Prodrome of upper respiratory tract symptoms which starts 4-21 days after exposure (usually 7-10 days) and lasts for 1-2 weeks.
- Paroxysmal cough with the following features:
- Is worse at night and may be associated with a short expiratory burst followed by an inspiratory gasp (the ‘whoop’).
- Is violent and uncontrolled, due to attempts to bring up thick mucus. This is not always successful, so the cough may appear dry as mucus remains in the bronchial tree.
- May be triggered by cold or noise.
- Associated with post-cough vomiting, with a risk of cyanosis in children and syncope in adults.
- Cough gets worse for 1-2 weeks, stays at the same frequency for another 2-3 weeks and then gradually gets less often. Although pertussis is colloquially known as the ‘100 day cough’, the paroxysmal phase of the cough usually lasts for no longer than 10 weeks, more commonly for six weeks. There is then a convalescent phase lasting 2-3 weeks, in which the cough gradually improves. If another respiratory tract infection is contracted in the few months after pertussis, paroxysm of coughing may recur.
- There is usually no fever.
Both measles and pertussis are notifiable at the point of
suspicion – public health can be notified online, and they will then get in
touch with the patient to arrange a diagnostic test if it is thought to be
appropriate. Treatment for measles is supportive, with admission if a
complication is suspected. Pertussis can be treated with a macrolide, but this
is only effective if started within 21 days of onset of the cough. If
macrolides are contraindicated, or not tolerated, the second-line antibiotic is
co-trimoxazole. This cannot be used in pregnant women; a discussion with
microbiology would be wise if treating a pregnant woman with pertussis and a
macrolide allergy. If a patient with suspected measles or pertussis does need
admission then it needs to be made clear to the admitting team what your
suspicion is, so that they can arrange appropriate isolation. Both infections
are extremely contagious, with each person who has measles infecting 15 - 20
others3, and each person with pertussis infecting 12-17 others.10
References [all accessed 17 June 2024]
1) UKHSA. Confirmed cases of pertussis in England by month. May 2024.
2) UKHSA. Latest measles statistics published. May 2024.
3) NICE CKS. Measles. Jan 2024.
4) NICE CKS. Whooping cough. March 2024.
5) UKHSA. Pertussis: the green book, chapter 24. April 2016.
6) UKHSA. Measles: the green book, chapter 21. Dec 2019.
7) UKHSA. Confirmed cases of measles in England by month, age and region: 2023. May 2024.
8) National Foundation for Infectious Diseases. Measles. May 2024.
9) UKHSA. What is whooping cough and is there a vaccine? April 2024.
10) Harrington L, Aris E, Bhavsar A. Burden of Pertussis in Adults Aged 50 Years and Older: A Retrospective Database Study in England. Infect Dis Ther. 2023 Apr;12(4):1103-1118.
11) NHSE. NHS urges young adults to catch up on missed MMR vaccine. March 2024.
12) NHS Lothian. Over 1,300 children and young people catch-up on their MMR vaccines in Lothian. March 2024.
13) Welsh Government. Call for all parents in Wales to urgently check their children’s MMR vaccination status amid rising concerns over measles. Feb 2024.
14) HSC Public Health Agency. MMR vaccine catch-up to tackle threat of measles. Feb 2024.