_ RCGP Learning
Blog entry by _ RCGP Learning
Written by Dr Emma Nash
Phosphate homeostasis
Phosphate is routinely reported as part of a bone profile blood test. Bone profiles are commonly used to assess calcium and alkaline phosphatase levels, but abnormal phosphate – usually low – is a frequent incidental finding.
Inorganic phosphate is measured as serum phosphate. It has many functions in the body, including calcium homeostasis, cell membrane structure (as phospholipids), DNA and RNA structure, bone growth and mineralisation, intracellular energy control, neuromuscular function, and extracellular pH maintenance.1
85% of phosphate stores are in bone, mainly as hydroxyapatite. Absorbed phosphorous is converted into its inorganic form by alkaline phosphatase and enters the extracellular fluid pool. From here it moves into bones and tissues as needed. Homeostatic control of phosphate is complex, and occurs through the intestine-bone-kidney-parathyroid axis. A summary of key components, and their effects, are shown in table 1. Some of the mechanisms work to both increase and decrease phosphate levels, depending on the site of action. Intestinal absorption, renal calcitriol (1,25-dihydroxycholecalciferol - the active form of vitamin D) and parathyroid hormone (PTH) are the greatest regulators of serum phosphate levels, although oestrogens, glucocorticoids, metabolic acidosis and various growth factors (particularly fibroblast growth factor 23 – FGF23) are also involved.2
|
Table 1: Control of phosphate homeostasis1,2,3 |
||
|
Substance |
Action |
Net effect on phosphate levels |
|
Calcitriol. |
Increases phosphate (and calcium) absorption from gut. Stimulates FGF23 production. Increases phosphate (and calcium) reabsorption in renal tubules. Inhibits PTH production. |
↑ |
|
PTH. |
Increases renal phosphate excretion (increases calcium reabsorption). Stimulates calcitriol synthesis. Stimulates FGF23 production, promoting bone turnover and calcium and phosphate release. |
↓ |
|
FGF23 |
Promotes bone turnover leading to phosphate release. Inhibits PTH secretion. Reduces renal phosphate reabsorption. Reduces calcitriol secretion. |
↓ |
Intestinal absorption
Phosphorous is present in a wide variety of foods, in both organic and inorganic forms, with the latter more easily absorbed. Intestinal absorption predominantly takes place in the duodenum and jejunum, with around 60-70% of intake being absorbed. Dietary intake from animal sources is greater than from plants. Dairy and bakery products make up the majority of our dietary intake. Phosphate additives are also commonly found in processed foods as preservatives and stabilisers. The widespread presence of phosphate in dietary sources means that a healthy adult with an ‘average’ diet should not develop dietary deficiency.4
Normal phosphate levels 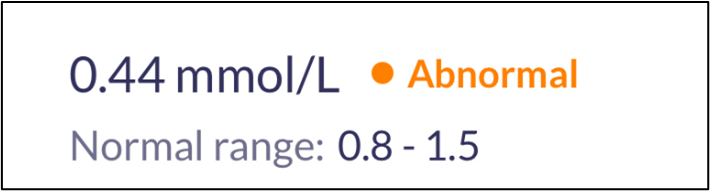
Local laboratory reference ranges may vary, but normal levels in children aged 1-16 are usually 1.3-2.4 mmol/L, and 0.8-1.5mmol/L in adults. It is important to note that serum levels may naturally be reduced by having had a recent meal (due to insulin production), in the winter due to lower vitamin D, in elderly men, and first thing in the morning. Paraproteinaemia can also cause a spurious low phosphate.5 Phosphate levels do not change significantly in pregnancy, but are higher in lactating women, infants and children. It is worth considering these factors when receiving an abnormal result, and some areas prefer a fasting phosphate test.6
Causes of hypophosphataemia
Medication
- Chronic use of antacids: these antacids form a complex with dietary phosphate, preventing its absorption. This is more prominent with those containing aluminium hydroxide, but those containing calcium carbonate can also decrease intestinal absorption of dietary phosphorous. Regular use of three months or more would normally be required to result in an intestinal deficiency, although this may be sooner in those on a low-phosphate diet (e.g. with advanced chronic kidney disease). Persistent use of magnesium-containing salts can also reduce phosphate absorption.2
- Thiazide diuretics: studies have found that hypophosphataemia is more common in patients taking thiazide (but not loop) diuretics, particularly in patients with hypokalaemia and/or a raised BMI.8
- Glucocorticoids and mineralocorticoids.
Intestinal causes
- Alcohol excess: reduced dietary intake, impaired absorption, increased urinary excretion.
- Severe malnutrition and refeeding syndrome: the shift from a catabolic state to an anabolic state can unmask a whole-body phosphate deficiency, even if the serum phosphate is normal prior to refeeding. This can produce a marked reduction in phosphate levels. This is most common in anorexia nervosa, but can also occur where malnutrition has arisen through medical problems such as cancer, alcohol excess and conditions where chewing/swallowing are severely impaired.4
- Chronic diarrhoea.
Intra/extracellular shift
- Following treated diabetic ketoacidosis (DKA): the shift in glucose following DKA treatment can result in hypophosphataemia.
- Rapid uptake of phosphate: this can occur in acute leukaemia, but more often is seen following parathyroidectomy for primary hyperparathyroidism. The sudden drop in PTH results in an influx of calcium and phosphate into bones. It can persist for several months following surgery, and is informally known as ‘hungry bone syndrome’.7
- Hyperinsulinaemia.
Other metabolic causes
- Hypothyroidism.
- Hypokalaemia.
- Hyperparathyroidism (primary and secondary).
- Vitamin D deficiency.
- Hypercalcaemia.
Consequences and management

Mild hypophosphataemia (0.6-0.8 mmol/L) is usually asymptomatic. Chronic hypophosphataemia below 0.6 mmol/L may still be asymptomatic, but muscle weakness, myalgia, bone pain and changes to mental status (e.g. confusion) can be seen. At this level, phosphate replacement is warranted, ensuring that the person also has adequate calcium and vitamin D stores. The dose is 4-6 effervescent tablets per day, although a lower dosage may be needed if diarrhoea occurs.9 Replacement should usually be adequate after 7-10 days.10 Alongside replacement, assess for potential causes, recognising that phosphate replacement can affect the PTH-calcium-vitamin D axis, so investigative bloods may need to be done early.
Symptomatic hypophosphataemia usually occurs when phosphate levels are below 0.32 mmol/L,11 and if this occurs acutely, intravenous replacement may be indicated. Severe hypophosphataemia can cause multi-organ cellular dysfunction and impaired energy metabolism. Examples of life-threatening consequences include acute respiratory failure, acute heart failure, arrhythmias, rhabdomyolysis, encephalopathy and seizures.
Mild to moderately low levels do not need urgent input, and time can be taken to ascertain whether they are pathologically low or confounded by any of the factors already mentioned. Repeating the test fasting may be useful, along with considering any recent hospital admissions (severe illness, diabetic ketoacidosis and parathyroidectomy can all result in hypophosphataemia), and reviewing any regular medications to see if they may be contributing to the findings. If not already available, consider checking calcium, urea and electrolytes, vitamin D, PTH and thyroid function tests.
If otherwise asymptomatic and not severe, simple monitoring is all that is needed.5
References
1. RL Wadsworth, S Siddiqui, Phosphate homeostasis in critical care, BJA Education, Volume 16, Issue 9, September 2016, Pages 305–309.
2. Goretti Penido M, Alon US. Phosphate homeostasis and its role in bone health. Pediatr Nephrol. 2012 Nov;27(11):2039-2048.
3. Ureña Torres PA, De Brauwere DP. Three feedback loops precisely regulating serum phosphate concentration. Kidney International. 2011; Volume 80, Issue 5, 443 – 445.
4. National Institutes of Health. Phosphorous: Fact Sheet for Health Professionals. 2023. [accessed 29 November 2024].
5. Glendenning P, Bell D, Clifton-Bligh R. Investigating hypophosphataemia. BMJ 2014;348:g3172.
6. Exeter Clinical Laboratory International. Phosphate. 2019. [accessed 29 November 2024].
7. Witteveen JE, van Thiel S, Romijn JA et al. THERAPY OF ENDOCRINE DISEASE: Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. European Journal of Endocrinology. 2013; Volume 168, Issue 3 Pages R45–R53.
8. Bosman A, Campos-Obando N, de Keyser C et al. Diuretic Use and Serum Phosphate: Rotterdam Study and UK Biobank. Journal of the Endocrine Society. 2024; Volume 8, Issue 5, bvae057.
9. British National Formulary. Phosphate. 2024. [accessed 29 November 2024].
10. Pappoe LK, Singh A. Hypophosphatemia. Editor(s): Stuart B. Mushlin, Harry L. Greene. Decision Making in Medicine (Third Edition). Mosby. 2010. Pages 392-393.
11. Gaasbeek A, Meinders AE. Hypophosphatemia: an update on its etiology and treatment. Am J Med 2005; 118: 1094–101.