_ RCGP Learning
Blog entry by _ RCGP Learning
Children with life-limiting conditions face significant challenges when they transition from paediatric to adult care. The transition involves many changes: the young person will transfer to adult specialities, to adult social care, and will experience changes in educational provision and legal changes involving parental responsibility for medical decision making.
The transition has been described as a ‘cliff-edge’ event, during which children and their families face significant stress, challenges, and unmet needs. When general practice is already aware of such a patient within their practice, a good service is already provided in many cases, but often young people with these conditions are not always visible, as the majority of their care is provided by paediatrics. Many of these young patients who thus far have had long term continuity of care from their paediatricians feel nervous or have little confidence in general practice and their ability to meet their complex needs. In some cases this can lead to ‘fire-fighting’, where general practice has to respond to crisis calls from young people (or their carers) with whom they may have had limited contact.
Recently, a small team at the RCGP – together with their colleagues from ‘Together for Short Lives’, produced an eLearning course on how the whole primary care team can contribute towards a good health transition from paediatric to adult care. These modules are for all primary care clinicians who want to provide excellent care for a young person with a chronic and/or life-limiting condition who is transitioning from paediatric to adult care. The modules are based on the insights generated by a pilot project which involved a steering group inclusive of general practice, palliative care, paediatricians, academics, and ‘Together for Short Lives’. Written by Dr Mike Miller, a paediatric palliative consultant with first hand experience of the pitfalls during transition and Dr Peter Lindsay, a GP with a special interest in paediatrics, the course combines the latest academic insights on health transition and the experiences of the authors and the steering group team.
During the pilot project, we recognised that there is overlap between young people with chronic and/or life-limiting conditions and young people with learning disabilities, and although the groups are distinct, there are similarities in their transition process. In many areas, local transition services for young people with complex needs are evolving rapidly: Leeds have developed an evolving transition network, and so far involves ongoing collaborations between education, the local children's hospice, social care, mental health services and learning disability leads.
As part of the pilot project, we performed initial searches within our practices for patients within these categories, and are now trying to develop processes to support transition. The pilot project highlighted the positive impact we can have in supporting the young person and family at a challenging and stressful time, and how we can improve health and social outcomes. As well as the routine care offered, general practice is uniquely placed to offer continuity of care through the transition period, early preparation for the transition to adult service, social prescribing and the help of the whole primary care team. Primary care is also perfectly placed to address health needs that often go under-recognised in this group, such as sexual health and contraception. If we can develop mechanisms to reliably identify these patients, then young people with chronic and/or limiting conditions will benefit from all that primary care can offer.
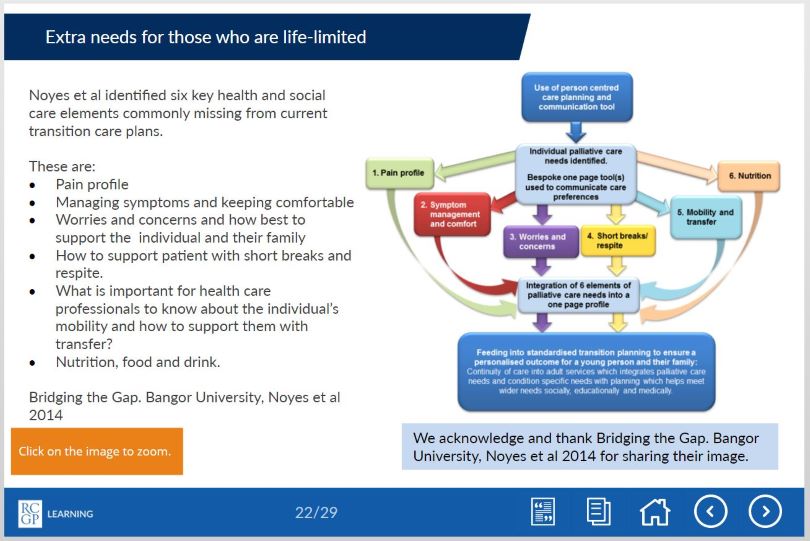
The eLearning modules firstly outline the challenges facing young people and their families during the transition period, from the perspective of a paediatric palliative care consultant who has devoted much of his career to improving the experience of young people and their families at transition. Secondly, poorly understood areas are tackled, such as the legal framework underpinning mental capacity at transition, and the practical implications of this for the young person and family. The second module presents practical approaches and best practice to support this area in a GP setting, in the current challenging and busy context of general practice. Please see below for some tasters from the eLearning modules.
Please also see the Developing Positive Transitions for Primary Care resources section, which signposts to further key information.
If you would like to learn more please see our eLearning modules and further learning resources:
'Better transitions: improving young people’s transfer from paediatric to adult services' eLearning course: https://elearning.rcgp.org.uk/bettertransitions
'Developing Positive Transitions for Primary Care' resources page: https://elearning.rcgp.org.uk/course/info.php?id=329